Positive Genetic Test for Negative Symptoms
The several subtypes of schizophrenia may actually be separate disorders. This heterogeneity complicates efforts to clarify the disease process. Fanous et al. (p. 1824) examined specific clinical features, rather than diagnoses, in relation to the DTNBP1 gene in 1,425 members of families with high rates of schizophrenia or poor-outcome schizoaffective disorder. A high-risk haplotype, i.e., set of alleles previously demonstrated to be strongly associated with schizophrenia, was more likely to be transmitted to people with high levels of negative symptoms, such as incoherence and restricted emotional expression. The DTNBP1 gene codes for dysbindin, which is expressed in lower levels in the prefrontal cortex and hippocampus of people with schizophrenia. These sites are involved in working memory and memory formation, respectively, cognitive functions related to the negative symptoms included in this study. The etiologic relevance of this genetic variation supports the influence of genetic factors on schizophrenia’s heterogeneity.
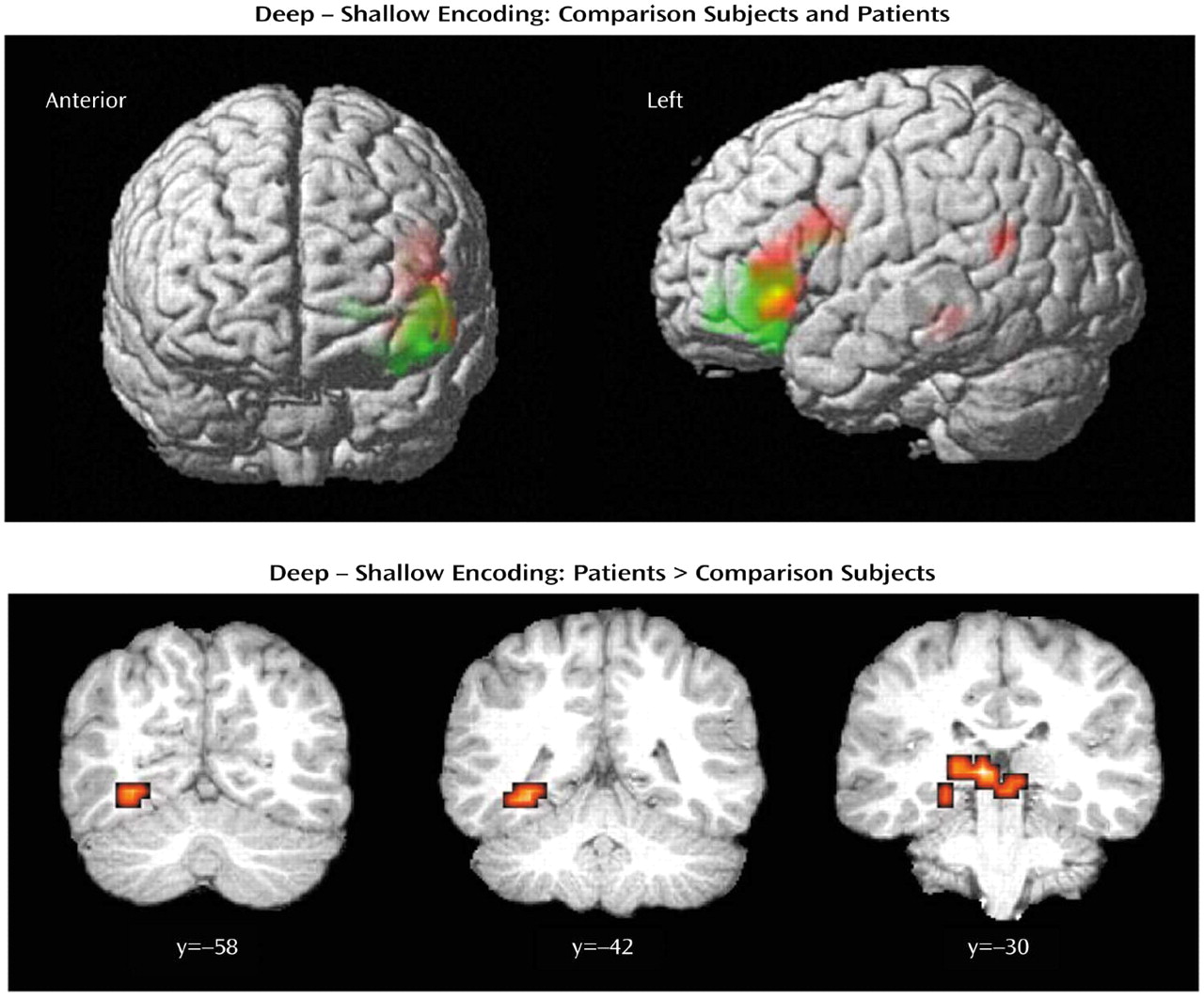
Semantic Strategies for Schizophrenia
People with schizophrenia have particular difficulty in remembering words, but it is not clear whether the problem is poor recall or an inability to store the words initially. Neuroimaging can show differences in brain activity between schizophrenic and healthy groups during both encoding and retrieval. During encoding, Ragland et al. (p. 1840) asked subjects to classify some words as either uppercase or lowercase, a perceptual distinction requiring shallow mental processing. Other words were classified as concrete or abstract, to require deeper processing. Encoding was accompanied by activation of the left ventrolateral prefrontal cortex in both groups, but the patients were slower and less accurate in classifying words, and overactivation occurred in some brain areas. Nevertheless, deep processing improved recognition during word retrieval to the same degree as in the healthy subjects. This improvement based on the level of processing suggests a means of enhancing memory in people with schizophrenia.
Taking the Dopamine Hypothesis to the Thalamus
Evidence of abnormalities in schizophrenia relates to both brain chemistry and anatomy. The neurotransmitter dopamine and the thalamus have been implicated separately, but dopamine signaling in the thalamus is largely unexplored. Clinton et al. (p. 1859) examined brain slices from deceased schizophrenia patients and normal subjects and compared mRNA expression of five dopamine receptors, binding to the D1, D2, and D3 receptors, a marker of presynaptic nerve supply, and three intracellular proteins with roles in dopaminergic signaling. The patients’ brains showed no abnormalities in dopamine receptor transcripts or binding sites but did have high levels of calcyon and spinophilin mRNA. Both proteins appear to mediate intracellular interactions between dopamine and other neurotransmitters, such as glutamate.
