Long-term psychoanalytically oriented treatment for severe personality disorders often entailed admission to a residential facility offering milieu therapy in the context of a therapeutic community
(1). These units offered a combination of intensive individual and group psychoanalytic psychotherapy and a vigorous program of social rehabilitation
(2). This approach, while costly, held promise in light of the pervasive developmental deficits of this group of patients that undermined their capacity to function effectively in interpersonal relationships. In the last two decades, the development of the diagnosis and understanding of severe personality disorders
(3) along with alternatives to hospitalization, improvements in the biological approach to severe personality disorders
(4), and cost-related considerations have resulted in a clear move away from residential treatment of personality disorders.
The evaluation of long-term residential psychotherapeutic treatment for severe personality disorders rests on a few cohort studies, which were limited by methodological problems such as a retrospective design, diagnostic criteria not being operationalized, lack of a comparison or control condition, and unstandardized outcome measures
(5,
6). At the same time, a handful of studies have produced evidence that outpatient programs based on cognitive behavior or psychodynamic approaches are quite effective, particularly in the treatment of borderline personality disorder
(7,
8). None of these alternatives provide the remedial compensatory environmental experience offered by the therapeutic community milieu. Since therapeutic community-based treatment has never been evaluated relative to these less intensive community-based treatments, there might be a risk that psychiatry will lose a possibly effective treatment modality without it ever having been properly evaluated.
Here we report a comprehensive outcome comparison for two models of delivering psychotherapeutic inpatient treatment: a long-term residential psychosocial treatment approach and a “step-down” model with a shorter-term inpatient stay followed by longer-term outpatient and community treatment. Both of these models were compared with general psychiatric community treatment on its own without the benefit of inpatient or outpatient specialist psychotherapeutic treatment.
Method
The study took place at The Cassel Hospital and North Devon Healthcare NHS Trust, England.
All patients consecutively admitted to The Cassel Hospital for specialist psychosocial treatment between 1993 and 1997 were considered for the study. Inclusion criteria were ages between 19 and 55, IQ above 80, and meeting diagnostic criteria for at least one personality disorder. Exclusion criteria were a diagnosis of schizophrenia, paranoid psychosis, or drug or alcohol addiction (but not misuse) as well as mental impairment and evidence of organic brain disorder.
Seventy-nine patients were allocated to the purely inpatient program, which consisted of an expected 12-month admission with no planned outpatient follow-up. Fifty-eight patients were assigned to the step-down program, which consisted of an expected 6-month admission followed by 12–18 months of outpatient group analytic psychotherapy and 6–9 months of concurrent outreach nursing. The treatment allocation followed established criteria of geographical accessibility to treatment, whereby patients outside the Greater London area were assigned to the inpatient program.
Of the 79 patients considered for the inpatient program, two (3%) did not meet criteria, and an additional 28 (35%) either refused consent or dropped out of the study immediately after signing consent forms and having contributed no data or after only completing the intake battery of measures. One patient (2%) of those considered for the step-down program did not meet criteria, and 12 patients (21%) either refused to give written consent or refused to cooperate with the study from the outset. Of the four successful suicides in the inpatient program group, two did not complete the baseline assessment, while the other two killed themselves by 6 and 12 months after admission, respectively. For these patients in the data analysis we carried over the values of the standardized measures from the last assessment point, and they were thus included in the multivariate analysis. However, they were excluded from the analysis of clinical outcome variables, since we found no satisfactory way of estimating these data.
The components of the residential treatment were 1) twice-weekly individual psychoanalytically oriented psychotherapy; 2) meetings with unit staff five times a week; 3) twice-weekly community meetings; 4) once-weekly small group psychotherapy; 5) a structured program of activities aimed at the acquisitions of interpersonal skills, resocialization, and rehabilitation; 6) and psychotropic medication. Patients were reviewed formally every 2 months.
The outpatient stage for the step-down program comprised 1) twice-weekly small group analytic psychotherapy; 2) twice-weekly individual and group meetings in the community with a psychosocially trained outreach nurse; 3) active networking with primary and secondary care workers; 4) team meetings to discuss patients’ progress; and 5) meetings with a senior psychiatrist to review progress.
The general psychiatric comparison group, selected from the caseload of all the senior district clinicians during the same period in North Devon, England, comprised 130 patients 19–55 years of age who were identified as suffering from a primary personality disorder diagnosis. These patients were screened with the Personality Diagnostic Questionnaire
(9), which confirmed the presence of at least one axis II diagnosis in 73 patients. Fourteen (19%) of these did not wish to participate in the study, and an additional 10 (14%) could not be regularly followed up. Fifty-seven percent had been inpatients in the previous year, and all had a history of hospitalization. Inclusion and exclusion criteria were the same as those used for the specialist treatment samples. Patients received standard general psychiatric care, which included 1) psychotropic medication; 2) supportive outpatient and community contact with one or more care workers, on average at intervals of 2–4 weeks; 3) hospital admission as needed; and 4) a clinical review on average once a month. This group would meaningfully reflect the outcome of expectable nonspecialist treatment in the United Kingdom.
