Case Presentation
“Ms. H,” a 29-year-old woman, presented to the emergency department with epigastric distress 2 hours after intentionally ingesting ethylene glycol in an admitted suicide attempt. After being stabilized, she was admitted to the inpatient psychiatric service.
Ms. H reported 3 weeks of depressed mood, anhedonia, decreased appetite with subjective weight loss of 7 lb, insomnia, decreased energy, and thoughts of suicide. She denied manic and psychotic symptoms. She denied any family history of suicide but reported that her mother had experienced episodes of depression. On the night before her presentation, she reported drinking eight beers, ingesting the various pills in her cousin's medicine cabinet, and falling asleep with the hope of death. When she awoke the next morning, she returned to her apartment, smoked marijuana, and attempted suicide with ethylene glycol.
She denied ever using cocaine, hallucinogens, heroin, or methamphetamine. Her urine drug screen on admission was positive for amphetamines; she attributed this to the medications in her cousin's medicine cabinet. She reported three to four binge drinking episodes annually but denied symptoms of alcohol abuse or dependence.
Ms. H denied episodes of depression before her first use of marijuana at age 18. By age 23, she was smoking two to three joints daily. She made her first suicide attempt at age 23 by acetaminophen overdose; she was admitted to a community hospital, where she was diagnosed with major depressive disorder, but she never received treatment after discharge. Ms. H said that marijuana relaxed her and made her “less worried” but interfered with her work as a massage therapist. Ms. H discontinued weekday use at age 24 but continued to smoke marijuana on weekends until early 2010, when she obtained her medical marijuana license. She reported that from February 2010 until her suicide attempts 7 months later, she smoked at least a joint of marijuana daily, and she doubled her use in the month preceding her suicide attempt.
Ms. H acknowledged the temporal association between her suicide attempts and episodes of increased marijuana use, but she was precontemplative about abstinence. She was referred to an outpatient substance abuse program, but declined to attend, saying, “Marijuana is prescribed by a doctor, so I don't think it's a problem.” She was discharged to her father's home with a prescription for 20 mg/day of citalopram and an appointment with a primary care provider.
Diagnosis
Ms. H drank to excess during the evening before ingesting ethylene glycol. However, she did not experience alcohol withdrawal and denied legal or interpersonal problems related to alcohol. While she was advised to address her binge drinking, there was no evidence that alcohol directly caused her depression.
Ms. H acknowledged that her primary substance use was with marijuana, first for a decade as a recreational drug and then for the 7 months preceding her suicide attempts as a registered medical marijuana user. She acknowledged that it now took escalating amounts of marijuana for her to feel relief, that she often used more than she intended to, and that marijuana use interfered with her occupational and social life. Her self-admitted periods of heaviest marijuana use were temporally associated with depressive episodes and suicide attempts, and she identified an additional episode of depression while smoking marijuana only on weekends.
While the possibility that she was experiencing a substance-induced mood disorder with depressive features could not be definitively excluded, Ms. H was diagnosed with major depressive disorder, recurrent, severe without psychotic features, and cannabis dependence.
Marijuana and Mental Illness
The associations between marijuana use and mental illness are numerous. In the United States, marijuana is the most frequently abused illicit substance, with over 16.7 million Americans reporting past-month use (
1), and it is identified as the primary substance of abuse in 17.1% of substance treatment admissions (
2). A growing body of evidence associates marijuana use with an earlier onset and more adverse course of psychotic disorders (
3).
What is less well known is that longitudinal studies associate marijuana use with depression. While infrequent marijuana use does not appear to be associated with depressive disorders (
4), the medicalization of marijuana encourages regular use, and regular use has a modest but significant association with depression that endures even after controlling for possible confounders. A recent prospective cohort study of 7,735 adults with no history of anxiety or mood disorders (
5) found that adults who used marijuana at the beginning of the 3-year study period were at an increased risk of having a first depressive episode (odds ratio=1.62, 95% CI=1.06–2.48) in comparison to nonusers, and this association was stronger with more frequent use. Animal models have found that both activation and blockade of the endocannabinoid system can lead to depression (
6).
Ms. H says she smoked marijuana before ingesting ethylene glycol in part to “steady” herself for her suicide attempt. This statement is intriguing, because while acute intoxication can induce euphoria, several studies have found a robust association between frequent marijuana use and suicidality, often in the absence of depression (
7–
9). A longitudinal study (
10) that followed a cohort of 2,033 Norwegians over 13 years from late adolescence into their late twenties found a significant association between using marijuana one to 10 times by age 21 and suicidal ideation by age 27 (odds ratio=2.4, 95% CI=1.3–4.3) after controlling for confounding factors such as conduct disorder, parental divorce and unemployment, school performance, and alcohol and nicotine use. Among those who had used marijuana 11 or more times by age 21, the researchers identified a significant association between both suicidal ideation (odds ratio=2.7, 95% CI=2.8–6.4) and suicide attempt (odds ratio=2.9, 95% CI=1.3–6.1) by age 27. Growing evidence associates hyperactivity of the endocannabinoid system with impulsivity and suicidality; for example, postmortem studies have found up-regulated cannabinoid receptors in the prefrontal cortex of individuals who died by suicide (
6). For someone like Ms. H, using marijuana may both relieve acute distress and increase the long-term risk of suicide and depression through chronic activation of the endocannabinoid system.
