Autism spectrum disorders (ASDs), characterized by pervasive impairments in social reciprocity and/or communication, stereotyped behavior, and restricted interests, have been the focus of debate in recent years, largely as a result of multinational reports of increasing prevalence (
1). Prevalence estimates range from 0.07% to 1.8% (
1–
6). The increased prevalence appears to be attributable to greater public awareness, broadening ASD diagnostic criteria, lower age at diagnosis, and diagnostic substitution (
7). Additionally, study design and execution have affected prevalence estimates, limiting the comparability of more recent estimates (
1,
8–
10).
This is the first population-based autism prevalence study in Korea. We targeted the entire elementary school population of a South Korean community, using both a general population sample and a group with a high probability of ASDs. Our study was designed to estimate ASD prevalence in different settings and to examine phenotypic variability along the autism spectrum.
Method
The study was approved by the Yale University and George Washington University institutional review boards.
Target Population
This study was conducted between 2005 and 2009 in the Ilsan district of Goyang City, South Korea, a stable, residential community near Seoul (area, 102 km2; population, 488,590) and representative of the general South Korean population (Korean Statistical Information Service, Capital Region Population, 2006). The target population (N=55,266) included all children born from 1993 through 1999 (ages 7–12 years at screening) and attending Ilsan elementary schools, as well as children in the same age group enrolled in the Ilsan Disability Registry between September 2005 and August 2006. Thirty-three of 44 elementary schools agreed to participate; 36,592 children were enrolled in participating schools and 294 in the Disability Registry (see section 1 of the data supplement that accompanies the online edition of this article). Investigators built collaborative community partnerships through ethnographic interviewing, meetings, and lectures (see section 2 of the online data supplement).
General-population sample students were in regular schools and classrooms, never received special educational services or psychiatric or psychological services, and were not in the Disability Registry. Children in the high-probability group were known to have special needs. They attended special education schools, used psychiatric or psychological services, or were listed in the Disability Registry. Sixty-two children from regular schools who completed assessments had histories of psychiatric or psychological service use and were counted in the high-probability group.
Participating families received screening results and a feedback session (see section 3 of the online data supplement).
Case Identification
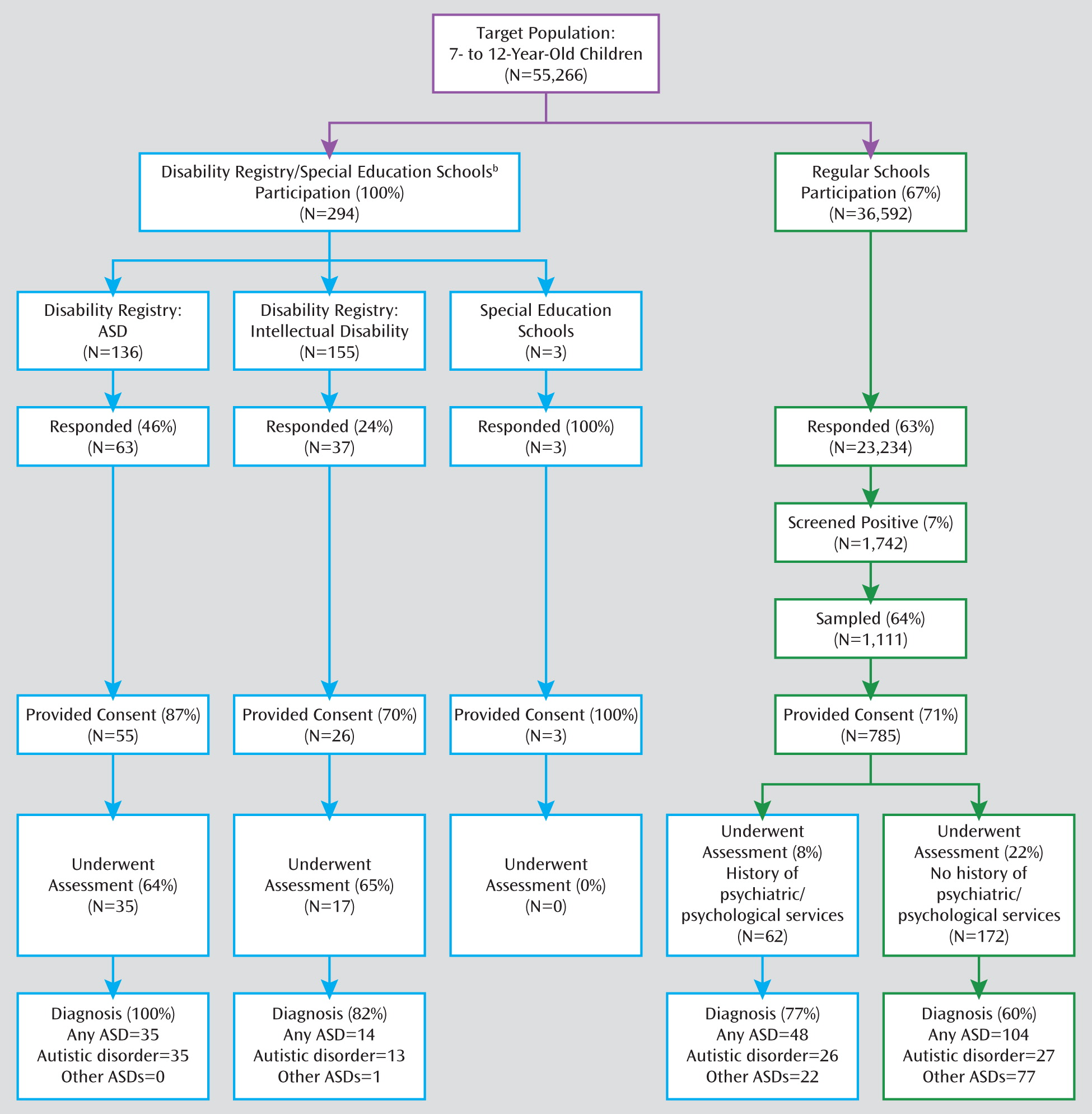
We used a two-stage design for case identification (
Figure 1). Stage 1 used systematic multi-informant screening with the Autism Spectrum Screening Questionnaire (ASSQ), a 27-item questionnaire assessing social interactions, communication problems, and restricted and repetitive behaviors (