After complete description of the study to all eligible patients, written informed consent was obtained.
The final study sample included 49 patients (62% of eligible) in the inpatient program, 45 (78%) in the step-down program, and 49 (67%) in the general psychiatric comparison group. All consenting patients were assessed for presence of axis I and II diagnoses by using the Structured Clinical Interview for DSM-III-R (SCID) and the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II)
(10), and thorough demographic and clinical history was obtained, recorded, and coded. Interrater reliability testing with a second psychiatrist reviewing taped interviews showed that kappa values calculated for each axis I diagnosis yielded a median kappa of 0.85 (range=0.73–1.00). Reliability of axis II diagnoses varied between 0.61 for Cluster A, 0.67 for Cluster B, and 1.00 for Cluster C disorders. Intelligence quotient equivalents were obtained through administration of the National Adult Reading Test
(11).
The median duration of inpatient stay was 42 weeks (mean=36, SD=19.0) and 28 weeks (mean=27, SD=6.9) for the inpatient program and step-down program patients, respectively. The median duration of outpatient treatment for the step-down program was 57 weeks (mean=44, SD=29.7). Since this was an intent-to-treat study, clinical dropouts were recalled for assessment at the agreed schedule. At the time of the 24-month assessment, all but three patients (6.7%) in the step-down program group who had their therapy extended for clinical reasons had terminated their specialist treatment program. However, because of their better compliance and longer duration of treatment, most patients in the step-down program had been discharged from treatment only 3 months before the 24-month assessment, compared with 14 months for patients in the inpatient program. The data were analyzed excluding program noncompleters, and no substantial difference in the pattern of outcomes on key variables was found.
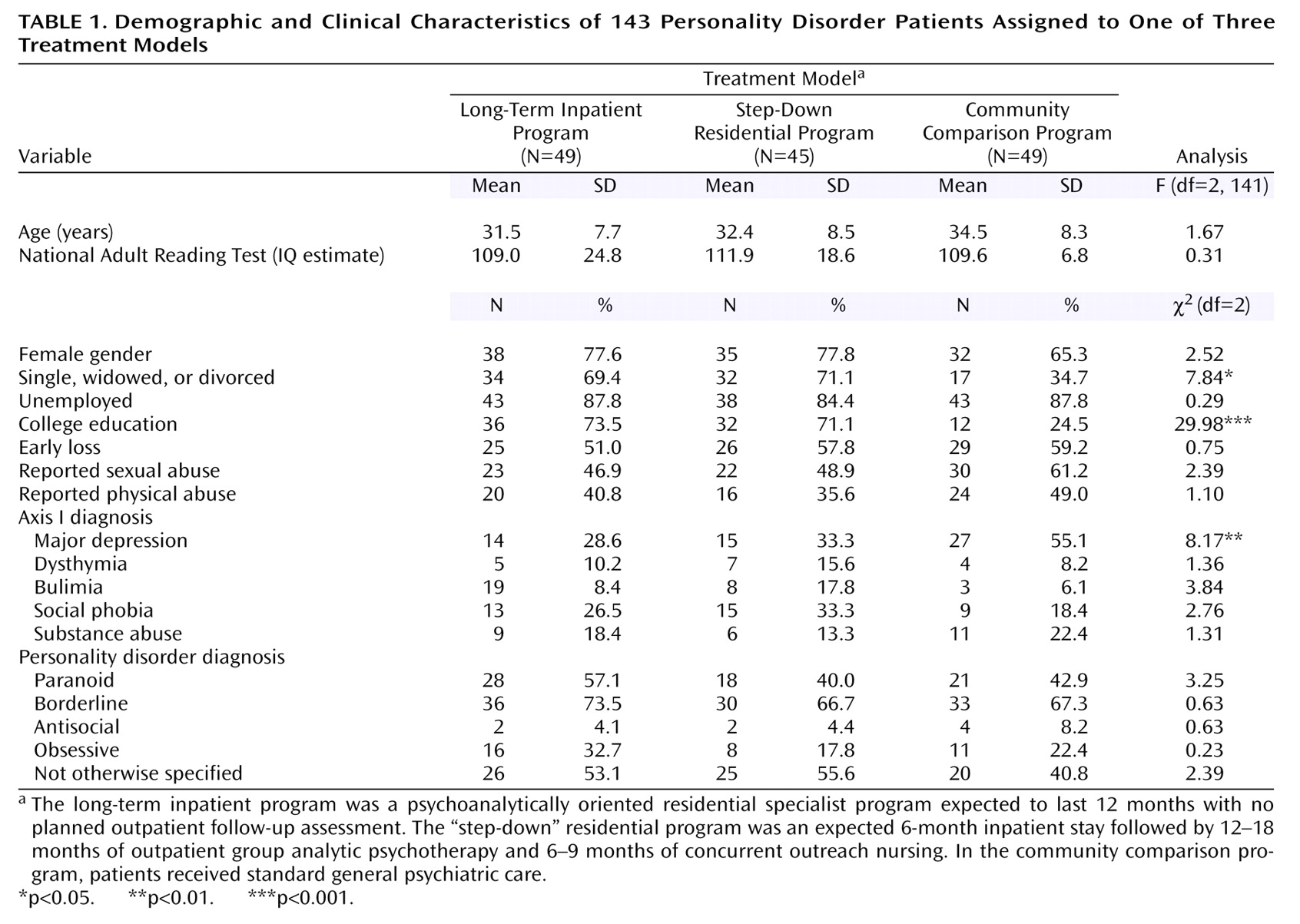
Demographic and clinical characteristics of the patients in the three treatment groups are shown in
Table 1. The three groups were well matched, but significant differences were found in terms of marital status, education, and major depression status. The general psychiatric comparison group had a higher proportion of patients who 1) were in a stable relationship, 2) had no college education, and 3) met criteria for current major depression. Most patients (70%) met criteria for more than two personality disorders, while 83% had a concurrent axis I diagnosis. No significant group differences were found in terms of personality disorder comorbidity or axis I/axis II comorbidity.
Measures of Outcome
Psychiatric symptoms and social adaptation
The SCL-90-R