Medical Marijuana in Colorado
While medical marijuana has been legal in California since 1996, its widespread use began in March 2009, when the federal government announced that it would not prosecute medical marijuana users and distributors in states where the medical use of marijuana is legal (
11). At the time of this writing, the District of Columbia and 14 states, including Colorado, have legalized medical marijuana (
12).
In November 2000, the Colorado electorate passed Amendment 20 with 54% of the vote (
12). Amendment 20 legalized the possession of marijuana by a person diagnosed with a “serious or chronic illness” whose doctor will attest that he or she “might benefit from medical use of marijuana” (
www.cdphe.state.co.us/hs/medicalmarijuana/amendment.html). The qualifying conditions are cancer, cachexia, HIV/AIDS, glaucoma, epilepsy, muscle spasms, severe nausea, and severe pain. As of September 2010, the state had 809 dispensaries—licensed stores that sell marijuana to registered users—which constituted more than a third of the nation's 2,192 dispensaries (
12).
The Colorado Department of Public Health and the Environment (CDPHE) compiles data on the age, gender, and qualifying condition of individuals registered for medical marijuana use; the number of physicians recommending marijuana; and the conditions for which physicians recommend marijuana. In the applications processed by the CDPHE, the average age of registrants is 40 years, and 71% of registrants are male. From 2000 through 2008, 8,957 people in Colorado registered to use medical marijuana. By June 2010, this figure had increased to an estimated 99,559 (Colorado Department of Public Health and Environment, private communication, December 2010). Approximately 2% of the state's population is now registered to use medical marijuana, and on a per capita basis, Colorado has twice as many medical marijuana users as California (
12). Medical marijuana registration is highest in Colorado's ski counties, where median income and education levels are highest (
13).
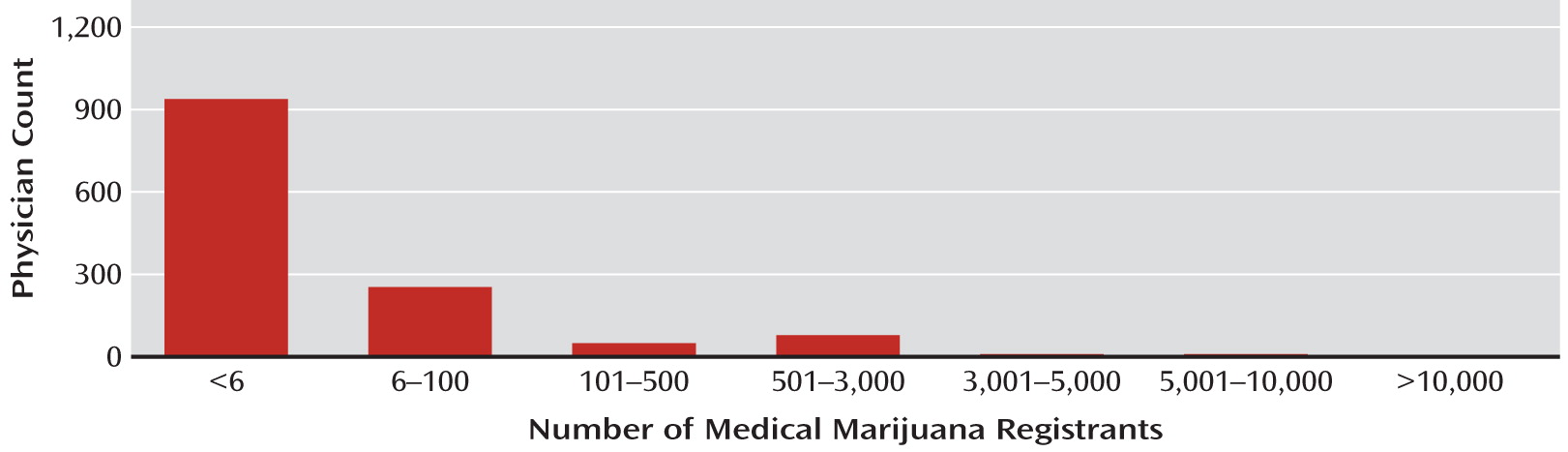
CDPHE data indicate that as of December 2010, 1,246 doctors have signed the medical marijuana registry forms the department has processed, which is approximately 9% of Colorado's licensed physicians. However, the practice has largely been limited to a small coterie of physicians, as illustrated in
Figure 1.