15). In stage 2, screen-positive children were evaluated using standardized diagnostic assessments: the Autism Diagnostic Observation Schedule (ADOS), the Autism Diagnostic Interview–Revised (ADI-R), and cognitive tests that have been validated in South Korean children (see section 4 of the online data supplement) (
16–
18).
Procedure
The study proceeded in four steps: screening, sampling, diagnostic assessment, and quality control of best-estimate diagnoses.
Screening (September 2005–August 2006).
All parents were asked to complete the ASSQ. Additionally, teachers were asked to complete the ASSQ for all children who had any ASD characteristics, which were described in educational sessions led by the research team (see section 5 of the online data supplement).
The Disability Registry/special education schools target population included 291 children in the Disability Registry (136 categorized as having ASDs and 155 as having “intellectual disability”). Three additional children were in the special education schools category but not in the Disability Registry. All 294 children in the Disability Registry and in special education schools were considered ASD screen positive.
Children from regular schools were considered screen positive if they had a teacher-rated ASSQ score ≥10 or if their parent-rated ASSQ score was in the top 5th percentile of ASSQ score distributions (scores ≥14) from completed questionnaires.
Sampling.
All screen-positive children in the Disability Registry or in special education schools were invited to participate in confirmatory diagnostic evaluations; for this group, there was no sampling. Because we expected some ASD cases among children in the regular schools, we offered to evaluate those most likely to have ASDs, that is, those who screened positive on the teacher-rated ASSQ and all children in the top 2 percentiles of scores on the parent-rated ASSQ, plus a random sample of 50% of students in the 3rd percentile of scores on the parent-rated ASSQ and 33% of students in the 4th and 5th percentiles.
Diagnostic assessment (February 2006–July 2009).
Extensive efforts were made to contact parents of all screen-positive children who provided consent for diagnostic evaluations (N=869). Children whose parents could not be contacted were classified as nonparticipants. Diagnostic evaluations used the ADI-R, the ADOS, and cognitive tests (the Korean WISC-III and the Leiter International Performance Scale–Revised). Children were classified as having an ASD if they met DSM-IV criteria for any pervasive developmental disorder. To generate best-estimate clinical diagnoses, all relevant data, including ADOS and ADI-R scores, were reviewed by one of two clinical teams who were independent of the original evaluators. The final diagnosis was based on clinical judgment. Each team included a board-certified Korean child psychiatrist trained both in Korea and in the United States and a second board-certified child psychiatrist or child psychologist (team 1: Y.S.K./K.A.C.; team 2: Y.J.K./S.J.K.). Disagreements were resolved by consensus between diagnosing clinicians. For the small portion of cases (N=7; 2.4%) for which there was persisting disagreement, North American senior investigators with expertise in ASDs (E.F./B.L.L.) reviewed cases independently and unanimously agreed on diagnoses.