(12) was used to measure the patients’ subjective experience of symptoms on a 5-point scale. The general severity index and positive symptom scores were used to report changes in this dimension. Interview-based measures were administered by a team of independent researchers trained to reliability criteria on all measures. A subset of 35 interviews was taped and independently coded by a senior psychiatrist blind to group allocation. The interviewer-based version of the Social Adjustment Scale
(13) provides an assessment on a 5-point scale of adjustment in the area of work, family of origin, marriage, sexual functioning, and leisure activities. A total social adjustment score is derived from the means of the subcategories. An interclass correlation coefficient (ICC) of 0.78 obtained for the total score showed a satisfactory interrater agreement. The Global Assessment Scale
(14) was used to evaluate patients’ general outcome in accordance with their level of functioning assessed during the 4 weeks before the assessment. Good interrater reliability was found (ICC=0.79). All the measures were applied at intake, 6 months, 12 months, and 24 months.
Clinical measures
A structured interview, modeled on the Suicide and Self-Harm Inventory
(15), was applied at intake, 12 months, and 24 months to obtain details of self-harm episodes, number and length of psychiatric inpatient episodes, and psychiatric outpatient attendance over the year before the assessment. Each variable was operationally defined, and the interviewer was required to write details that would be checked for accuracy by a senior psychiatrist (M.C.). A random sample of the clinical variables was crosschecked against the records of the patients’ general practitioners, who receive details of all medical and psychiatric procedures concerning their patients.
Statistical Analysis
All analyses were carried out in SPSS for Windows, version 9 (Chicago, SPSS, Inc.). The multivariate analog of the analysis of covariance (ANCOVA) for repeated measures was applied to the interval data from all the main standardized measures separately, with education, marital status, and mood disorder as covariates, one repeated-measure factor (time), and a between-subjects factor (group). Nonsignificant covariates were dropped from the model, and the analysis was repeated. Bonferroni tests of adjustments were used in pairwise contrasts to correct for risk of type I errors. Two clinical outcome variables and one service utilization variable were dichotomized as present/absent at intake, 12 months, and 24 months. Differences between groups at 12 or 24 months were examined using hierarchical logistic regressions on dichotomized clinical variables, with dichotomized group memberships as predictors and baseline status on the clinical variable and the demographic and mood disorder variables as covariates. The presence or absence of self-mutilation or suicide attempts or acute psychiatric admission was predicted at 12 and 24 months in separate analyses using self-mutilation or suicidality or psychiatric inpatient status at intake and group membership as binary categorical predictor variables.
