The Impact of National Health Care Reform on Adults With Severe Mental Disorders
Abstract
Objective:
Method:
Results:
Conclusions:
Method
Data Sources
Data Analysis
Results
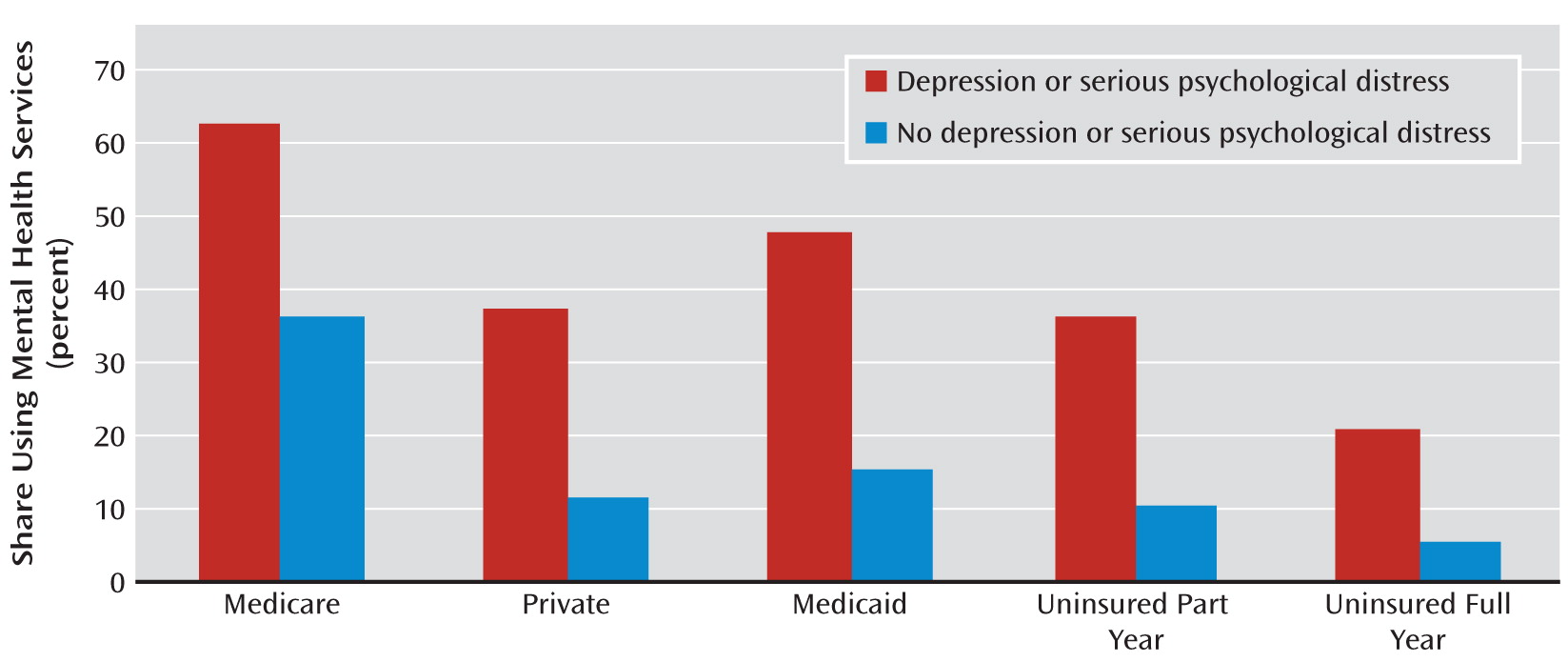
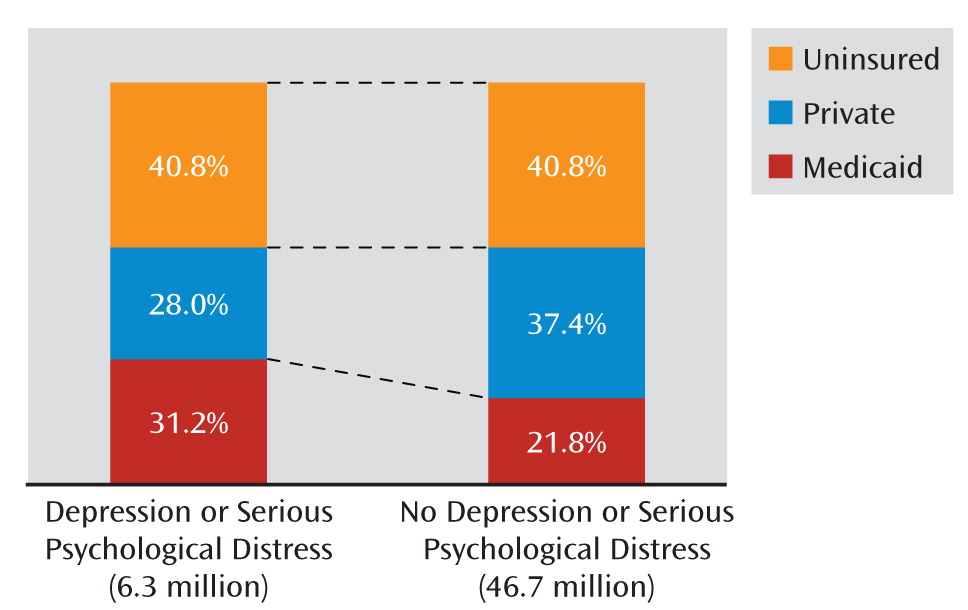
Current Income, Insurance Coverage, and Utilization
| Mental Health Status Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Probable Depression | Serious Psychological Distress | Depression or Serious Psychological Distress | Neither Depression Nor Serious Psychological Distress | Full Sample | |||||
| N | 95% CI | N | 95% CI | N | 95% CI | N | 95% CI | N | 95% CI | |
| Person-year observations | 5,351 | 3,199 | 5,880 | 45,200 | 51,080 | |||||
| Weighted population (1,000s) | 15,408 | 14,161–16,656 | 9,056 | 8,179–9,934 | 17,013 | 15,650–18,376 | 167,852 | 157,354–178,349 | 184,865 | 173,528–196,201 |
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Family income relative to federal poverty line | ||||||||||
| <133% | 40.8 | 38.7–42.9 | 46.9 | 44.4–49.3 | 40.7 | 38.7–42.7 | 17.7 | 16.8–18.6 | 19.9 | 19.0–20.8 |
| 133%–400% | 41.3 | 39.4–43.2 | 39.0 | 36.7–41.2 | 41.6 | 39.8–43.5 | 41.0 | 40.0–41.9 | 41.0 | 40.1–42.0 |
| >400% | 17.9 | 16.2–19.6 | 14.2 | 12.3–16.0 | 17.6 | 16.0–19.3 | 41.3 | 40.0–42.6 | 39.1 | 37.8–40.3 |
| Female | 57.8 | 55.9–59.8 | 59.4 | 56.7–62.2 | 58.0 | 56.0–59.9 | 50.0 | 49.5–50.5 | 50.8 | 50.2–51.3 |
| Race/ethnicity | ||||||||||
| Hispanic | 15.9 | 13.9–18.0 | 16.5 | 14.2–18.8 | 16.3 | 14.3–18.3 | 14.1 | 12.7–15.4 | 14.3 | 12.9–15.6 |
| Black | 15.7 | 13.7–17.7 | 14.3 | 12.1–16.4 | 15.5 | 13.5–17.5 | 11.9 | 10.7–13.0 | 12.2 | 11.1–13.3 |
| White | 62.6 | 59.9–65.4 | 64.4 | 61.3–67.6 | 62.5 | 59.7–65.2 | 68.3 | 66.6–70.1 | 67.8 | 66.0–69.5 |
