Evidence from prospective birth cohort and high-risk studies has consistently shown that individuals who later go on to fulfill diagnostic criteria for schizophrenia in adulthood, as a group, achieve lower scores on intelligence tests in childhood and adolescence than their peers (1–11). Most of these studies have generally shown an inverse linear relationship between premorbid intellectual ability and later schizophrenia and provide among the strongest support for a neurodevelopmental etiologic model for schizophrenia (12). However, there are still some unanswered questions.
First, the exact nature of the premorbid intellectual deficit in schizophrenia was not explored in most of the previous studies. Second, it is not known whether impaired premorbid intellectual functioning is specific to schizophrenia. It has been suggested that impaired premorbid intellectual ability is shared with all functional psychoses (13, 14). Certainly other studies have shown that nonschizophrenic, nonaffective psychoses are also associated with impaired premorbid intellectual functioning (2, 8), but little is known about this aspect of bipolar disorder. To our knowledge, only three prospective studies have addressed this issue (7, 9, 15). An analysis of the Dunedin birth cohort showed that children with a later diagnosis of schizophreniform disorder in adulthood had impaired intellectual performance, whereas children later diagnosed with mania or anxiety/depression did not differ from comparison subjects on intellectual performance (7), although this particular finding was obtained from a relatively small number of subjects (N=20) in the mania group. An analysis of an Israeli cohort of male conscripts showed that subjects later diagnosed with schizophrenia had poorer intellectual performance at age 18, while subjects later diagnosed with nonpsychotic bipolar disorder did not differ from comparison subjects (9). However, this study excluded subjects with psychotic bipolar disorder and was thus not representative of all bipolar disorders. Recent results from a Swedish cohort of conscripts showed that a lower general intelligence score was associated with higher risks for schizophrenia, severe depression, and other nonaffective psychoses but not for bipolar disorder (15).
In the present study we aimed to investigate the premorbid intellectual functioning of individuals later diagnosed with bipolar disorder (both psychotic and nonpsychotic), schizophrenia, and other psychoses among a large cohort of Finnish conscripts. The high statistical power of this study allowed us to examine both the nature and linearity of any association found.
Method
Subjects
The study population comprised all Finnish male citizens born between 1962 and 1967 who served in the Finnish Defense Forces between 1982 and 1987. The annual size of the Finnish male birth cohort varied between 37,115 and 38,925 (total, 227,543), during the years 1962–1967, and the total number of subjects included in this study was 195,019 (86% of the birth cohort; the remaining 14% of the cohort subjects did not begin their military service in due time because of ethical or religious convictions, a deferment on the basis of current work or study, or a severe medical condition, such as asthma or diabetes). Permission for the study was obtained from the Ministry of Health and Social Affairs, the Headquarters of the Finnish Defense Forces, and the Ethics Committee of the National Public Health Institute.
Assessment of Intellectual Ability at Conscription
The ability test scores used in the present study were obtained from the Finnish Defense Forces Basic Ability Test, which was developed at the Finnish Defense Forces Education Development Center. The obligatory test is given to all new recruits during the 2 first weeks of their military service. The results of the examination are used when the conscripts are selected for leadership training during their military service. The mean age of the subjects at the time they took the ability test was 19.9 years (SD=0.8, range=16.6–25.8).
The ability test battery was designed to measure general ability and logical thinking. The test assortment comprises verbal, arithmetic, and visuospatial reasoning subtests. Each subtest is composed of 40 multiple-choice questions in a series proceeding from the easiest to the most complicated. Each subtest gives scores that are converted to stanines (standard nines). The range of scores is 1–9, with a mean of 5.00 and a standard deviation of 1.96. The test-retest reliabilities of the subtests vary from 0.76 to 0.88 (J. Sinivuo, 2003 file on Finnish Defense Forces).
The verbal reasoning subtest comprises four types of questions. The subject has to choose synonyms or antonyms of a given word, to select a word belonging to the same category as a given word pair, to choose which word of a word list does not belong in the group, and to choose similar relationships between two word pairs.