Outcome was also evaluated as a categorical variable. Using the formula provided by Jacobson and Truax
(16), we calculated a cutoff point for each standardized measure that defined the boundary of “clinically relevant change” in each group. A variable for SCL-90-R, Social Adjustment Scale, and Global Assessment Scale was computed showing the number of improved patients at each of the assessment points. Nonparametric tests were then performed to test the difference among the three groups.
Results
Psychiatric Symptoms, Social Adjustment, and Global Assessment of Functioning
The multivariate analog of the repeated-measures analysis of covariance, with education and mood disorder status as the significant covariates included in the model, applied to the means of the SCL-90-R general severity index revealed a significant time effect (Wilks’s lambda=0.82; F=9.77, df=3, 136, p<0.001) and a significant group-by-time interaction (Wilks’s lambda=0.84; F=4.31, df=6, 272, p<0.001).
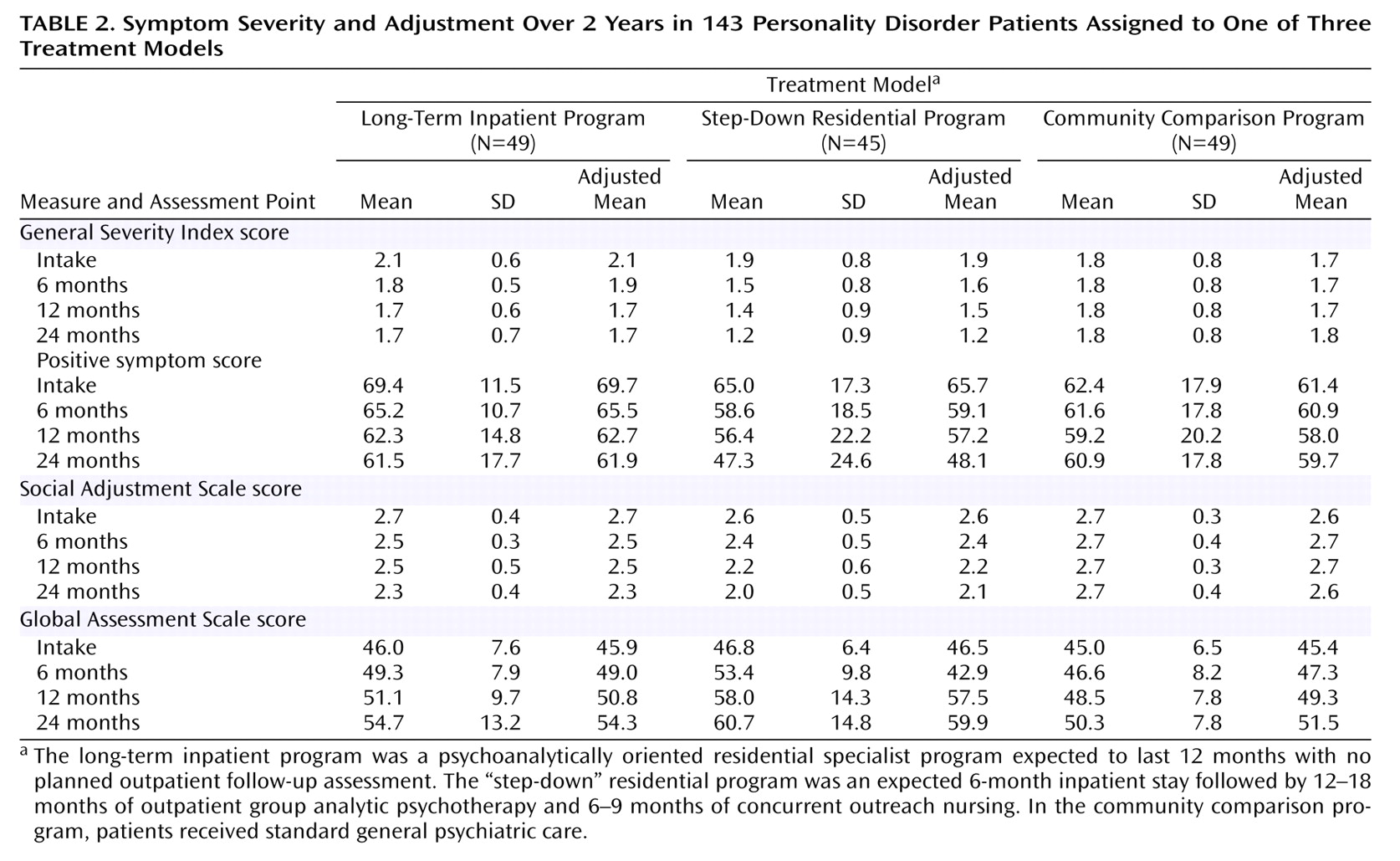
After we controlled for mood disorder, a significant effect of time (Wilks’s lambda=0.89; F=5.69, df=3, 137, p<0.001) and a significant group-by-time interaction (Wilks’s lambda=0.85; F=3.74, df=6, 274, p<0.001) were found for positive symptom total scores. The means displayed in
Table 2 indicate that both symptom severity and number of symptoms reported decreased significantly more sharply in the step-down program patients relative to lower or lack of changes in the other two groups.