| Other | 5.8 | 4.4–7.1 | 4.8 | 3.5–6.0 | 5.8 | 4.5–7.0 | 5.8 | 5.0–6.5 | 5.8 | 5.0–6.5 |
| Education | ||||||||||
| Less than high school | 28.9 | 26.9–39.0 | 31.7 | 29.2–34.1 | 29.0 | 27.1–31.0 | 15.7 | 15.0–16.5 | 17.0 | 16.2–17.8 |
| High school diploma | 36.9 | 34.9–38.9 | 36.6 | 34.0–39.2 | 36.6 | 34.7–38.5 | 30.5 | 29.6–31.5 | 31.1 | 30.2–32.1 |
| Some college | 20.5 | 18.8–22.3 | 20.4 | 18.1–22.6 | 20.8 | 19.1–22.5 | 24.6 | 23.8–25.4 | 24.2 | 23.5–25.0 |
| Bachelor's degree | 8.8 | 7.7–10.0 | 7.3 | 6.0–8.7 | 8.9 | 7.8–10.0 | 17.8 | 16.8–18.8 | 16.9 | 16.0–17.9 |
| Advanced degree | 4.0 | 3.2–4.8 | 3.1 | 2.3–4.0 | 3.9 | 3.2–4.7 | 10.8 | 10.1–11.5 | 10.2 | 9.5–10.8 |
| Census region | ||||||||||
| Northeast | 16.7 | 14.3–19.2 | 17.0 | 14.1–19.9 | 16.9 | 14.4–19.4 | 18.7 | 16.8–20.6 | 18.5 | 16.6–20.4 |
| Midwest | 20.2 | 17.9–22.6 | 20.5 | 17.6–23.3 | 20.2 | 17.8–22.6 | 22.4 | 20.3–24.6 | 22.2 | 20.1–24.3 |
| South | 40.4 | 37.4–43.5 | 40.1 | 36.8–43.4 | 40.0 | 37.0–43.0 | 35.6 | 32.7–38.6 | 36.1 | 33.2–38.9 |
| West | 22.6 | 18.9–26.3 | 22.4 | 19.0–25.9 | 22.9 | 19.2–26.6 | 23.2 | 20.1–26.3 | 23.2 | 20.1–26.2 |
| Metropolitan Statistical Area residence | 81.4 | 78.5–84.3 | 79.9 | 76.5–83.2 | 81.4 | 78.5–84.3 | 83.9 | 81.8–86.1 | 83.7 | 81.5–85.8 |
| Attitudes (disagree strongly or somewhat) | ||||||||||
| Healthy enough, don't need insurance | 85.9 | 84.8–86.9 | 88.2 | 86.8–89.6 | 85.7 | 84.7–86.8 | 79.8 | 79.2–80.5 | 80.4 | 79.8–81.0 |
| Health insurance not worth cost | 56.7 | 54.8–58.6 | 55.8 | 53.4–58.3 | 56.6 | 54.8–58.4 | 61.3 | 60.4–62.2 | 60.8 | 60.0–61.7 |
| Take more risks than average person | 55.9 | 53.9–57.9 | 55.6 | 53.3–57.8 | 55.8 | 53.9–57.6 | 60.7 | 60.0–61.4 | 60.2 | 59.6–60.9 |
