DSM-IV recognizes two specific eating disorders, anorexia nervosa and bulimia nervosa, together with a residual diagnostic category termed “eating disorder not otherwise specified”
(1) . In outpatient settings, the most common eating disorder diagnosis is eating disorder not otherwise specified, followed by bulimia nervosa and then anorexia nervosa
(2 –
5) . Despite its prevalence, there have been no studies of the treatment of eating disorder not otherwise specified. Some treatment studies have included subthreshold cases of anorexia nervosa or bulimia nervosa
(6,
7), and there has been interest in binge eating disorder
(8), a subtype of eating disorder not otherwise specified, but such cases constitute less than half those with eating disorder not otherwise specified
(5) . The majority have a mixed clinical picture in which the features of anorexia nervosa and bulimia nervosa are combined in various ways
(5) . The treatment of these patients has not been studied.
Given that the clinical features of bulimia nervosa and eating disorder not otherwise specified are very similar, it has been postulated that treatments that have beneficial effects on bulimia nervosa should also benefit patients with eating disorder not otherwise specified
(9) . Were this to be the case, such treatments would be of great clinical value as they could be used with about 80% of outpatients with an eating disorder.
The leading treatment for bulimia nervosa is a specific form of cognitive-behavioral therapy (CBT)
(10,
11) . Recently this treatment has been reformulated so that rather than being a treatment for bulimia nervosa in particular, it is now a treatment for eating disorder psychopathology whatever the DSM-IV diagnosis
(12) . There are two forms of this “enhanced” treatment (CBT-E): a focused form (CBT-Ef) that targets eating disorder psychopathology exclusively, and a more complex broad form (CBT-Eb) that also addresses certain additional problems—mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties—that commonly appear to maintain eating disorders or complicate treatment
(12) .
In this study we compared these two treatments in outpatients with any form of eating disorder provided that their body mass index (BMI) was over 17.5. Thus the patients in the study met DSM-IV diagnostic criteria for bulimia nervosa or eating disorder not otherwise specified, but patients in the anorexia nervosa weight range were excluded by the BMI cutoff. The first aim of the study was to compare the two treatments with a waiting list control condition. This was essential because nothing is known about the spontaneous remission rate among patients with eating disorder not otherwise specified. The second and main aim was to compare the effects of the treatments at treatment completion and after a 60-week period of follow-up. A substantial period of follow-up was essential because eating disorders are prone to relapse and treatments have been found to differ in their relative longer-term effects
(13,
14) . The third aim was to determine whether DSM-IV eating disorder diagnosis was a moderator of treatment response, a question of clinical and nosological significance. The fourth aim was to explore the relative effects of the two treatments in patients with and without mood intolerance, clinical perfectionism, low self-esteem, or marked interpersonal difficulties.
Method
Design
A randomized controlled trial was conducted at two eating disorder centers. Eligible patients underwent randomized assignment to four treatment conditions: CBT-Ef, CBT-Eb, or an 8-week delay in starting treatment followed either by CBT-Ef or CBT-Eb. Patients were assessed before treatment, after 8 weeks of treatment, at the end of treatment, and, for those in the control condition, at the end of the waiting list period preceding treatment. After treatment, patients were entered into a period of follow-up and reassessed 20, 40, and 60 weeks later. During follow-up, the patients received no further treatment unless it was judged necessary on clinical grounds (i.e., follow-up was closed). The study was approved by the two local human subjects committees. The trial was registered with Current Controlled Trials (ISRCTN no. 15562271, http://controlled-trials.com).
Recruitment
Participants were recruited from consecutive referrals by family doctors and other clinicians to two well-established eating disorder clinics in the United Kingdom, one serving central Oxfordshire and the other Leicester city.