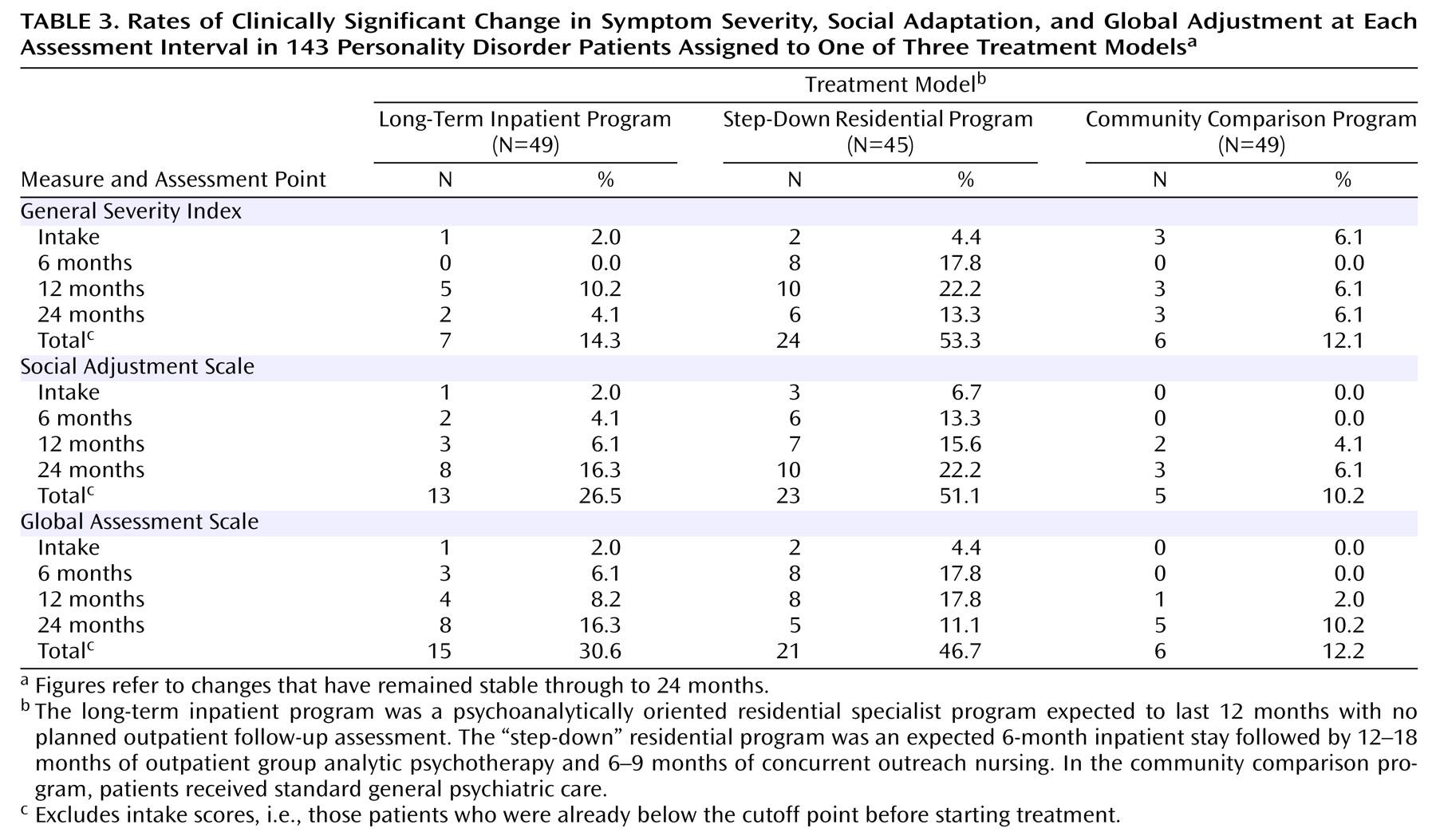
Table 3 displays the rates of clinically significant improvement in the three groups over time. It shows that a total of 24 patients (53%) in the step-down group scored below the cutoff point for symptom severity (the criterion for a clinically relevant change) by 24 months, compared with only seven (14%) and six (12%) in the inpatient and community psychiatric groups, respectively. The difference was highly significant (χ
2=23.93, df=2, p<0.001).