Confirmed ASD diagnoses met DSM-IV criteria and were classified as one of the following: any ASD (any pervasive developmental disorder), autistic disorder, or other ASDs (Asperger's disorder, pervasive developmental disorder not otherwise specified, Rett's disorder, or childhood disintegrative disorder).
Quality control of best-estimate diagnoses.
Best-estimate diagnostic reliability and validity were examined and maintained throughout the study. In a review of 49 randomly selected cases, agreement between Korean and North American assessment teams regarding the presence or absence of any ASD was 93.9%, with a kappa value of 0.75 (see section 6 of the online data supplement).
Cultural Considerations
We carefully addressed potential cultural biases in case identification. The team cultural anthropologist (R.R.G.) organized parent and teacher focus groups to identify local beliefs that might influence symptom reporting and to address stigma and misunderstandings related to ASDs (see section 2 of the online data supplement). The ASSQ, ADI-R, and ADOS were translated, back-translated, and validated for Korean children (see section 4 of the online data supplement). While screening was conducted with parent and teacher questionnaires and standardized diagnostic tools were used, we report best-estimate final clinical diagnoses that were validated by expert clinical judgment; this procedure protected against possible departures from the validity of instruments. To minimize possible cultural biases in diagnosis, each diagnostic team was composed of Korean diagnosticians with extensive clinical and research experience in both the United States and Korea. Moreover, a random sample of diagnoses (N=49) were validated by North American experts (B.L.L./E.F.) (see section 6 of the online data supplement).
Statistical Methods
There were missing data for the ASSQ because 1,414 parents (6.1%) completed only one page of the two-page form. Among completed ASSQ forms, first-page scores were highly correlated with second-page scores (r=0.72, p<0.001). Therefore, for the 1,414 incomplete ASSQ scores, values for missing data were imputed using the scores from completed pages in three different ways that produced highly correlated scores: simple weighted average, regression, and hot-deck imputation. The highest score was used as the primary imputed value to maximize screening sensitivity, yielding 264 screen-positive children. Sensitivity analyses were conducted to examine the impact of imputation procedures on prevalence estimates by using the high, low, and mean of three imputed ASSQ scores (see section 7 of the online data supplement).
The denominator used to compute ASD prevalence was the entire target population (that is, all 55,266 children ages 7–12 years in the study community) to reflect variance arising from nonparticipants (see sections 8 and 9 of the online data supplement). Prevalence estimates by sex and by ASD subtype in the total population, in the high-probability group, and in the general-population sample were computed using the Proc Frequency procedure in SAS, version 9.1 (SAS Institute, Cary, N.C.). Crude prevalence estimates (not adjusted for nonparticipants) were obtained.
Several strategies were used to adjust for missing data from screen-positive nonparticipants:
Adjustment by Disability Registry categories.
All nonparticipants with a Disability Registry-based ASD classification were assumed to have an ASD because every individual in the registry who had an ASD classification and who underwent diagnostic assessment had a confirmed ASD diagnosis (
Figure 1). Nonparticipants with a Disability Registry-based intellectual disability classification were considered noncases because no data supported an ASD diagnosis for those who did not undergo comprehensive assessments. Adjustment for nonparticipants from the Disability Registry added 101 ASD cases (91 boys and 10 girls).
Adjustment for nonparticipants in regular schools.
To account for missing data from screen-positive nonparticipants, we studied characteristics that might predict participation. We hypothesized that each child's parents have an unobservable score on a latent variable representing willingness to participate in diagnostic evaluations. Probabilities for consent and evaluation after screening positive, likely indicators of this latent construct, were modeled with logistic regression, using parent-rated ASSQ score and child's sex and age as predictors. ASSQ score was significantly positively associated with parental consent and with participation in the assessment, and male sex significantly predicted only parental consent. Predictive scores for each child who underwent assessment were obtained and used, together with parent-rated ASSQ score, sex, and age as covariates, to predict caseness. No indicators of the latent variable were significant predictors of caseness. Therefore, it is reasonable to infer that the probability of ASD diagnoses among children who were not definitively evaluated is no different from that for children who had full assessments. Hence, a simple proportional weigh-back procedure was used to compute prevalence estimates for the regular schools (see section 10 of the online data supplement).
