There is current debate about the appropriateness of applying diagnostic nosology to preschool children
(1). The validity of interviews based on DSM specifically has been questioned because the reported rates of disorders diagnosed on the basis of this methodology appear to be high
(2). These are appropriate critiques that are best addressed by examining empirically derived data. In this paper, we address one specific aspect of this debate: whether DSM-IV disruptive behavior symptoms overidentify preschool children as disordered.
Since noncompliance and aggression are more common in early childhood than other developmental periods
(3), it is possible that the operational definitions of the symptoms of oppositional defiant and conduct disorders reflect behaviors that are normative for preschool children. Consequently, caregivers may positively endorse these symptoms even when the behavior is not atypical or impairing. This would pose a serious threat to the validity of DSM symptoms for this population.
To date, most studies of preschool disruptive behavior disorders have relied on clinically referred samples
(4–
6) or, when nonreferred samples are included, have not reported rates of oppositional defiant and conduct disorder symptoms and disorders for the nonreferred children
(7–
9). Thus, the rates of oppositional defiant and conduct disorder symptoms in typically developing preschoolers are not known. This gap in knowledge precludes our ability to address the concern that the reported rates of oppositional defiant and conduct disorders in preschool children are inflated because of symptom definitions that pathologize normative behavior in young children.
In this study we test the discriminative validity of oppositional defiant and conduct disorders by comparing rates of symptoms of these disorders between preschoolers referred for disruptive behavior problems and preschoolers who were not referred. To our knowledge, this is the first study in which rates of DSM-IV symptoms of oppositional defiant and conduct disorders among referred and nonreferred preschoolers are compared.
Method
Participants were consecutive referrals to the Preschool Behavior Problems Clinic for aggression, temper tantrums, or noncompliance and a comparison group of 50 nonreferred children from a pediatric clinic. Of the 86 consecutive referrals, seven were excluded: four had an IQ below 70, two families had incomes in the upper-middle income range, and one mother refused to participate in the research project. The resulting number of referred children was 79. Written informed consent was obtained from all participating mothers after the procedures had been fully explained. All participants were between the ages of 2.5 and 5.5 years and resided with their biological mothers. Mothers who volunteered to be in the comparison sample and then reported during the initial phone screen that they were concerned about their children’s behavior or that the child had been referred for mental health services were referred to the Preschool Behavior Problems Clinic.
The groups were matched on demographic characteristics and developmental level. The mean age was 48 months (SD=8.9) for referred and 47 months (SD=10.1) for nonreferred children. The majority of the children were boys (75% [N=59] of the referred and 70% [N=35] of the nonreferred children) and African American (82% [N=65] of the referred and 98% [N=49] of the nonreferred children), and the majority of the families were welfare recipients (84% [N=66] of the referred and 94% [N=47] of the nonreferred children). The average general cognitive ability score was 84.4 (SD=12.5) among referred children and 86.4 (SD=11.5) among nonreferred children.
DSM-IV symptoms of oppositional defiant and conduct disorders were assessed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E)
(10), a semistructured diagnostic interview. One of the clinicians administering the K-SADS-E to the biological mothers was a child psychiatrist; all of the other clinicians administering the interview were advanced clinical psychology students who held at least a master’s degree.
Some developmental modifications to the interview were made (see reference
11 for details) for the purpose of providing developmentally appropriate operational definitions or for eliminating symptoms that lacked face validity. For example, for stealing, we did not require the item to be of nontrivial value, as stated in DSM-IV, since preschool children would not usually attempt to take larger and more expensive items. Use of a weapon could include using a stick, rock, or bat. For the symptom of often loses temper, a child needed to have persistent, frequent tantrums (i.e., several times a day) from which recovery was slow. For the symptom of difficulty paying attention, we used examples such as being able to pay attention to a story being read. The symptoms of curfew violation, truancy, and running away were not included because of insufficient face validity. Symptom and duration criteria were applied as stated in DSM-IV. Kappa coefficients were 1.0 for conduct disorder and 0.74 for oppositional defiant disorder. Fisher’s exact tests were used to test for significant differences between the referred and nonreferred children.