Improvement in social adaptation as shown in total Social Adjustment Scale score was more marked in the two Cassel Hospital groups than in the general psychiatric group (
Table 2). After we controlled for marital status and mood disorder, we found a highly significant effect of time (Wilks’s lambda=0.83; F=9.37, df=3, 136, p<0.001) and a significant interaction between group and time factors (Wilks’s lambda=0.85; F=3.92, df=6, 272, p<0.001). The difference between groups in number of patients who reached clinically significant improvement in social adaptation was significant (χ
2=26.62, df=2, p<0.001). Only five patients (10%) in total in the general psychiatric group were improved according to criteria by 24 months compared with 13 (27%) in the inpatient group and 23 (51%) in the step-down group.
Results of the global assessment of mental health measure showed that patients in the step-down condition achieved most marked improvements relative to the other two groups. The ANCOVA revealed a significant time factor (Wilks’s lambda=0.66; F=23.42, df=3, 137, p<0.001) and a significant group-by-time interaction (Wilks’s lambda=0.91; F=2.24, df=6, 274, p<0.05) after we controlled for mood disorder. By 24 months, a total of 21 patients (47%) in the step-down group achieved a clinically significant increase in global assessment of mental health score, compared with 15 patients (31%) in the inpatient group and six patients in the general psychiatric condition (χ2=19.98, df=2, p<0.001).
Clinical and Service Utilization Outcomes
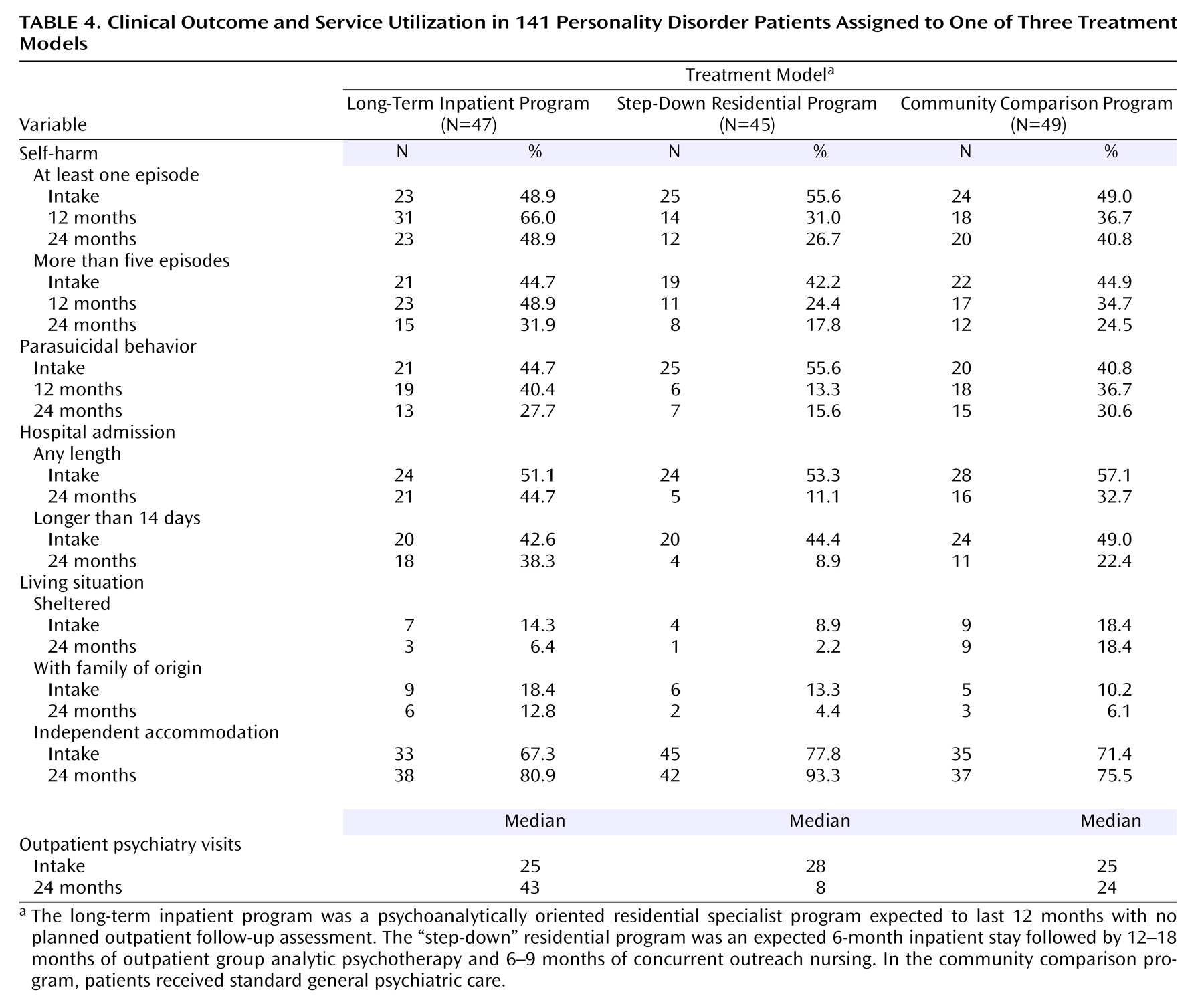
Table 4 shows figures concerning clinical outcomes in the three groups at the different assessment points.