Adjusted prevalence was computed in several steps:
1. Adjusted prevalence for children in the Disability Registry was computed using the number of children with ASDs as the numerator, adjusted for nonparticipants.
2. Among students in regular schools, adjusted prevalence for children with and without psychiatric or psychological service use was computed separately because of potential differences between the two groups with regard to the probability of completing the full assessment and having ASD diagnoses. Because we lacked accurate data on the proportion of psychiatric or psychological service use among children enrolled in regular schools, we performed sensitivity analyses to examine differences in prevalence stemming from three possible scenarios: the lowest, mid-range, and highest proportions of psychiatric or psychological service use. Prevalence with a mid-range proportion of psychiatric or psychological service use was used to determine final results.
3. A weigh-back procedure was conducted to achieve adjustment for sampling procedure in screen-positive children (see section 11 of the online data supplement).
4. Final adjusted prevalence: For the overall study population, final adjusted ASD prevalence was computed as the sum of adjusted prevalence among children in the Disability Registry, children from regular schools who did not have psychiatric or psychological service use, and children from regular schools who had psychiatric or psychological service use. For the high-probability group, final adjusted ASD prevalence was computed as the sum of the adjusted prevalence among children in the Disability Registry and those in regular schools who had psychiatric or psychological service use. For the general-population sample, final adjusted ASD prevalence was the adjusted prevalence among children in regular schools who did not have psychiatric or psychological service use.
Results
The parents of 23,337 children returned ASSQ forms; 103 were in the Disability Registry/special education schools group (35% response) and 23,234 were in regular-schools group (63% response). The sex and birth cohort distribution of the screened children is summarized in
Table 1; the mean ages of children at time of screening, by birth cohort year, are summarized in Table S2 in the online data supplement. Birth cohort distributions for children in the Disability Registry/special education schools and regular-schools groups were similar, with significantly more boys in the Disability Registry/special education schools (82% compared with 48%, p<0.001).
Teachers completed ASSQs for 314 children; children for whom teachers did not complete the ASSQ were considered screen negative on the teacher-rated ASSQ. For the 314 children with completed ASSQs, 94 were scored <10, which was considered a negative screen. Of the 220 with positive teacher-rated screens, 122 were screen positive by teacher reports only and 98 were screen positive by both parent and teacher reports.
For the 1,214 sampled screen-positive students, 869 parents (72%) consented to participate in the full assessment. Of these, 286 (33%) completed full assessments. Of those who completed the assessment, 201 (70%) were confirmed to have ASDs (autistic disorder, N=101; other ASDs, N=100), yielding a crude prevalence for any ASD of 0.36% (autistic disorder, 0.18%; other ASDs, 0.18%). There were no cases of Rett's disorder or childhood disintegrative disorder in those assessed.
In the high-probability group (those in the Disability Register, those in special education schools, and those in regular schools who had psychiatric or psychological service use) 97 of 114 children were confirmed to have autistic disorder (N=74) or other ASDs (N=23). The high-probability group contributes 0.18% for any ASD to the total population prevalence (autistic disorder=0.13% and other ASDs=0.05%; the ratio of autistic disorder to other ASDs was 2.6:1).
For 104 children with ASDs in the general-population sample, among the 172 assessed, the crude prevalence for any ASD was similar to that in the high-probability group (0.19%). However, the ratio of autistic disorder to other ASDs was reversed, with prevalences of 0.05% and 0.14%, respectively (ratio, 1:2.6) (
Table 2). Other differences between the high-probability and general-population groups included the ratio of boys to girls, which was 5.1:1 in the high-probability group and 2.5:1 in the general-population sample (p=0.037) (
Table 2). Mean performance IQ for individuals with any ASD was 75 (SD=28) in the high-probability group and 98 (SD=19) in the general-population sample (p<0.001) (see section 4.c of the online data supplement). In the general-population sample, 12% had superior IQs (≥120), compared with 7% in high-probability group. Fifty-nine percent of children in the high-probability group had intellectual disability, compared with 16% in the general-population sample (
Table 2).