| Overcome illness without medical help | 69.9 | 67.9–71.4 | 72.9 | 70.9–74.9 | 69.3 | 67.7–71.0 | 62.1 | 61.4–62.9 | 62.8 | 62.1–63.6 |
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| SF-12 Physical Health Summary | 43.2 | 42.6–43.8 | 41.5 | 40.8–42.2 | 43.3 | 42.8–43.9 | 52.1 | 52.0–52.3 | 51.3 | 51.1–51.4 |
| Age | 42.0 | 41.5–42.5 | 42.1 | 41.4–42.8 | 41.8 | 41.4–42.3 | 40.2 | 40.0–40.4 | 40.4 | 40.1–40.6 |
| Medicare Full Year | Private Full Year | Medicaid Full Year | Uninsured Part Year | Uninsured Full Year | Total Population, 2006 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental Health Status Group and Income Relative to Federal Poverty Line | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | N (1,000s) | |
| Probable depression | ||||||||||||
| <133% | 15.0 | 13.2–17.0 | 10.3 | 8.9–11.8 | 24.9 | 22.4–27.6 | 20.3 | 18.4–22.2 | 29.5 | 26.9–32.4 | 6,124 | |
| 133%–400% | 10.6 | 8.7–12.9 | 48.1 | 45.0–51.2 | 6.8 | 5.5–8.3 | 15.8 | 13.7–18.1 | 18.8 | 16.4–21.5 | 6,286 | |
| >400% | 6.1 | 4.3–8.6 | 78.6 | 75.0–81.8 | —a | —a | 8.0 | 6.0–10.7 | 6.7 | 5.0–9.0 | 2,998 | |
| All incomes | 11.6 | 10.4–12.9 | 38.1 | 36.2–40.1 | 13.1 | 11.7–14.5 | 16.2 | 15.0–17.6 | 21.0 | 19.3–22.8 | 15,408 | |
| Serious psychological distress | ||||||||||||
| <133% | 16.0 | 13.8–18.6 | 9.0 | 7.3–11.1 | 25.7 | 22.8–28.7 | 19.4 | 17.1–21.8 | 29.9 | 26.7–33.3 | 4,117 | |
| 133%–400% | 12.4 | 9.7–15.7 | 44.7 | 40.8–48.7 | 7.7 | 6.0–9.8 | 16.1 | 13.2–19.4 | 19.1 | 16.2–22.4 | 3,476 | |
| >400% | 10.8 | 7.3–15.6 | 73.8 | 67.7–79.1 | —a | —a | 7.8 | 5.1–11.9 | 7.3 | 4.8–11.0 | 1,464 | |
| All incomes | 13.9 | 12.2–15.7 | 32.1 | 29.8–34.5 | 15.1 | 13.4–16.8 | 16.4 | 14.9–18.1 | 22.5 | 20.4–24.7 | 9,056 | |