The subtest for arithmetic reasoning comprises four types of problems. The subject has to complete a series of numbers that have been arranged to follow a certain rule, to solve verbally expressed short problems, to compute simple arithmetic operations, and to choose similar relationships between two pairs of numbers. The verbal and arithmetic subtests are presented in 10 unseparated blocks. Each block includes four problems (one problem of each type), and thus the total number of problems in each subtest is 40.
The visuospatial reasoning task is a set of matrices containing a pattern problem with one removed part. The subject is asked to decide which of the given single figures completes the matrix. This test is analogous to the widely used Raven’s Progressive Matrices (16, 17), and it requires the subject to conceptualize spatial relationships ranging from the very obvious to the very abstract.
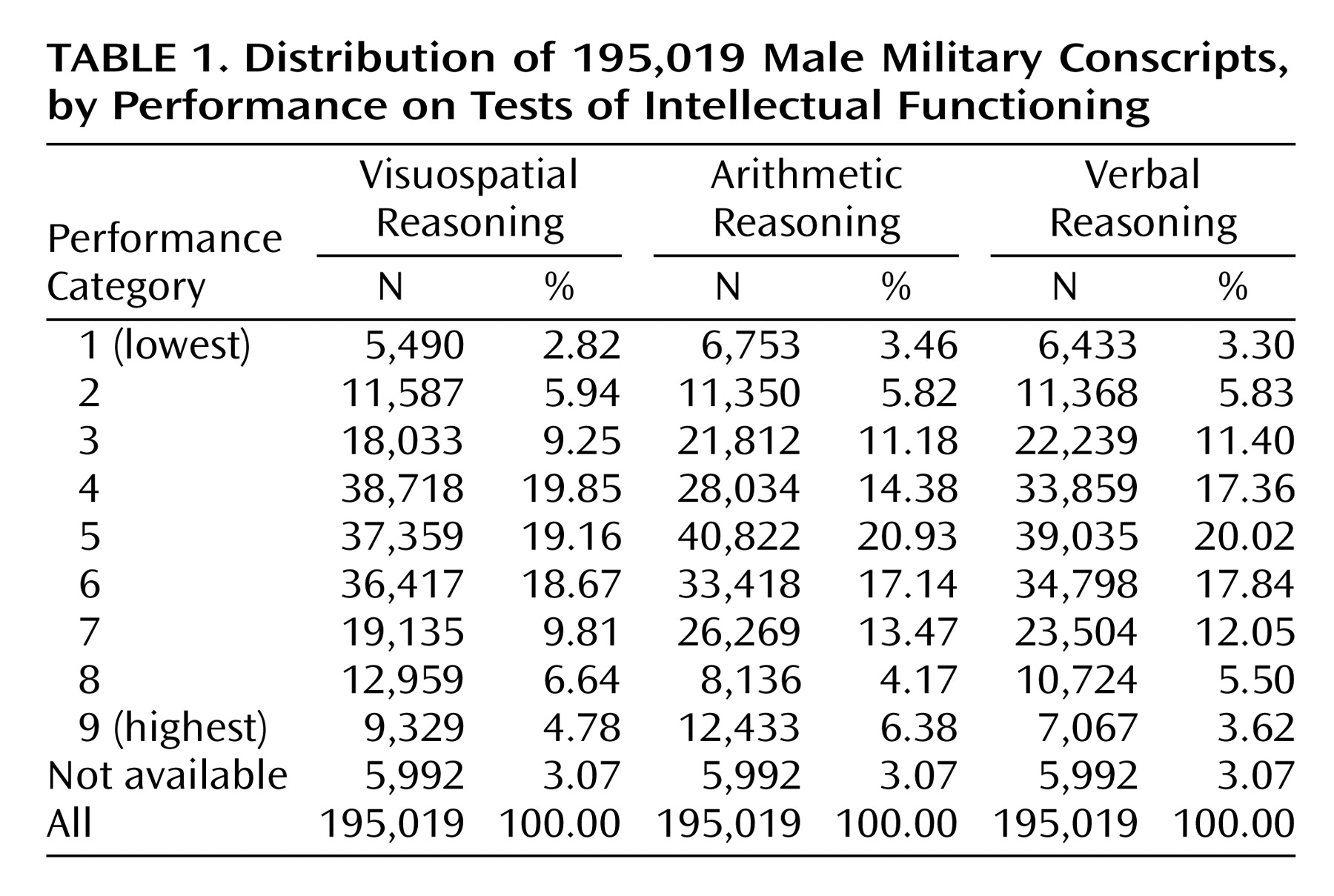
The distribution of the entire study population in the test functioning categories from 1 to 9 is shown in
Table 1.