Statistical adjustment for nonparticipants in the total population yielded an ASD prevalence estimate of 2.64% (
Table 3). The estimated prevalence of any ASD was 1.89% in the general-population sample and 0.75% in the high-probability group. Prevalences for ASD subtypes were 0.94% for autistic disorder and 1.70% for other ASDs; sex-specific prevalences 3.74% for boys and 1.47% for girls.
Sensitivity analyses were conducted to examine the robustness of the total population estimate using the lowest, the mean, and the highest of three methods as the imputed ASSQ score. Prevalence estimates of any ASD diagnosis ranged from 2.69% (95% confidence interval [CI]=2.20–3.18) to 2.74% (95% CI=2.25–3.24). Additional sensitivity analyses for lowest, mid-range, and highest proportion of psychiatric or psychological service use in the regular-schools group yielded prevalence estimates of any ASD ranging from 2.44% (95% CI=1.81–3.07) to 2.75% (95% CI=1.96–3.55). Both sensitivity analyses indicate that these differences are minimal, with a broad overlap of confidence intervals.
Discussion
There is a striking difference between our estimated prevalence of 2.64% for any ASD and previously reported estimates ranging from 0.6% to 1.8% (
1). We carefully examined possible reasons for this difference.
Although researchers have not found cultural variability in phenotypic expression of ASDs, cultural variables may affect prevalence estimates. Indications generally suggest ascertainment bias toward lower prevalence in South Korea since Koreans consider autism to be a stigmatizing hereditary disorder; autism (
chap'ae) impugns the child's lineage on both sides and threatens the marriage prospects of unaffected relatives. As a result, autism is often untreated, misdiagnosed as attachment disorder, or unreported in records (
8). Although our total population approach avoided clinical and administrative obstacles associated with stigma, it is possible that some parents, fearing a diagnosis, chose not to report ASD symptoms or to participate in diagnostic evaluations. To address cultural issues, focus groups conducted by our cultural anthropologist with parents, teachers, researchers, and clinicians did not identify cultural factors that biased ascertainment toward higher prevalence.
It is possible that our prevalence calculations overestimate prevalence as a result of a less-than-optimal participation rate in our general-population sample (63%). Typically, epidemiologic studies that are least subject to bias have a participation rate approaching 80%. Our survey weighting procedures assumed that participation at different stages of sample recruitment was not differentially related to ASD case status. However, it could be argued that in this cultural context, with few services for children with developmental disorders, parents of children with serious but unrecognized developmental problems would be more likely to participate in research than parents of unaffected children. Moreover, the fact that most children diagnosed in the study were previously unidentified argues against the hypothesis that stigma and fear of an ASD diagnosis served as a deterrent to participation. The survey may have provided welcome opportunities for parents and school professionals to gain new knowledge about children with obvious special needs but no officially recognized disability. Similarly, participation may have been higher in schools that had more students with ASDs.
We considered the possibility that employing instruments designed for North American populations might introduce cultural biases. The Korean team performed translations and back-translations as well as standardization of screening and diagnostic instruments. Final best-estimate clinical diagnoses were made by Korean-North American diagnostic teams, based on standardized assessments and international diagnostic criteria. The agreement between the best-estimate clinical diagnoses and the diagnoses generated from the screening cutoff score and the ADOS and ADI-R diagnostic algorithm was good (64%–84%; data not shown) and was comparable to that in studies conducted in other countries (
16,
17,
19–
23). Such agreement suggests that cultural biases did not affect case identification and final caseness determination, a finding consistent with the experiences of investigators using the tools employed in this study in other cultures and reporting no adjusted cut-offs or changed algorithms.
Our prevalence estimates derive from examination of two distinct subgroups of the total population: a high-probability group and a general-population sample. The inclusion of the general-population sample contrasts with primarily high-probability group targets of most previous studies reporting ASD prevalence estimates. General-population samples have been inconsistently surveyed in previous studies, for various reasons: they are less accessible than clinical (high-probability group) samples; there are trade-offs between the requirement of a very large sample and the expected low yields of ASD cases; studies of general-population samples are generally not seen as cost-effective; and there is no accepted methodology for screening ASDs in general-population samples. Our total population study employed rigorous outreach and screening in an attempt to obtain an unbiased sample that included as many children as possible in the community.