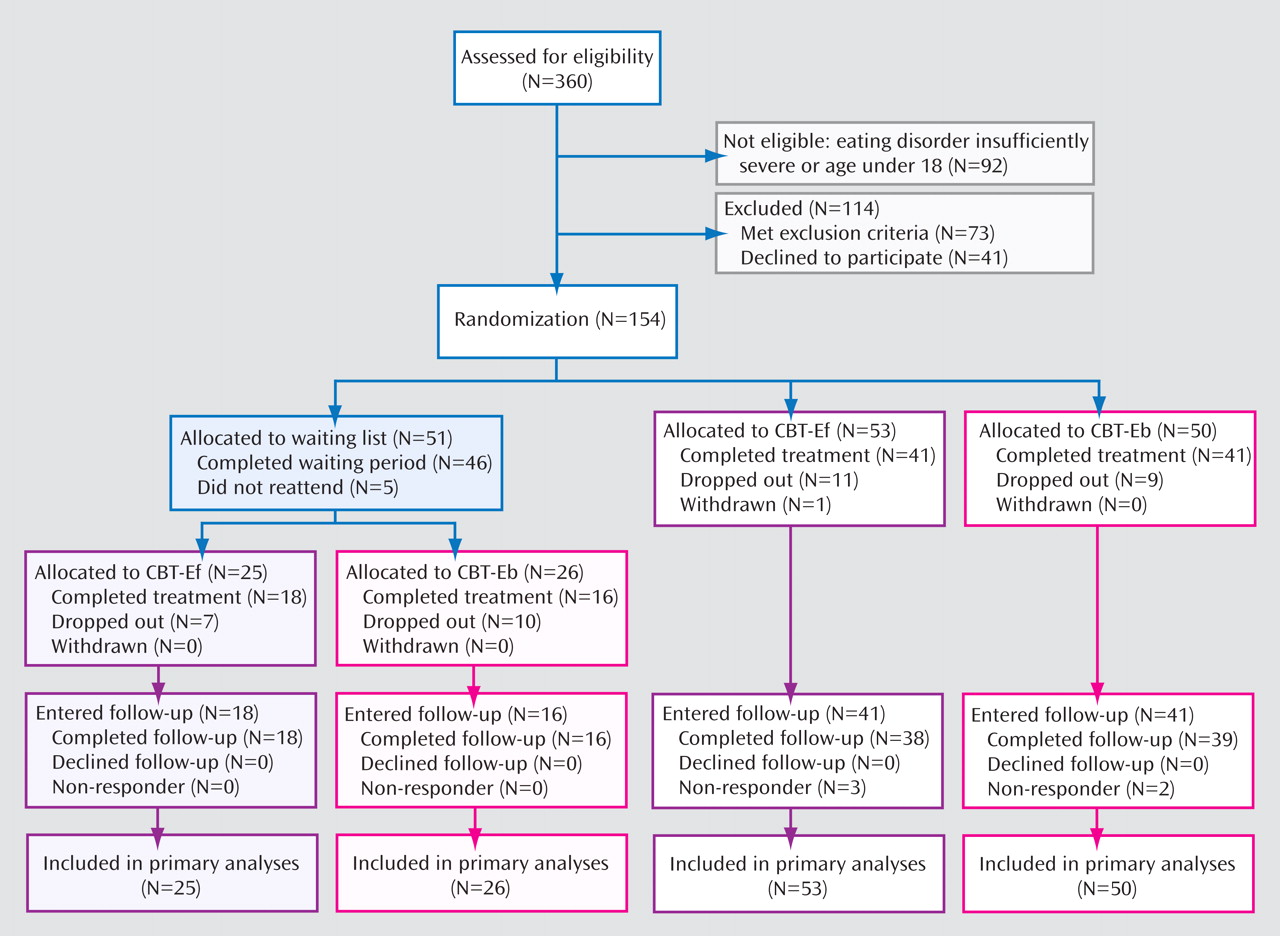
Figure 1 summarizes participant enrollment and flow through the study. Recruitment was designed to be broadly inclusive, with few exclusion criteria. To be eligible, patients had to have an eating disorder requiring treatment, as judged both by the referring clinician and subsequently by the senior eating disorder specialist at each site (Z.C., C.G.F., or R.L.P.); be 18 to 65 years of age; have a BMI over 17.5; and provide written informed consent after receiving a complete description of the study. The exclusion criteria were prior receipt of a treatment closely resembling CBT-E or an evidence-based treatment for the same eating disorder (N=12); a coexisting axis I psychiatric disorder that precluded eating disorder-focused treatment (N=22); medical instability or pregnancy (N=0); and not being available for the following 28 weeks (N=39). Patients who were receiving ongoing psychiatric treatment were weaned from it before entering the study (N=4); an exception was clinically warranted antidepressant medication (N=76), which was kept stable during treatment.
Treatment
Both forms of CBT-E are designed for adult outpatients with any form of eating disorder. A detailed treatment manual is available
(15,
16) . Both treatments comprise twenty 50-minute sessions, preceded by one 90-minute preparatory session and followed by a review session 20 weeks after treatment. The first 4 weeks of CBT-Ef and CBT-Eb are identical and solely address the eating disorder. Thereafter the two treatments diverge, and at this point the therapists in the trial learned which treatment their patients had been assigned to receive. In CBT-Ef the remainder of treatment is concerned with addressing the remaining eating disorder features (e.g., the overconcern with shape and weight, extreme dieting, binge eating, purging)
(15), whereas in CBT-Eb the remaining sessions also address mood intolerance, clinical perfectionism, low self-esteem, or interpersonal difficulties, as indicated in the individual patient
(16) . The two treatments are illustrated in the clinical vignettes. (Further information about the treatments can be obtained at www.psychiatry.ox.ac.uk/credo; the web site also provides access free of charge to the materials needed to practice CBT-E.)