Psychiatric Status at Follow-Up
The Finnish Hospital Discharge Register was used to identify all persons in the study population who had been hospitalized because of bipolar disorder (ICD-8 codes 296.10 and 296.30; ICD-9 codes 2962-, 2963-, 2964-, and 2967A), schizophrenia (ICD-8 codes 295.00, 295.10, 295.20, 295.30, 295.40, 295.50, 295.60, 295.80, and 295.99; ICD-9 codes 2951-, 2952-, 2953-, 2954A, 2956-, 2957A, and 2959-), or other psychosis (ICD-8 codes 296.88, 296.99, 297.00, 297.98, 298-, 299.99; ICD-9 codes 2961E, 2971A, 2973A, 2988A, and 2989X) before Jan. 1, 1992. If there were multiple diagnoses for one individual, the last observed diagnosis was used. As a result of the record linkage, we found that 100 cohort members had subsequently been hospitalized with a diagnosis of bipolar disorder, 621 with a diagnosis of schizophrenia, and 527 with diagnoses of other psychoses. The mean follow-up time was 7.1 years (SD=1.7). The age at onset was defined as the age at the beginning of first hospitalization for any diagnosed psychiatric disorder. The diagnostic validity of the Finnish Hospital Discharge Register has been examined against DSM-III-R criteria and has been found to have excellent specificity for diagnoses of schizophrenia (92%–100%) (18–21) and bipolar disorder (92%) (22). The mean length of time between the ability test and the first hospitalization due to a diagnosed psychosis was 3.6 years (SD=2.1) for schizophrenia, 3.9 years (SD=2.5) for bipolar disorder, and 4.1 years (SD=2.5) for other psychoses. There were 134 subjects who had been hospitalized because of a psychosis before the ability test, and these subjects were not included in the study.