Our high-probability group prevalence estimate of 0.75% is in the lower range of previous ASD prevalence estimates, and the ASD clinical characteristics of the children in this group were similar to those reported in previous studies that largely targeted high-probability samples (
3).
Our finding of a higher ASD prevalence appears to be attributable to the general-population sample component, in which the prevalence was 1.89%. A few studies have included toddlers from general-population samples in the screening stage, but sample sizes were small, and ASD diagnoses are less reliable in this age group (
24–
27). Additionally, the prevalence estimate validity in a U.K.-based total population study was compromised by low participation rates (<30%) (
28,
29). Posserud et al. (
30) used the ASSQ in a two-stage total population design and reported a prevalence of 0.87%, but their study differed from ours in three ways: the screening cutoff score was the upper 2nd percentile, compared with the upper 5th percentile in our study; investigators did not use the ADOS and ADI-R for final diagnoses; and their sample was one-fourth the size of ours. In our study, 54% of children in upper 3rd–5th percentile screen-positive ranges were confirmed to have ASDs, in addition to 71% of children in the upper 1st–2nd percentile screen-positive ranges. Along with differences in the diagnostic assessment tools and sample size, these data suggest that the higher screening cutoff score in the Posserud et al. study (
30) may have led to lower sensitivity in case identification and a lower ASD prevalence.
We examined the striking finding that many of the children in our study were in regular schools, without having been diagnosed and without support. It is possible that higher-functioning Korean children with ASDs manage in mainstream classrooms because of the nature of South Korean education, in which the school day exceeds 12 hours, 5–6 days a week. Teaching is highly structured, with much behavioral regulation, in settings where socialization is subordinated to educational progress (
31; Ministry of Education, Science, and Technology, Education Statistics, 2007). For quiet, high-functioning children with ASDs, this environment may reduce the likelihood of referrals to special education programs. Therefore, it was especially important for our study to screen “mainstream” school populations; our screening of children in regular schools found a relatively high proportion of cases in the general-population sample.
Finally, our findings are consistent with current research suggesting a dimensional distribution of “autistic traits” throughout the general population (
32,
33). The clinical characteristics of general-population sample children with ASDs differed from those of children with ASDs in the high-probability group; the former had higher cognitive abilities and a lower male predominance. Differences between the high-probability and general-population groups may be crucial for understanding the full range of autism spectrum characteristics and for proper phenotyping in etiologic and treatment studies.
Our study highlights the importance of methodology in determining prevalence estimates. Previous studies have varied enormously in the methods associated with multistage case identification designs, study populations, survey areas, screening, participation, and quality of confirmative diagnoses; each factor may have led to different prevalence estimates in each study (
1,
9,
10). Our study emphasizes the importance of proactive screening of all children in target populations to maximize the sensitivity of case identification and to reduce bias in prevalence estimates. Our experience suggests that the application of validated, reliable, gold-standard screening procedures and diagnostic methods in other total population samples is possible, and we believe it will strengthen the design of future prevalence surveys.
Limitations of this study include the relatively small proportion of children in the whole sample who received a full diagnostic assessment. This is a ubiquitous problem in similar epidemiologic studies (
34). In order to model parent participation in the survey, we hypothesized a latent variable reflecting parental willingness to participate in further diagnostic assessment after a positive screen. In addition, the conservative approach of considering nonparticipants from the Disability Registry's intellectual disability category as noncases may have resulted in an underestimation of ASD prevalence in the high-probability group. Because not all children were evaluated, the proportion of psychiatric or psychological service use in the total group of children in regular schools can only be estimated, adding modest uncertainty to the prevalence estimates. Moreover, our prevalence estimates were based on the assumption that we identified all ASD cases in the study population; yet, we may have missed cases among screen-negative children, thus underestimating prevalence. Lastly, although we found a significant group of children with ASDs who were functioning at various levels in the general population while not receiving services, the general-population sample may vary qualitatively and quantitatively in different cultures and communities.
While replication of our findings in other populations is essential, we conclude that the application of validated, reliable, and commonly accepted screening procedures and diagnostic criteria in a total population may yield an ASD prevalence exceeding previous estimates. Hence, we report an ASD prevalence estimate in the range of 2%–3% with due caution about the risks of over- and underestimation.