Results
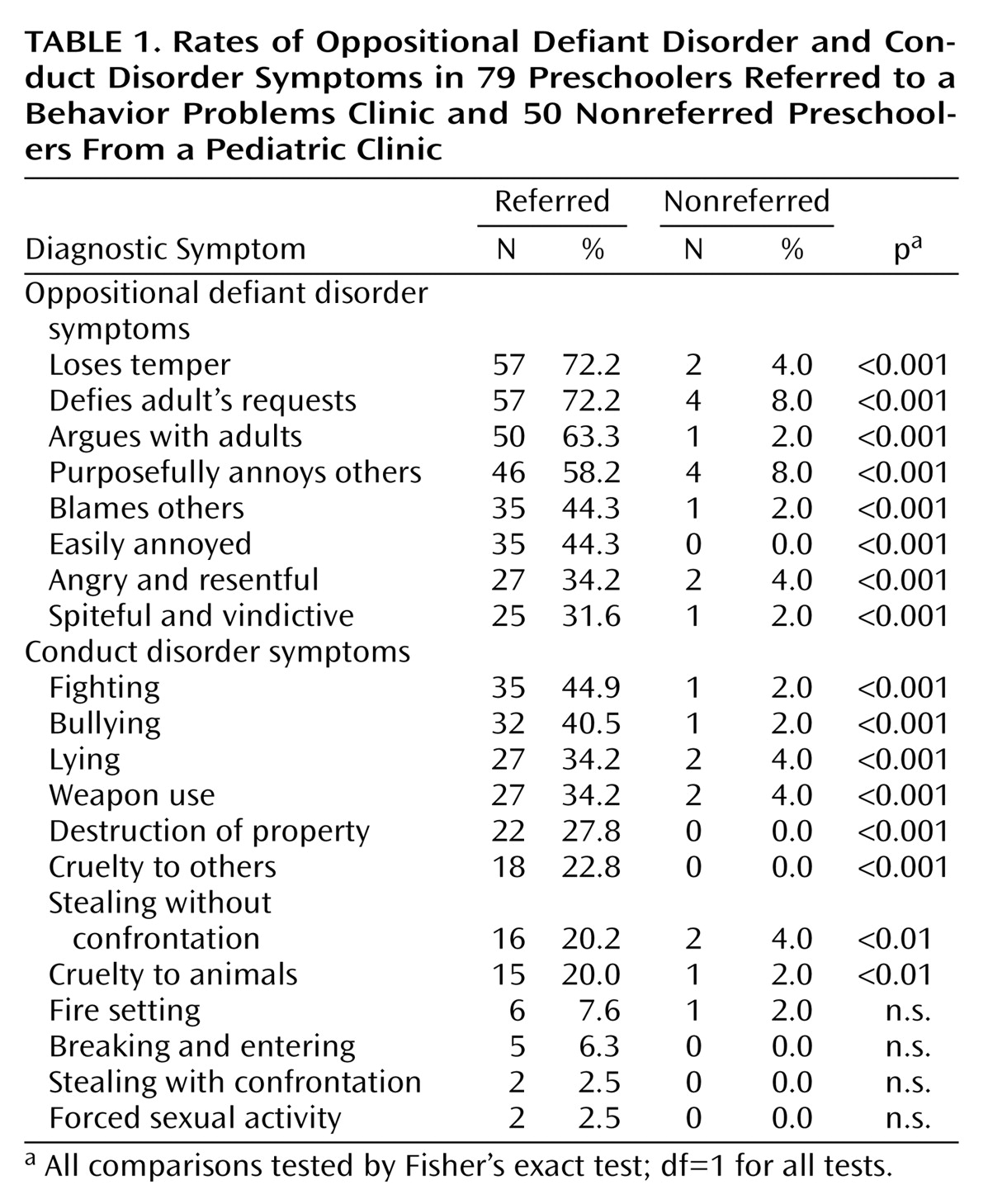
Rates for symptoms of oppositional defiant and conduct disorders for the clinically referred and nonreferred preschoolers are presented in
Table 1. Rates of oppositional defiant disorder symptoms were significantly higher in referred than nonreferred preschoolers. The base rate of oppositional defiant disorder symptoms ranged from 0.0% to 8.0% in the nonreferred children (all but two symptoms had a base rate below 5.0%), whereas rates ranged from a low of 31.6% to a high of 72.2% among the referred children (
Table 1). Only one nonreferred child (2.0%) met criteria for oppositional defiant disorder, compared with 47 (59.5%) of the referred children.
The majority of the comparisons of rates of conduct disorder symptoms yielded significantly higher rates among referred preschoolers than nonreferred children; base rates were below 5.0% for all conduct disorder symptoms among the nonreferred children. Four symptoms for which base rates were below 8.0% for both groups of children did not demonstrate discriminative validity: fire setting, breaking and entering, stealing with confrontation, and forced sexual activity. Only five of the nonreferred preschoolers were reported to have any symptoms of conduct disorder, and one nonreferred child met criteria for conduct disorder (the same child who met criteria for oppositional defiant disorder), compared with 33 (41.8%) of the referred children.
Discussion
Our results provide preliminary evidence for the discriminative validity of DSM-IV oppositional defiant and conduct disorder symptoms in preschool children. Both oppositional defiant and conduct disorder symptoms were rare among nonreferred preschool children, and the rate of these disorders was 2%, which is slightly lower than the rate reported among older children from similar environments
(12). In contrast, oppositional defiant disorder symptoms were commonly endorsed among the clinically referred preschoolers, and a substantial minority endorsed conduct disorder symptoms. To our knowledge, this is the first report in which data are presented on rates of oppositional defiant and conduct disorder symptoms in referred and nonreferred preschool children. Testing the discriminative validity of these symptoms is one critical aspect for determining whether DSM-IV can be used validly in preschool children.
One could argue that in making developmental modifications to the assessment of oppositional defiant and conduct disorder symptoms, such as not requiring stolen objects to be of nontrivial value or defining weapons as sticks, rocks, or bats, results in defining a disorder with such commonly occurring behaviors that many preschool children would be diagnosed inappropriately. This does not appear to be the case. Although the functional equivalence of the operational definitions in the present study to those validated as symptoms in older children remains to be established, the symptom definitions are clinically discriminative.
The results presented here can be generalized to African American children living in urban poverty, a group of children who have often been underrepresented in the literature on diagnostic validity. Replication of our findings in larger and more diverse samples will allow for testing the diagnostic validity across age, gender, ethnicity, and socioeconomic status. Clearly, the validity of DSM-IV oppositional defiant and conduct disorders in preschoolers requires additional tests, including predictive validity. In addition, the utility of the developmental modifications used in the present study was not systematically assessed. A comparison of the validity of disruptive behavior symptoms in preschoolers generated by well-operationalized methods is a critical next step to identifying a developmentally appropriate diagnostic nosology for disruptive behavior disorders in preschool children.