Statistical Analysis
The risk of psychiatric disorder was analyzed with logistic regression. The results of the tests were given in terms of the ordered scale of nine classes. In the logistic regression analysis the ability test results were used as categorical explanatory variables, with the fifth performance category used as a reference. The regression analyses were carried out for each subtest separately. Since the stanine categories obtained from the military database were not continuous variables, it was not possible to calculate descriptive statistics such as means and standard deviations. Birth year, test year, and age at the time of testing were used as background categorical variables, which were controlled for in all models. Tests for linear trend components were carried out for each subtest separately (23).
Results
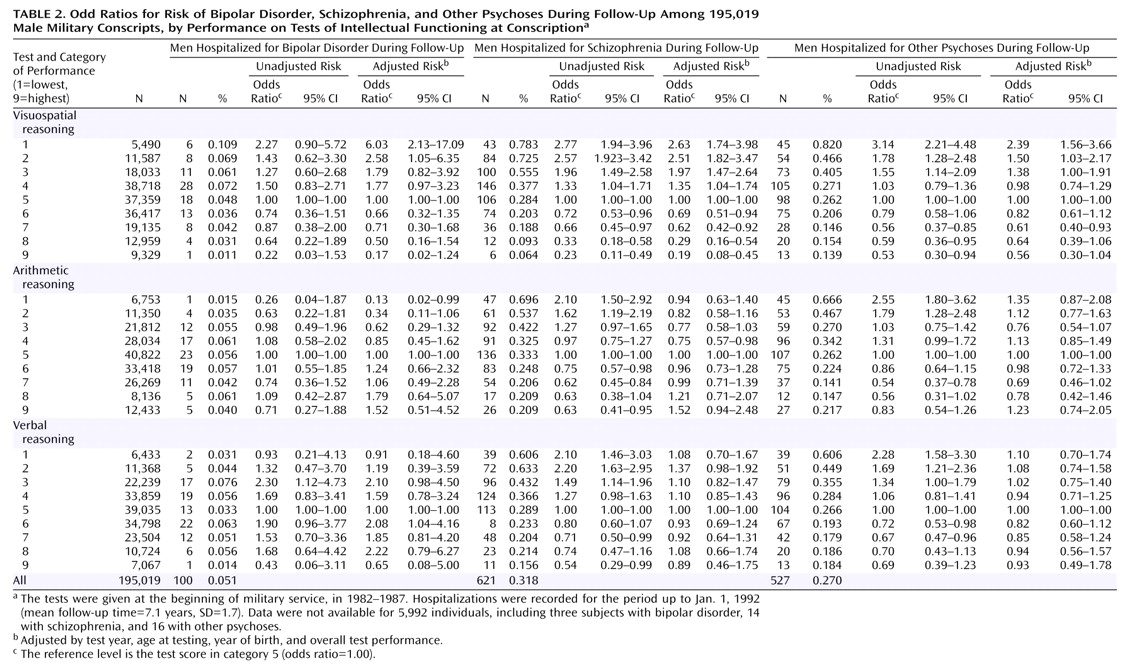
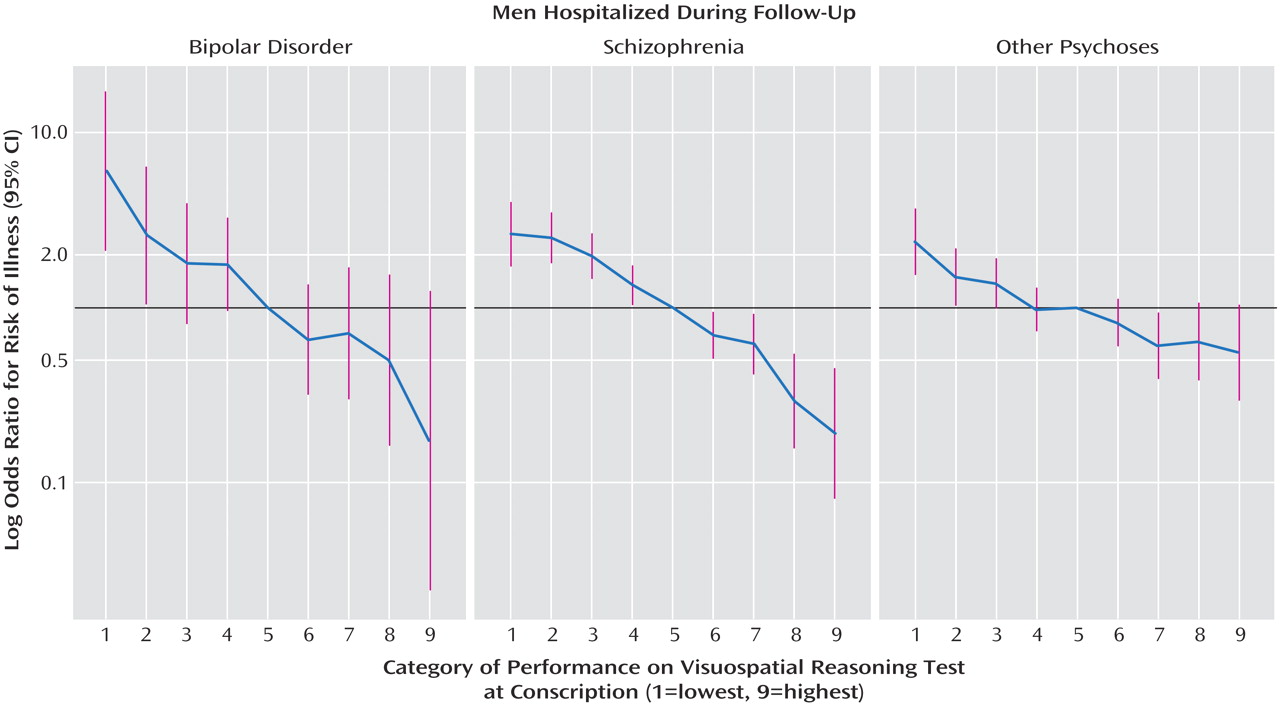
The adjusted odds ratios show that the risks of bipolar disorder (N=100), schizophrenia (N=621), and other psychoses (N=527) increased progressively (p<0.0001 for linear trend) as a function of declining performance on the subtest for visuospatial reasoning (
Table 2,
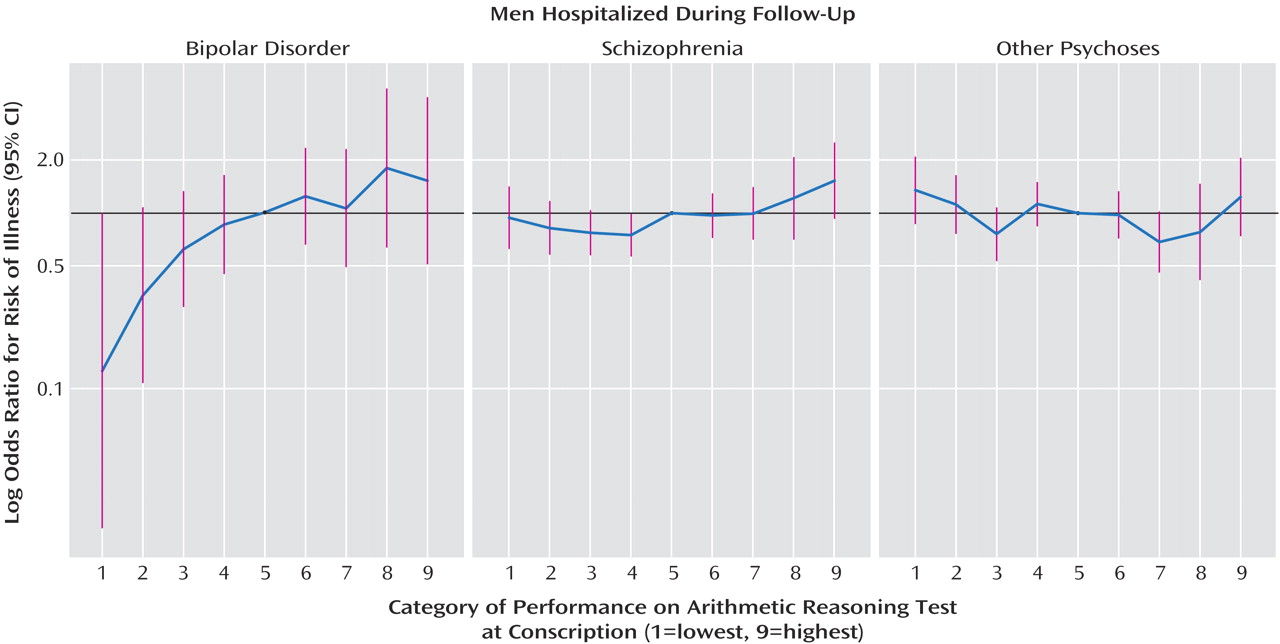