Five therapists took part; four were psychologists and one was a psychiatric nurse specialist. All had generic clinical experience and experience treating patients with eating disorders, and each received 6 months’ initial training. Each therapist conducted both treatments. Weekly supervision meetings were led by Z.C. and C.G.F. throughout the study. All sessions were recorded and were regularly audited to ensure that the treatments were well implemented.
Assessment
Eating disorder features
These were assessed using the 16th edition of the Eating Disorder Examination interview (EDE)
(17) and its self-report version (EDE-Q)
(18) . The EDE was administered by assessors who were trained and supervised by M.E.O., an expert on the instrument. The assessors were blind to the patients’ treatment condition and had no involvement with treatment. Two primary outcome variables were generated from the EDE ratings: change in the severity of eating disorder features as measured by the global EDE score, and having a global EDE score less than one standard deviation above the community mean (i.e., below 1.74)
(19) . Normative comparisons of this type are widely used to identify clinically significant change
(19 –
21) .
General psychiatric features
These were measured using the Brief Symptom Inventory (BSI)
(22), a short version of the Symptom Checklist—90
(23) . The Structured Clinical Interview for DSM-IV
(24) was used at baseline to identify the presence of coexisting axis I psychiatric disorders.
Treatment suitability and expectancy
These were measured after two treatment sessions and after 8 weeks using widely employed visual analogue scales
(14) . Suitability was measured again at the end of treatment.
Severity of additional psychopathology
For the exploratory fourth aim, the therapists rated the severity of each patient’s mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties after 4 weeks of treatment. In the absence of validated measures of these constructs, their severity was assessed using a 4-point Likert scale; detailed definitions of the four constructs are provided in the CBT-Eb treatment manual
(16) . These ratings were made before the therapist learned the patient’s treatment assignment.
Power and Sample Size
Sample size calculations were performed a priori in terms of the first two aims and outcome variables, on an intent-to-treat basis. With regard to the second and main aim of the study, it was calculated that a sample size of 75 patients per treatment condition was required to provide 80% power at two-sided p<0.05 to detect a difference in global EDE change of 0.45 points, assuming a standard deviation of global EDE change scores of 1.0
(14) (i.e., a moderate effect size of 0.45) and also to detect a difference between the two conditions of at least 25% in the categorical outcome measure. For the first aim, a larger difference was expected, and a sample size of 50 per group would provide 80% power at two-sided p<0.05 to detect a large effect size of 0.6. Thus, the patients were allocated to the four treatment conditions in the ratio 25:25:50:50 (8-week wait then CBT-Ef, 8-week wait then CBT-Eb, immediate CBT-Ef, immediate CBT-Eb, respectively). The third and fourth aims were not the subject of power analyses as the analyses were exploratory.
Randomization
A computer-based minimization algorithm was used by one of the authors (H.A.D., who had no involvement in recruitment) to allocate patients to the four treatment conditions, balancing gender, eating disorder diagnosis, BMI, and need to remain on psychotropic medication. When groups were evenly balanced, pre-prepared blocked randomization lists of varying size were used to allocate patients to the four conditions.
Statistical Methods
The statistical analysis was undertaken by one of the authors (H.A.D.) blind to treatment condition. Standard treatment trial data analytic procedures were used. For the first aim, the endpoint was at 8 weeks. This comparison did not include data on the subsequent treatment response of patients who had first been in the waiting list control condition as their data would have appeared twice. For the other aims the endpoints were at completion of treatment and at 60-week follow-up.
Change scores were calculated. Data are presented as Ns and percentages for categorical data and means and standard deviations for continuous data; 95% confidence intervals (CIs) are used to indicate the uncertainty around the estimates. For data assessed at any one time point, categorical data were compared using chi-square tests or logistic regression analysis. Continuous data were compared using grouped t tests or Mann-Whitney tests and analysis of variance or Kruskal-Wallis tests. Follow-up data were analyzed using both repeated-measures analysis of variance and mixed models to take into account the correlation between repeated measurements and to examine main effects and their interaction, adjusting for the baseline score. Results were similar across both methods.
Unless otherwise stated, the analyses were by intent-to-treat with the initial data brought forward. Other imputation methods were tested, but as there were few missing data, this made little difference to the main findings.