| Probable depression or serious psychological distress | ||||||||||||
| <133% | 14.7 | 13.0–16.6 | 10.8 | 9.4–12.4 | 25.2 | 22.8–27.8 | 19.9 | 18.2–21.7 | 29.4 | 26.9–32.1 | 6,701 | |
| 133%–400% | 10.4 | 8.6–12.7 | 48.0 | 45.1–50.9 | 6.6 | 5.4–8.0 | 16.1 | 14.1–18.3 | 18.9 | 16.6–21.4 | 7,107 | |
| >400% | 5.6 | 3.9–8.0 | 79.2 | 75.8–82.3 | —a | —a | 7.9 | 6.0–10.4 | 6.8 | 5.1–9.0 | 3,205 | |
| All incomes | 11.3 | 10.2–12.6 | 38.4 | 36.5–40.3 | 13.1 | 11.8–14.5 | 16.2 | 15.0–17.4 | 21.0 | 19.4–22.8 | 17,013 | |
| Neither probable depression nor serious psychological distress | ||||||||||||
| <133% | 5.2 | 4.7–5.8 | 21.2 | 19.9–22.6 | 16.2 | 14.8–17.6 | 19.2 | 18.1–20.4 | 38.1 | 36.5–39.8 | 29,922 | |
| 133%–400% | 1.8 | 1.5–2.0 | 62.8 | 61.5–64.1 | 2.6 | 2.3–3.0 | 13.9 | 13.3–14.5 | 18.9 | 17.8–20.1 | 68,078 | |
| >400% | 0.6 | 0.5–0.8 | 88.8 | 87.9–89.7 | —a | —a | 5.5 | 4.9–6.1 | 4.8 | 4.2–5.5 | 69,851 | |
| All incomes | 1.9 | 1.7–2.1 | 66.2 | 65.1–67.3 | 4.1 | 3.7–4.4 | 11.4 | 10.9–11.9 | 16.5 | 15.7–17.3 | 167,852 | |
Postreform Changes in Coverage
| Coverage | Users | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Postreform | Change | Baseline | Postreform | Change | |||||||
| Group and Coverage | N (1,000s) | % | N (1,000s) | % | N (1,000s) | % | N (1,000s) | % | N (1,000s) | % | N (1,000s) | % |
| Probable depression or serious psychological distress | ||||||||||||
| Medicare | 1,907 | 11.2 | 1,907 | 11.2 | 0 | 0.0 | 1,216 | 18.0 | 1,216 | 17.0 | 0 | 0.0 |
| Medicaid | 2,174 | 12.8 | 4,162 | 24.5 | 1,988 | 91.5 | 1,052 | 16.0 | 1,965 | 28.0 | 913 | 86.8 |
| Private | 6,674 | 39.2 | 8,391 | 49.3 | 1,717 | 25.7 | 2,550 | 39.0 | 3,122 | 44.0 | 572 | 22.4 |
| Uninsured part year | 2,729 | 16.0 | 1,113 | 6.5 | –1,615 | –59.2 | 998 | 15.0 | 407 | 6.0 | –591 | –59.2 |