Figure 1). The odds ratios interpreted as the increase in risk for each successive stanine category were 1.41 for bipolar disorder, with a 95% confidence interval (CI) of 1.21–1.63, 1.35 (95% CI=1.27–1.44) for schizophrenia, and 1.19 (95% CI=1.11–1.27) for other psychoses. The odds ratios indicating the difference in risk of illness between the lowest performance (category 1) and the highest (category 9) were 34.65 (95% CI=4.05–296.44) for bipolar disorder, 13.76 (95% CI=5.49–34.47) for schizophrenia, and 4.28 (95% CI=2.09–8.77) for other psychoses. When the subjects who were hospitalized during the first 12 months after the test (N=87) were omitted, the odds ratios did not change substantially (odds ratio=20.87 for bipolar disorder, 12.42 for schizophrenia, and 4.06 for other psychoses). No independent risk increase was associated with performance on the test of verbal functioning (odds ratios for linear trend, 1.0 for all disorders). The adjusted odds ratios revealed that the risk of bipolar disorder increased progressively (p=0.008 for linear trend) as a function of increasing score on the arithmetic subtest; the odds ratio indicating the difference in risk between category 1 and category 9 was 0.08 (95% CI=0.01–0.81), corresponding to an odds ratio of 0.81 (95% CI=0.70–0.95) for linear successive change in risk, resulting in a 12-fold risk of bipolar disorder in the highest performance category (
Figure 2). No linear trend was detected in the risk for schizophrenia or other psychoses.