Results
Sample
A total of 154 eligible patients were recruited and underwent randomized assignment between March 2002 and July 2005 (
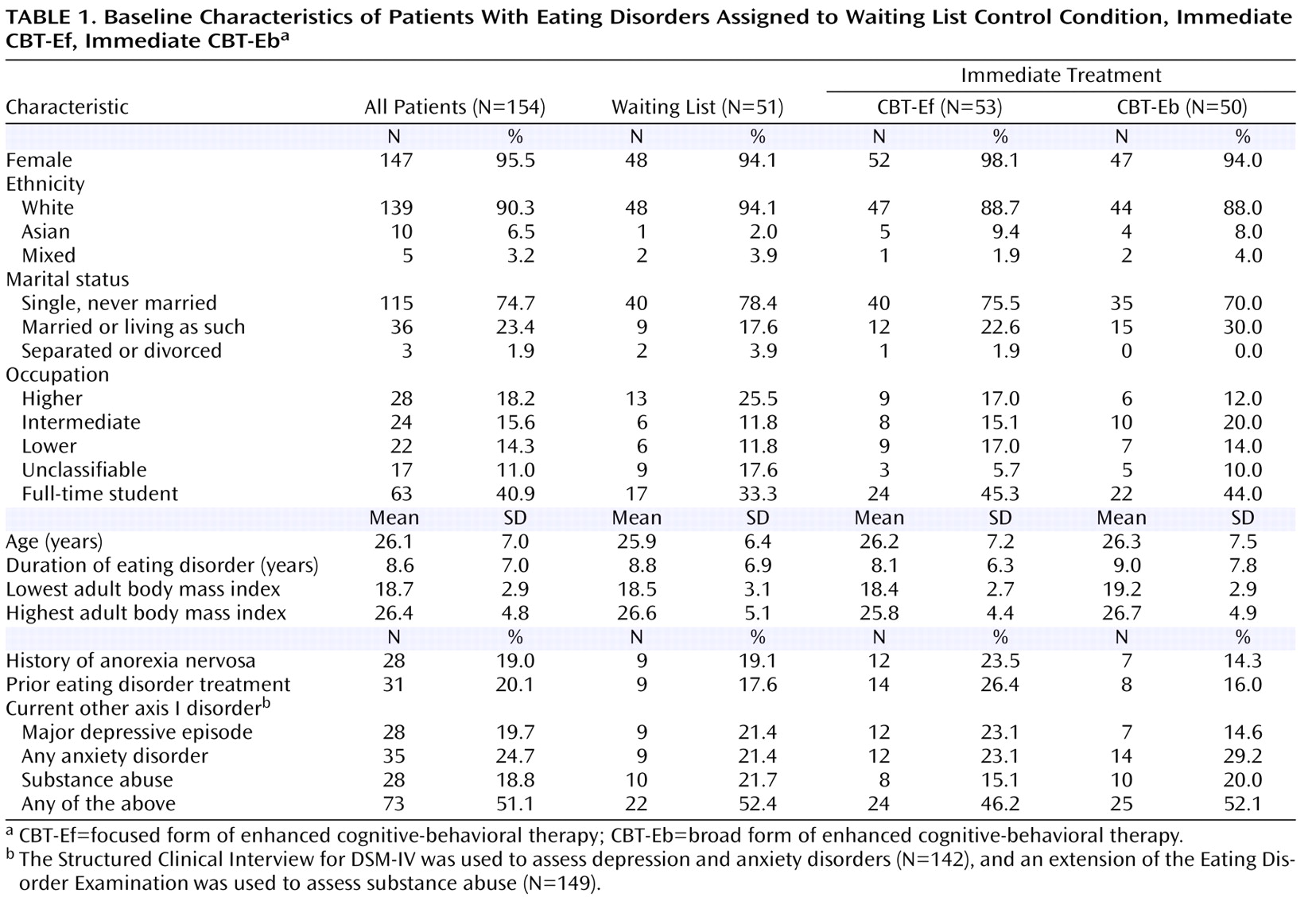
Figure 1 ). Ninety-three (60.4%) were from Oxford, and 61 (39.6%) from Leicester. Five did not attend their initial assessment, all of whom had been assigned to the waiting list condition. Among the remainder (N=149), 57 (38.3%) had a diagnosis of bulimia nervosa and 92 (61.7%) a diagnosis of eating disorder not otherwise specified. Seven patients (4.7% of the full sample) fulfilled the DSM-IV research criteria for binge eating disorder. The characteristics of the sample are summarized in
Table 1 .
Of the 154 patients, 53 were assigned to immediate CBT-Ef, 50 to immediate CBT-Eb, and 51 to the waiting list control condition, after which they received either CBT-Ef (N=25) or CBT-Eb (N=26). The study groups were balanced on all baseline factors except that patients assigned to immediate CBT-Eb were less likely to have a current major depressive episode or a history of anorexia nervosa (
Table 1 ). Adjusting for these two factors in the analyses made no difference to the findings.
Suitability, Expectancy, and Attrition
The ratings of suitability and expectancy were high and did not differ between the two forms of CBT-E. Of the 149 patients who started treatment, 33 (22.1%) did not complete treatment or were withdrawn because of lack of response. The noncompletion figures were 14.0% (8/57) for the patients with bulimia nervosa and 27.2% (25/92) for those with eating disorder not otherwise specified (chi-square p=0.09).