Precursors of Schizophrenia, Bipolar Disorder
Even before schizophrenia is apparent, people who will later develop it have generally worse school performance and lower IQs than their peers. Tiihonen et al. (p. 1904) examined the nature of the impairment and whether it also occurs in bipolar disorder and other psychoses. Results of tests measuring verbal, arithmetic, and visuospatial reasoning were available for 195,019 men conscripted into the Finnish military between 1982 and 1987. The Finnish Hospital Discharge Register was used to identify conscripts later hospitalized for psychosis. By 1992, 100 of the men had been hospitalized with bipolar disorder, 621 with schizophrenia, and 527 with other psychoses. The earlier test results showed that all three diagnostic groups had impaired visuospatial reasoning before identification of the illness. A dose-response relationship was evident—the lower the score, the greater the risk of illness. Surprisingly, men who developed bipolar disorder had higher arithmetic scores, perhaps because of exaggerated alertness and psychomotor activity.
Adolescent’s Diagnosis and Gender Shape Adult’s Personality Disorder
A large study of adolescent psychiatric patients who were reinterviewed 28 years later confirms that personality disorders are common in adults who had disruptive behavior disorders or emotional disorders (e.g., depression) during adolescence. Helgeland et al. (p. 1941) interviewed 130 subjects in their mid-40s and found personality disorders in 65% of those who had disruptive behavior disorders in adolescence and 58% of those who had emotional disorders. Several outcomes were influenced by gender. Among men, personality disorders were more common in those who had disruptive behavior disorders during adolescence than in those with emotional disorders, and the likelihood of personality disorders decreased as age increased. Among women, antisocial and related personality disorders were associated with disruptive disorders during adolescence, and emotional disorders in adolescence were associated with avoidant, dependent, and obsessive-compulsive personality disorders. The differing developmental pathways for males and females could be due to culture, biological factors, or both.
Images in Psychiatry
Augusta Mental Health Institute, 1840–2004 (p. 1823)