There was no relationship between age at onset of psychiatric illness and performance on the ability tests. We checked whether the length of follow-up after testing had any effect on the results. However, the interpretation did not materially change when different lengths of follow-up (2, 4, 6, 8, and 10 years) were considered.
Discussion
This longitudinal follow-up study of a large cohort of Finnish male conscripts examined the risk of later functional psychotic illness in relation to performance on ability tests in late adolescence. Premorbid visuospatial intellectual performance was impaired in all three categories of functional psychotic illness (schizophrenia, bipolar disorder, and other psychoses), and a dose-response relationship was evident in that the lower the score on the visuospatial subtest, the greater the risk for any of the three disorders. Performance on the verbal subtest was not associated with the adjusted risk of later psychiatric disorder. The unadjusted odds ratios indicate that the risk of schizophrenia was slightly increased among subjects with poor performance on the verbal subtest, but this was explained by the correlation between subtest scores, i.e., poor verbal performance was not a risk factor per se when visuospatial and arithmetic test results (in addition to age, birth year, and test year) were controlled for with logistic regression; it was only an indicator of poor overall performance. On the contrary, poor visuospatial performance was an independent risk factor and not just an indicator of poor overall performance. However, the higher the score on the arithmetic subtest, the greater the risk of bipolar disorder. The conscripts were screened in medical examinations by physicians and were observed by the officers during the first weeks of their military service, and therefore, they were considered healthy during the time of the testing. We found that premorbid intellectual functioning was not associated with age at onset of illness, which suggests that poor intellectual performance was not explained by prodromal symptoms.
This study adds to the large literature showing a premorbid intellectual deficit in schizophrenia (1–11, 15) but takes it further by demonstrating that visuospatial reasoning may be a core element of this premorbid intellectual deficit. Previous prospective studies have focused on general aspects of intellectual development, using educational test scores (1) or archived information collected for purposes other than identification of precursors of psychiatric illness, such as school records (9). The high-risk study design, which investigates childhood development in offspring of an affected parent, has been able to provide information on specific neuropsychological abilities (6), but its application is limited because only 10%–15% of patients with psychosis have an affected parent. Studies of conscripts who have undergone extensive testing upon joining military service at age 18 or 19 provide useful information on specific premorbid intellectual abilities. Such cohorts have provided valuable information on premorbid intellectual (2, 8–10) and social and behavioral (10, 24, 25) functioning in schizophrenia as well as identifying environmental risk factors for psychosis, such as cannabis use (26, 27) and urban birth (28). Our study adds to this “conscript” literature by examining specific intellectual abilities at age 20 in what we believe to be the largest group yet studied of individuals who later were diagnosed with psychotic illnesses.
Comparison With Similarly Designed Conscript Studies
Performance on general intelligence tests and subtests for verbal ability, visuospatial reasoning, general knowledge, and mechanical knowledge was examined in relation to later schizophrenia (N=195) and nonschizophrenic psychoses (which included bipolar disorder) (N=192) in a Swedish cohort of conscripts tested between 1969 and 1970 (2). This study found a linear relationship between low intelligence score and later schizophrenia, but the relationship between intelligence score and “other psychosis” (which included affective psychosis) departed significantly from linearity. Although visuospatial performance was impaired in both groups, only the deficit in mechanical knowledge remained significant after adjustments were made for the results on all the other subtests. This same cohort (N=50,087) was used in a recent study (15) that showed that during a 27-year follow-up period the low general intelligence score was associated with a higher risk for hospital-treated schizophrenia, severe depression, and other nonaffective psychoses, but no risk increase was observed for bipolar disorder. The general intelligence score in this study was a composite score of general knowledge, verbal intelligence, visuospatial ability, and mechanical ability. Mechanical ability (not visuospatial ability) was the strongest predictor of schizophrenia. One explanation for the discrepancy between this finding and our results, as well the results of Reichenberg et al. (9), could be that the visuospatial ability test used by the Swedish army may differ from the tests used by the Finnish and Israeli armies (which are based on Raven’s Progressive Matrices). This may also explain the difference between our finding on the association between visuospatial reasoning and risk of bipolar disorder and the parallel results from the Swedish cohort (15). The intelligence test used in Sweden did not include a mathematical subtest, and therefore, it is not possible to compare our finding about the association between mathematical ability and risk of bipolar disorder with the results of Zammit et al. (15).