Effects of Immediate Treatment Versus Delayed Treatment
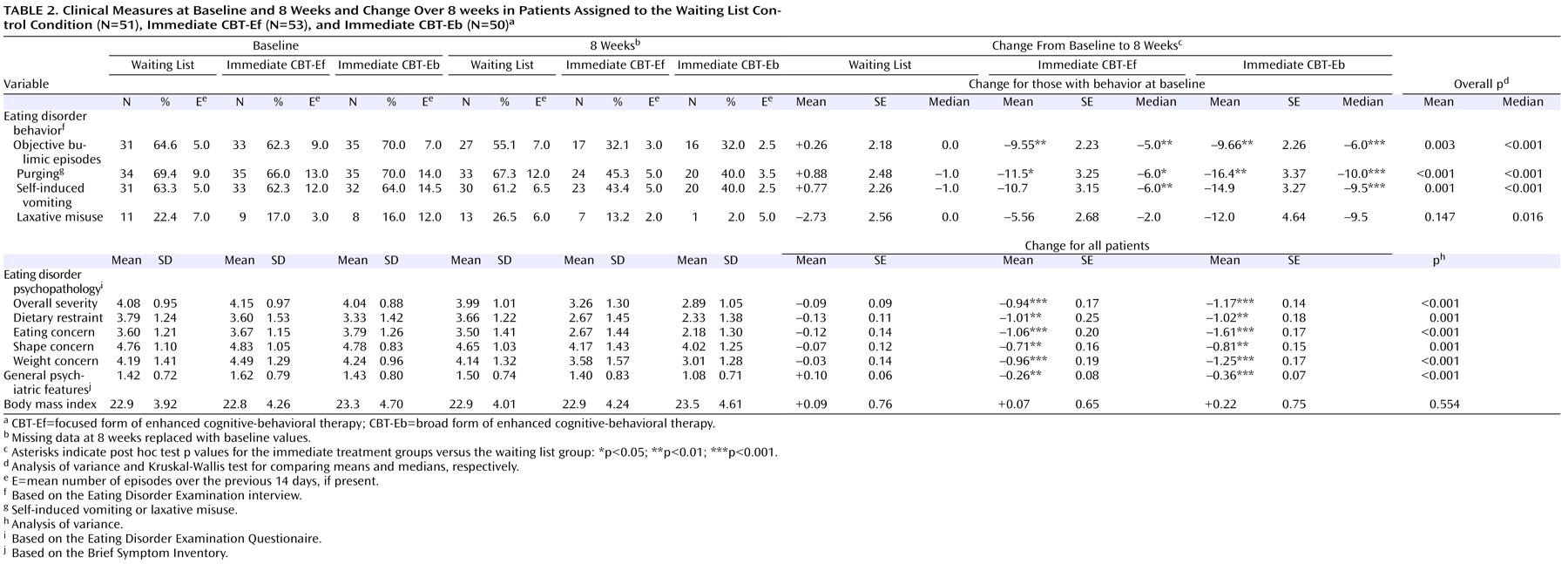
There was little change in patients in the waiting list control condition, whereas there was substantial change in those in the two CBT-E conditions and no significant differences between them (
Table 2 ). There were no significant effects of site. The mean changes in global EDE-Q score were –0.09 (95% CI=–0.28 to 0.10), –0.94 (95% CI=–1.28 to –0.61) and –1.17 (95% CI=–1.45 to –0.90) in the waiting list, CBT-Ef, and CBT-Eb conditions, respectively.