| Uninsured full year | 3,530 | 20.7 | 1,440 | 8.5 | –2,090 | –59.2 | 759 | 12.0 | 310 | 4.0 | –449 | –59.2 |
| Total | 17,013 | 100.0 | 17,013 | 100.0 | 0 | 0.0 | 6,575 | 100.0 | 7,019 | 100.0 | 445 | 6.8 |
| Neither probable depression nor serious psychological distress | ||||||||||||
| Medicare | 3,182 | 2.0 | 3,182 | 2.0 | 0 | 0.0 | 1,169 | 6.0 | 1,169 | 6.0 | 0 | 0.0 |
| Medicaid | 6,843 | 4.0 | 17,292 | 10.0 | 10,449 | 152.7 | 1,089 | 6.0 | 2,471 | 13.0 | 1,382 | 126.8 |
| Private | 111,161 | 66.0 | 128,338 | 76.0 | 17,177 | 15.5 | 13,158 | 70.0 | 14,519 | 74.0 | 1,361 | 10.3 |
| Uninsured part year | 19,032 | 11.0 | 7,765 | 5.0 | –11,267 | –59.2 | 1,953 | 10.0 | 797 | 4.0 | –1,156 | –59.2 |
| Uninsured full year | 27,634 | 16.0 | 11,275 | 7.0 | –16,359 | –59.2 | 1,483 | 8.0 | 605 | 3.0 | –878 | –59.2 |
| Total | 167,852 | 100.0 | 167,852 | 100.0 | 0 | 0.0 | 18,853 | 100.0 | 19,561 | 100.0 | 709 | 3.8 |
| Full population | ||||||||||||
| Medicare | 5,089 | 3.0 | 5,089 | 3.0 | 0 | 0.0 | 2,385 | 9.0 | 2,385 | 9.0 | 0 | 0.0 |
| Medicaid | 9,017 | 5.0 | 21,453 | 12.0 | 12,437 | 137.9 | 2,142 | 8.0 | 4,436 | 17.0 | 2,295 | 107.1 |
| Private | 117,835 | 64.0 | 136,730 | 74.0 | 18,894 | 16.0 | 15,708 | 62.0 | 17,641 | 66.0 | 1,932 | 12.3 |
| Uninsured part year | 21,760 | 12.0 | 8,878 | 5.0 | –12,882 | –59.2 | 2,950 | 12.0 | 1,204 | 5.0 | –1,747 | –59.2 |
| Uninsured full year | 31,164 | 17.0 | 12,715 | 7.0 | –18,449 | –59.2 | 2,242 | 9.0 | 915 | 3.0 | –1,327 | –59.2 |
| Total | 184,865 | 100.0 | 184,865 | 100.0 | 0 | 0.0 | 25,427 | 100.0 | 26,581 | 100.0 | 1,154 | 4.5 |
Postreform Changes in Use
Discussion
Acknowledgments
Footnotes
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