In a later Swedish conscript cohort (8), tested between 1990 and 1997, performance on tests of verbal ability, visuospatial reasoning, mechanical/technical skills, and general intelligence was examined in relation to later schizophrenia (N=60) and nonschizophrenic, nonaffective psychoses (N=92). The authors found that low scores across a range of tests of intellectual functioning predicted later nonaffective psychosis. The effects were generally stronger for schizophrenia than for other nonaffective psychoses.
Low intellectual performance at conscription (between 1985 and 1991) predicted later schizophrenia (N=509) in the Israeli Draft Board Registry Study (10). The relationship did not deviate significantly from linearity. Results for the individual subtests were not presented. Reichenberg and co-workers examined an expanded version of this cohort and investigated performance on individual subtests in relation to later schizophrenia (N=536), schizoaffective disorder (N=31), and nonpsychotic bipolar disorder (N=68) (9). Subjects with schizophrenia showed significant premorbid deficits on all intellectual measures, whereas subjects with nonpsychotic bipolar disorder showed no differences from the comparison group. Subjects with schizoaffective disorder were significantly impaired only on Raven’s Progressive Matrices (visuospatial reasoning).
There is a remarkable confluence between the results of the previous conscript studies and ours in showing that schizophrenia is linked with low premorbid intellectual functioning in an inverse linear fashion. The linear trend of the risk indicates that low premorbid intelligence is associated with greater risk, and high premorbid intelligence with lower risk, of mental illness when compared with average intelligence levels. This implies that high intelligence may protect individuals against schizophrenia, by contributing to better insight or through other protective factors.
Our findings concur with those of the Israeli Draft Board Registry Study (9) in showing that performance on visuospatial reasoning showed larger effect sizes than verbal or arithmetic tests for risk of later psychosis. We had the power to take this further by showing a differential pattern of premorbid intellectual functioning in bipolar disorder whereby visuospatial reasoning is impaired but premorbid arithmetic ability is intact and may actually exceed that of comparison subjects. The finding of an association between progressively increasing risk of bipolar disorder and high arithmetic intellectual performance is rather surprising. The arithmetic test not only requires mathematical skills but also rapid information processing, since the limited amount of time for solving the tasks allows only a small percentage of subjects to finish the test. It is plausible to assume that subjects having the ability to rapidly process information may share the same neurobiological characteristics as subjects who develop mania, a state characterized by high alertness and psychomotor activity. It is tempting to speculate that good arithmetic or psychomotor performance may have contributed in human evolution to the persistence of bipolar disorder, which is strongly genetically transmitted and associated with a high mortality rate (29, 30). Results from a study of Icelandic subjects suggest that relatives of people with psychosis excel in school, particularly in mathematics (31). It has also been suggested that pupils with the highest academic achievements also may have a higher risk of developing schizophrenia as an adult (32).
Strengths and Limitations
We believe that the database used in the present study is the largest thus far for investigating an association between premorbid intellectual functioning and the risk of mental disorders. This data set allowed us to detect risk increases for bipolar disorder with sufficient statistical power. A possible limitation is that the diagnoses in our study were taken from a national hospital discharge register (Finnish Hospital Discharge Register) and therefore raise concerns about the validity and reliability of the diagnoses. In Finland, over 90% of the people with a psychotic disorder are hospitalized (18), and the diagnostic validity (specificity) of the Finnish Hospital Discharge Register diagnoses of schizophrenia and bipolar disorder has been found to be over 90% (93% for schizophrenia and 92% for bipolar I disorder) (18–22). Another limitation is that information on the socioeconomic status of the family of origin was not available, but the visuospatial intellectual functioning measured by Raven’s Progressive Matrices is independent of education or cultural or socioeconomic factors (16, 17), and validation data on 3,250 children and adolescents showed that the socioeconomic status of the family accounts for less than 5% of the test variance (17).
In conclusion, these results provide what we believe to be the first evidence from a large prospective study showing that premorbid visuospatial reasoning is impaired in bipolar disorder, schizophrenia, and other psychoses but that high arithmetic ability is associated with greater risk for later bipolar disorder. Therefore, our findings indicate both shared and unique aspects in the etiology of bipolar disorder and schizophrenia.