The number of patients who engaged in at least one episode of self-mutilation decreased markedly by 12 and 24 months in the step-down sample, whereas it increased at 12 months in the inpatient group and marginally decreased in the general psychiatric group by 24 months. The hierarchical logistic regression showed that the model including self-mutilation the year before intake and group status was predictive of self-mutilation at 12 months (χ2=60.48, df=3, p<0.001), with membership in the inpatient program contributing to the prediction (B=1.91 [SE=0.59], df=1, p<0.002). Similarly, predicting self-mutilation at 24 months from the covariates and group membership yielded a highly significant model (χ2=45.07, df=3, p<0.001). We found that membership in the step-down group was a significant parameter in the model (B=–1.03 [SE=0.52], df=1, p<0.05). The odds ratios revealed that patients in the step-down program were three times less likely to self-mutilate by 24 months (CI=1.01–7.69), while membership in the inpatient program group predicted a 1.5 increase in self-mutilation (CI=0.59–4.14). If we consider the number of self-mutilating episodes and divide the samples into no self-mutilation, occasional (1 to 5), and frequent (>5) episodes for each group separately, significant reduction relative to baseline was only found in the step-down patients by 12 months (Kendall’s W=0.22; χ2=9.94, df=1, p<0.003). By 24 months, a significant decrease was seen in both the step-down group (Kendall’s W=0.31; χ2=13.76, df=1, p<0.001) and the general psychiatric group (Kendall’s W=0.82; χ2=4.00, df=1, p<0.05) but not the long-term inpatient specialist group (Kendall’s W=0.01; χ2=0.29, df=1, p=0.59).
The models that included suicide attempts the year before intake, group status, and attempted suicide as the dependent variables were also highly significant at 12 and 24 months (χ2=31.54, df=3, p<0.001, and χ2=17.05, df=3, p<0.001, respectively). Membership in the step-down program was revealed to be a significant parameter in the model both at 12 months (B=–1.80 [SE=0.58], df=1, p<0.002) and at 24 months (B=–1.19 [SE=0.55], df=1, p<0.04). Patients in the step-down program were six times (CI=18.87–1.95) and three times (CI=9.61–1.12) less likely to attempt suicide by 12 and 24 months, respectively.
In the year after expected discharge patients in the step-down program were 4 times less likely to be readmitted to a psychiatric service (CI=12.50–1.32). The logistic regression confirmed that this group was significantly different from the other two groups (B=–1.42 [SE=0.59], df=1, p<0.002). Only five patients (11%) in the step-down program required inpatient treatment compared with 21 (45%) and 16 (33%) of the patients belonging to the inpatient and general psychiatric groups, respectively. Length of inpatient episodes expressed as a trichotomous variable (no days, up to 14 days, above 14 days) showed that decrease in length of stay by 24 months for each group separately was highly significant for the step-down patients (Kendall’s W=0.44; χ2=20.00, df=1, p<0.001) and for the general psychiatric sample (Kendall’s W=0.18; χ2=8.91, df=1, p<0.005), but not for the inpatient sample (Kendall’s W=0.011; χ2=0.53, df=1, p=0.47).
With regard to living situation, by 24 months patients in the two specialist groups achieved a shift toward more independent accommodation status, whereas no change was recorded in the general psychiatric group. The difference between the groups was again significant (χ2=10.49, df=4, p<0.04).
Significant group differences were also revealed in the number of outpatient (including day patient) psychiatric consultations by 24 months (χ2=16.84, df=2, p<0.001). Patients in the step-down program achieved significant reductions from baseline (Wilcoxon’s z=–2.85, p<0.005), whereas subjects in the inpatient specialist program and in the general psychiatric group maintained similar or higher levels of outpatient utilization (Wilcoxon’s z=1.09, p=0.28 and Wilcoxon’s z=–0.62, p=0.54, respectively).