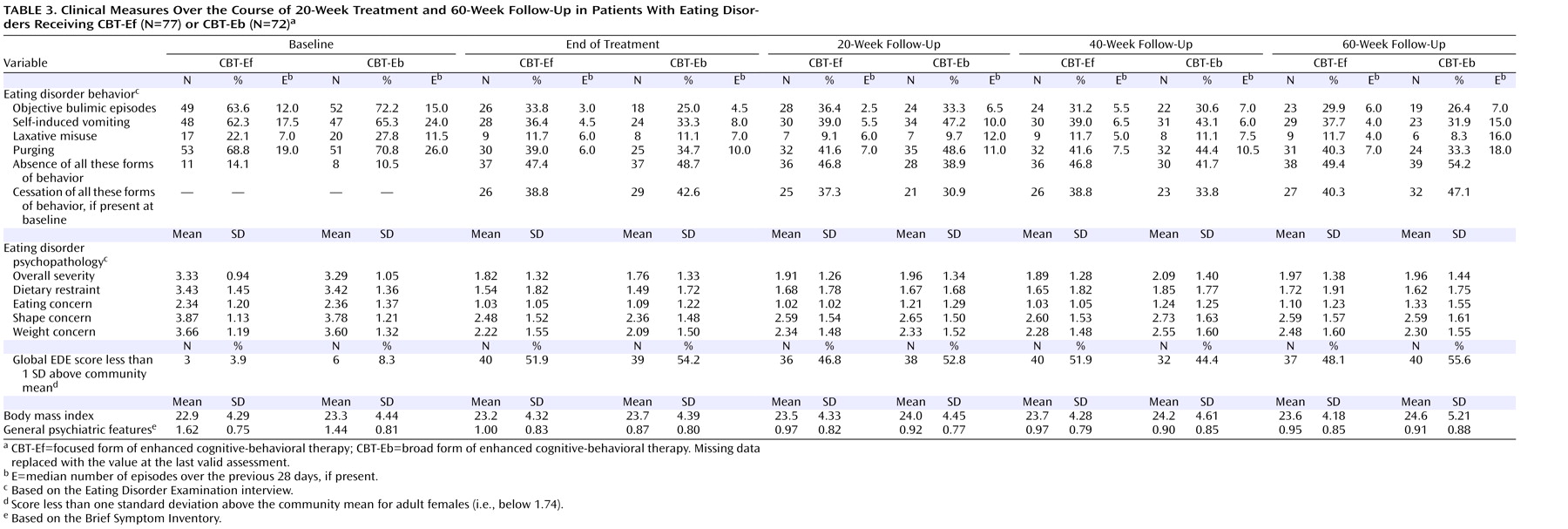
Effects of CBT-Ef and CBT-Eb at End of Treatment and at 60-Week Follow-Up
There was a substantial response to treatment across all measures (
Table 3 ) and no significant differences between the two treatments; indeed, the mean absolute and change scores were almost identical for the two treatments (e.g., global EDE change: –1.51 [SD=1.35] versus –1.53 [SD=1.28] for CBT-Ef and CBT-Eb, respectively). By the end of treatment, half the overall sample (N=79; 51.3%) had global EDE scores below 1.74. There were no significant effects of site. The changes were greater in the patients who completed treatment; for example, at the end of treatment two-thirds (N=77/116, 66.4%) had a global EDE score below 1.74, and there was no difference between the two treatments (66.1% of the CBT-Ef group versus 66.7% of the CBT-Eb group).
Compliance with follow-up was high, with 95.1% (331/348) of the assessments successfully completed. Of the 116 patients who entered follow-up, eight had additional treatment and nine had one to five brief “booster” sessions. The changes were well maintained across the follow-up period. At 60-week follow-up, 50.0% of the overall sample (N=77) had a global EDE score below 1.74. The mean changes in global EDE in the CBT-Ef and CBT-Eb groups were similar at 1.36 (SD=1.42) and 1.33 (SD=1.30), respectively.
Eating Disorder Diagnosis as a Moderator of Treatment Response
The patients with bulimia nervosa and eating disorder not otherwise specified entered the study with very similar psychopathology, as described in a separate report
(5) . This similarity was also present at 8 weeks (data not shown), and on repeated-measures analysis of variance there was no significant main effect of diagnosis at this point. There were also no significant differences between the two diagnostic groups at end of treatment and at 60-week follow-up. At the end of treatment, 52.7% (30/57) of the patients with bulimia nervosa and 53.3% (49/92) of those with eating disorder not otherwise specified had a global EDE score below 1.74, and at 60-week follow-up these figures were 61.4% (35/57) and 45.7% (42/92), respectively.
