T
o the E
ditor: Drug-induced electrolyte disturbances have considerable implications. In our recent research dealing with this topic (
1), an association between hypocalcemia and drug treatment was noted in a small subset of risperidone users. We then retrieved all medical files in our psychiatry clinic and examined adult patients with at least one measurement of serum calcium, regardless of diagnosis/drug therapy, excluding those with obvious risks for electrolyte disturbances.
Finally, 1,320 record sets were derived from 1,245 patients (see the data supplement accompanying the online version of this letter). Risperidone users had more frequent incidence of hypocalcemia (≤2.1 mmol/l) (N=50/328) than comparison subjects (N=19/973) (odds ratio=9.21, 95% confidence interval [CI]=5.34–15.88, χ
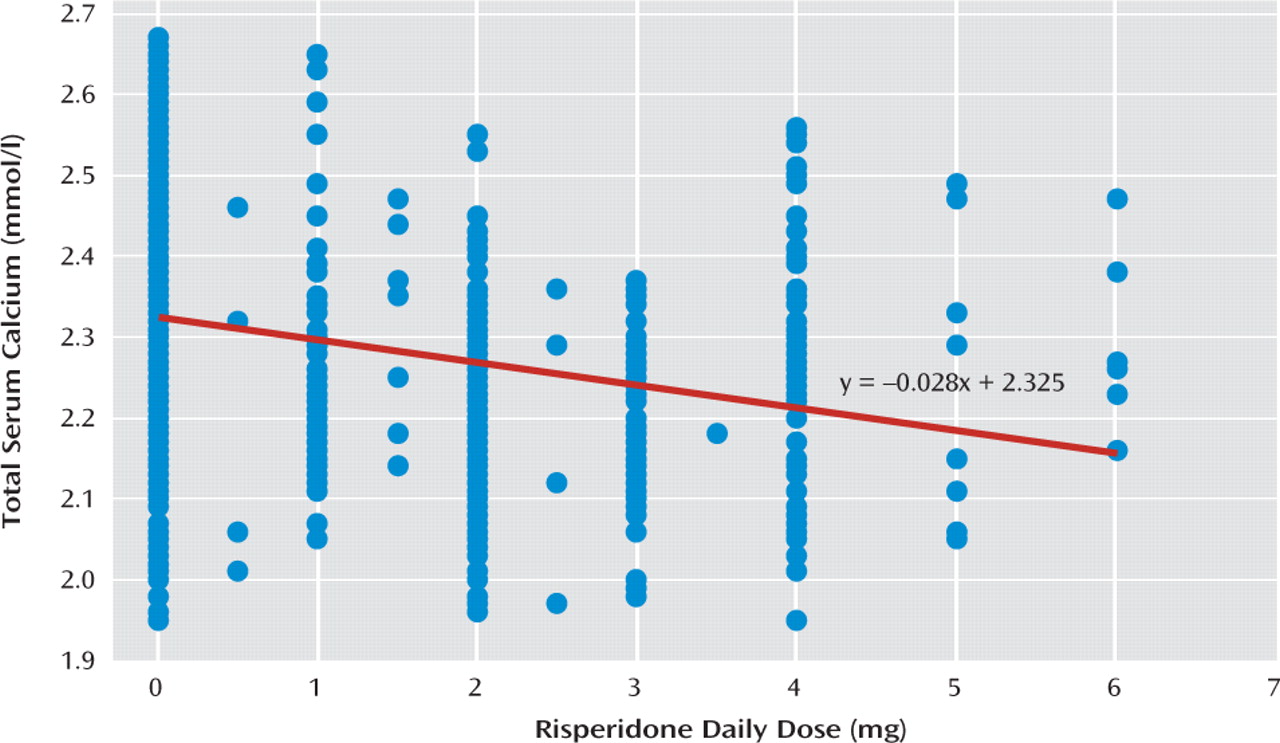
2=88.4, df=1, p<0.001). The mean calcemia level was significantly lower in the risperidone group (2.24 mmol/l [SD=0.13] vs. 2.33 mmol/l [SD=0.12], t=−11.7, df=1318, p<0.001). Additionally, there was significant correlation between the risperidone dose (mean daily dose: 2.5 mg [SD=1.2], 95% CI=2.4–2.8) and the serum calcium level (F=98.8, df=1, p<0.001; r
s=−0.299, p<0.001), with the lowest concentrations at approximately 3 mg (
Figure 1). Multivariable logistic regression, with confounders well-documented in the source data (age, gender, current drug treatment, data sets) (see the data supplement), confirmed independent association of risperidone and hypocalcemia (adjusted odds ratio=9.21, 95% CI=5.02–17.81, df=1, p<0.001). Both in the total number of hypocalcemic subjects (N=73) and in those with hypocalcemia within 99 percentiles (N=69), no significant association with any other study variable was found.
Presently, it is not known whether the association has causal relationships. In addition, our method does have some shortcomings (e.g., possibility of selection bias), although we utilized a fairly large sample size, with the finding being stable on different statistics. However, correlation of calcemia level with risperidone dose and literature data probably justifies additional research of possible causality. Risperidone, as well as other antipsychotics, can induce hyperprolactinemia and hypogonadism (
2), synthesis of calcium binding proteins in the tissues (
3), and changes in calcium-dependent signaling pathways (
4), which could cause a calcium-depleted state and/or trigger calcium redistribution within body compartments. Individuals treated with antipsychotics have small but variable risks of hip fracture (
5). With additional risks, even small disturbances of calcium homeostasis could make this population prone to osteoporosis and increase the probability of fractures.