Discussion
We would like first to comment on the limitations of the study. Since the allocation to the study groups was not the result of randomization, the issue of the comparability of the groups needs to be addressed. It is likely that the hospitalized and comparison groups differed at referral for different kinds of treatment and that further bias may be introduced when compared groups are referred from different geographical areas of the country even for the same kind of treatment. The confounding of type of treatment with participant characteristics could be a significant threat to the internal validity of the study. To mitigate this risk we found that the groups were relatively well matched on most demographic, diagnostic, and other clinical criteria, including severity, that were measured. Controlling for the three variables that were significantly different did not affect the observed differences in outcome. The two treatment samples comprised patients referred specifically for specialist psychotherapeutic treatment, so it could be argued that they were selected on the basis of their potential for responsiveness to such approach. In reality the strict funding arrangements introduced in the United Kingdom in 1993 (when recruitment for this study commenced) meant that only “meritorious” patients in terms of severity and chronicity of disturbance were funded for treatment at tertiary care centers such as the hospital under investigation.
The multicomponent nature of the treatment programs under scrutiny complicates assessments of effectiveness due to the complexity of the intervention. It is not clear if mere hospitalization, the nature of the hospital climate, or the treatments offered in the hospital or a combination of these was the effective component of the treatment. The relatively inclusive selection criteria, in specifying a single personality disorder diagnosis as sufficient to qualify for entry into the study, might have led to a heterogeneous patient group. All three samples were largely (80% or more) made up of individuals with at least one cluster B personality disorder diagnosis, and the average participant met two to three sets of diagnostic criteria; the breadth of the original inclusion criteria did not turn out to be a problem. Further limitations of the study included the lack of raters’ blindness with regard to group allocation and assessment point and the asymmetrical follow-up period, which was inevitable given the unequal length of treatment and our intention to follow the natural course of the disorder.
Bearing in mind these limitations, the results showed that a step-down program comprising a medium-term residential stay in a psychosocial therapeutic milieu followed by long-term outpatient group psychotherapy and support in the external community achieved significantly greater improvement on a number of standardized and clinical outcome measures than long-term specialist residential treatment alone with no outpatient follow-up or general psychiatric management. The significant decrease in self-mutilating and parasuicidal behavior and in readmission rates along with a sustained improvement in symptom severity and social and global adjustment in the step-down group is an indication that continuing treatment in the community plays an important role in helping patients make the transition between hospital and community life. We suggest that providing a long-term outpatient specialist psychosocial aftercare program seems to protect patients from the anxieties connected with discharge from the hospital, which in turn enables them to better face the challenges of readapting to community life without breaking down
(17). The initial phase of hospitalization in a structured setting with multiple and intense therapeutic input may be an important component of the treatment of individuals with severe personality disorders to initiate a process of reversal of entrenched patterns of dysfunctional behavior, expressed as severe symptoms or self-destructive acting out. However, recent purely community-based approaches to the treatment of personality disorders may suggest that admission to a hospital milieu could be avoided with no detriment to effectiveness
(7,
8,
18). Hospital treatment for 6 months or 12 months is no longer regarded as realistic treatment options for the treatment of personality disorders in North America, as third-party payers regard the cost associated with inpatient admission as excessive. However, we have shown that the cost of specialist inpatient admission relative to that of treatment as usual reduces health and social care cost in the year after treatment termination, and if the savings are maintained the cost of treatment would be offset within 5 years for patients in the step-down program
(19). Thus, a long-term program that includes a 6-month inpatient stay might be in part justifiable in economic terms, at least in countries where socialized health care would require that these severely problematic individuals receive treatment.
In contrast, the findings concerning long-term specialist residential treatment were mixed. Compared with the general psychiatric group, the inpatient group did generally better in symptom reduction, social adaptation, and global outcome but showed comparable results in clinical and service utilization variables. When the planned length of hospitalization is excessive, this may carry risks in the shape of regressive and iatrogenic effects, as the results in self-harming and parasuicidal behavior confirmed. In addition, the lack of a planned outpatient follow-up treatment leaves patients to a state of continuing vulnerability to acute decompensations as shown by the unchanged rate of readmissions to psychiatric services in the year following expected discharge.
In conclusion, this study suggests that medium-term residential psychotherapeutic treatment as part of a long-term step-down program may be an important component for the effective treatment of severe personality disorders, while the role of long-term inpatient stay may need redefining. Further comparative studies that include a partial hospitalization program or a specialist outpatient program are needed to ascertain that a phase of specialist residential hospitalization is in fact necessary for achieving a better outcome with this group of patients.