Additional Psychopathology and the Relative Effects of CBT-Ef and CBT-Eb
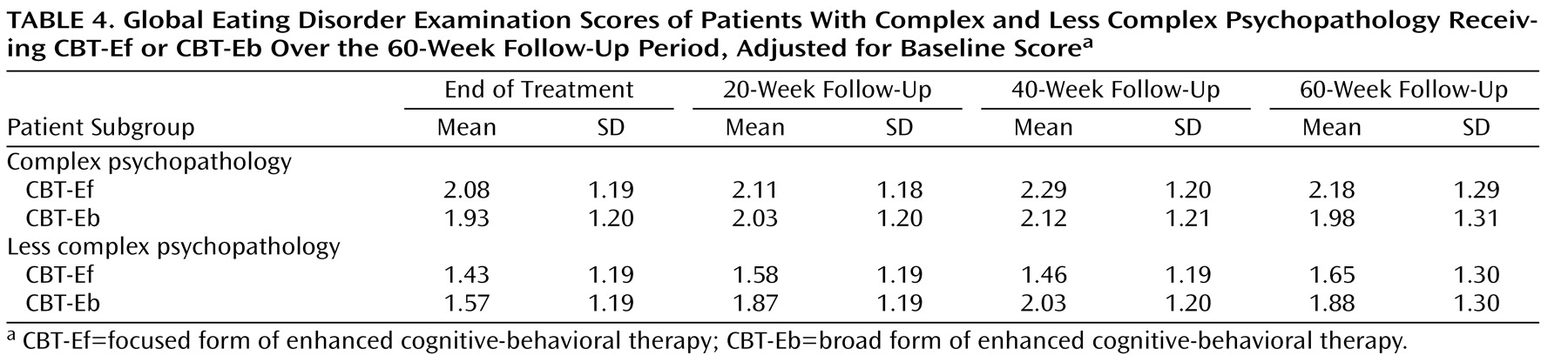
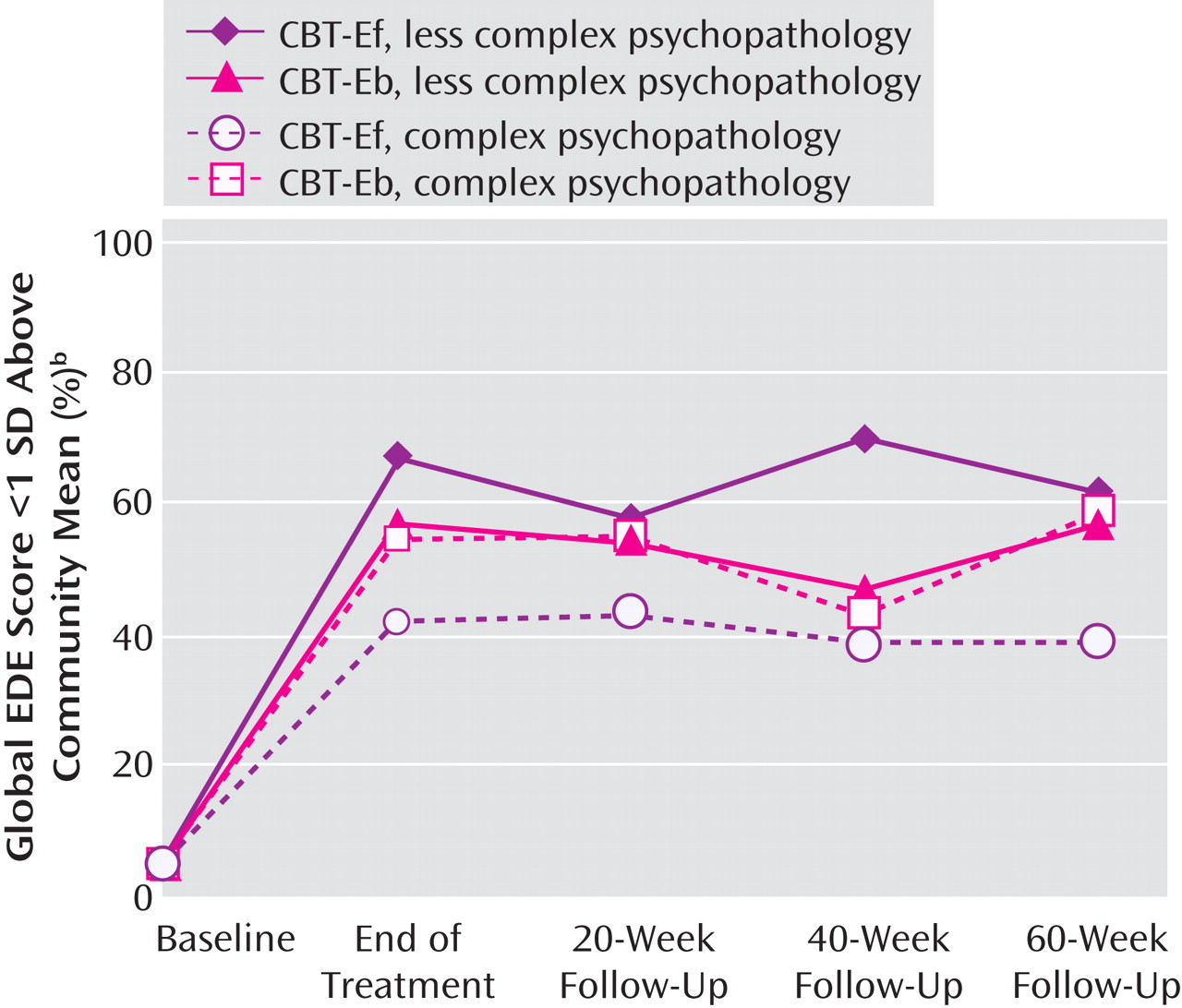
In this exploratory analysis, the clinicians’ ratings of their patients’ mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties were used to identify patients with marked additional psychopathology of the type that CBT-Eb was designed to target. Outcomes for these patients were compared with those of the remainder in relation to the form of CBT-E received. A notable pattern of findings emerged. This was clearest when at least two of the domains had been rated as moderate or major clinical problems. This applied to 54 patients (54/138, 39.1%). This subgroup with “complex” additional psychopathology responded less well in general than the “less complex” subgroup; their mean global EDE score at 60-week follow-up, adjusted for baseline, was 2.09 (95% CI=1.74–2.44), compared with 1.77 in the less complex subgroup (95% CI=1.49–2.05; overall adjusted p value on repeated-measures analysis of covariance, p=0.041), and 48% (95% CI=35–61) had a global EDE score below 1.74, compared with 60% (95% CI=49–70) of the less complex subgroup.
Within the complex subgroup of patients, those who received CBT-Eb had consistently lower adjusted global EDE scores than those who received CBT-Ef (
Table 4 ), and they were more likely to have scores below 1.74 (see
Figure 2 ; e.g., at 60-week follow-up 60% [95% CI=40–79] versus 40% [95% CI=22–58]). The reverse pattern of findings was consistently present among the less complex patients, with CBT-Ef proving superior to CBT-Eb (see
Table 4 and
Figure 2 ).
Discussion
This study is novel since it focused on the treatment of patients with any form of DSM-IV eating disorder provided that their BMI was over 17.5 (i.e., only patients in the anorexia nervosa weight range were excluded). Two transdiagnostic treatments were compared, one that focused solely on eating disorder features and a more complex treatment that also addressed mood intolerance, clinical perfectionism, low self-esteem, or interpersonal difficulties. The sample was a clinically relevant one, as it was recruited from two catchment area clinics and few exclusion criteria were applied. However, over 40% of the potentially eligible patients did not take part, the two main reasons being not being available for the necessary 28 weeks and not wanting to participate in research. A low proportion of the sample had binge eating disorder, which is consistent with previous findings
(2,
3) . With regard to outcome assessment, this is typically measured in terms of change in both the severity of eating disorder features and the proportion of patients with certain clinical features that were universally present at the outset (e.g., binge eating, purging, or being underweight). In this study we were able to use the former criterion (reduction in global EDE score) but the latter could not be employed given the heterogeneous character of the sample (e.g., not everyone engaged in binge eating or purging at the outset). Accordingly, we chose as a second (categorical) outcome variable a normative comparison, namely, achieving a level of eating disorder features less than one standard deviation above the community mean. This is well-established practice in other fields
(19 –
21) and has been done before in this area
(14) .
Four findings are of note. The first is that it was feasible to treat this broad range of patients using one or the other form of CBT-E. The second is that in the waiting list control condition the patients’ symptom severity did not change. Absence of change in bulimia nervosa patients allocated to a waiting list is consistent with previous findings
(25), but this is the first time that such data have been reported for patients with eating disorder not otherwise specified. This lack of change is not surprising given that these patients generally present with a long, unremitting history.
The third finding is that the patients responded well to both treatments and that their DSM-IV eating disorder diagnosis was not a moderator of outcome. At the end of 20 weeks, more than half the overall sample (52.7% and 53.3% of those with bulimia nervosa and eating disorder not otherwise specified, respectively) had a level of eating disorder features less than one standard deviation above the community mean, and at 60-week follow-up the comparable figures were 61.4% and 45.7%. With regard to the bulimia nervosa response rate, at the end of treatment 38.6% (22/57) reported no episodes of binge eating or purging over the previous 28 days, and at 60-week follow-up the proportion was 45.6% (26/57). These figures suggest that CBT-E might be more effective than its earlier version
(14), especially given the inclusive nature of this study’s sample, although a direct comparison of the two treatments is needed to substantiate this conclusion, as response rates vary from study to study. The fact that diagnosis did not moderate outcome at any time point suggests that the distinction between bulimia nervosa and eating disorder not otherwise specified may be of limited prognostic significance.
The fourth finding is tentative and it concerns the relative effects of the two forms of CBT-E. In the full sample, they were no different in their effectiveness. However, the planned exploratory analysis revealed that in patients with substantial additional psychopathology of the type targeted in CBT-Eb, this version of the treatment appeared to be more effective than the focused form, whereas in the remaining patients the opposite was the case. While this pattern of results was consistent over time (
Figure 2 ), many of the individual p values fell short of statistical significance. However, p values are not central to the interpretation of exploratory analyses of this type
(26) . To determine the robustness of this finding, further comparisons of the two treatments are required using designs that directly address this question. In the meantime it would seem reasonable to use the present findings to guide clinical practice. Thus the simpler focused form of the treatment, CBT-Ef, should perhaps be viewed as the default form as it is easier to learn and implement, with the more complex form, CBT-Eb, reserved for patients with marked additional psychopathology of the type that it targets.