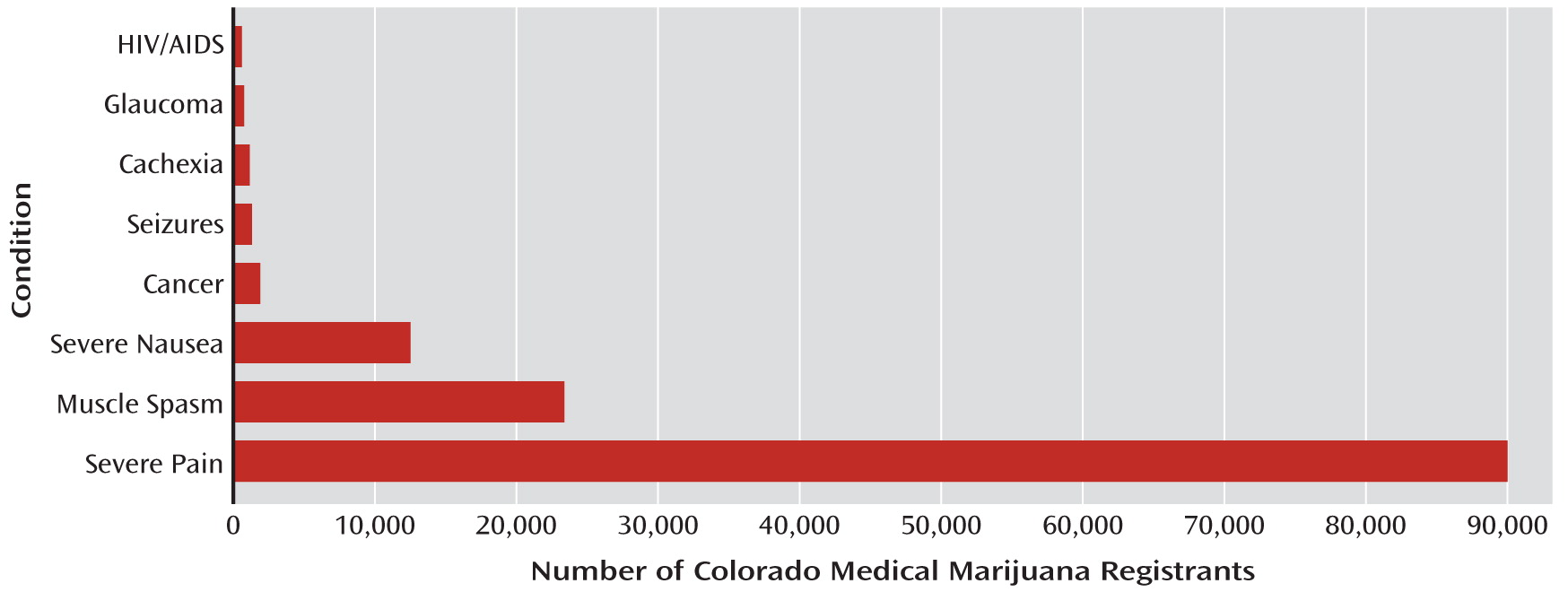
In the applications processed by the CDPHE, 94% of Colorado medical marijuana registrants are qualified for severe pain.
Figure 2 enumerates the medical conditions for which users are qualified to take medical marijuana; note that users can be qualified for more than one condition.
Like the majority of medical marijuana users in Colorado, Ms. H was licensed to use marijuana for severe pain. In fact, studies of cannabinoid-mediated analgesia suggest benefit for neuropathic pain in multiple sclerosis. Investigators are interested in designing peripheral cannabinoid agonists to treat pain syndromes, but the available literature is limited by small sample sizes, heterogeneous populations, subjective outcome measures, difficulty maintaining the study blind, and variable concentrations of cannabinoids in smoked marijuana (
14). Ms. H identified her own pain as daily headaches that developed after her husband struck her in the head during a domestic dispute that occurred 6 months before she registered to use medical marijuana. She was not asked about the cause of her headaches when she registered.
Treatment of Cannabis Dependence
The treatment of cannabis dependence and withdrawal remains nonspecific. When withdrawing from marijuana, users can experience a variety of symptoms, including anger, anorexia, craving, dysphoric mood, insomnia, irritability, and restlessness. Symptoms begin within a day of discontinuing marijuana, peak approximately 5 days after discontinuation, and extend for 1 to 3 weeks (
15). While many psychotropic agents have been studied for the treatment of cannabis dependence, greater efficacy has been demonstrated with behavioral psychotherapies, especially motivational interviewing, cognitive-behavioral therapy, and contingency management. Marijuana-specific manuals exist for these interventions. The best practice remains behavioral psychotherapy alongside treatment of co-occurring mental health and substance use conditions (
16).
Ms. H received citalopram to target depressive symptoms and as-needed doses of hydroxyzine and trazodone to ameliorate insomnia, irritability, and restlessness. The treating psychiatrist employed motivational interviewing techniques with Ms. H, expressed empathy for her many psychosocial stresses, and attempted to develop a discrepancy between her desire to continue using cannabis and its association with her two suicide attempts.
Discussion
As Ms. H's case illustrates, the rapid expansion of medical marijuana use raises concerns about the psychiatric complications of marijuana use, the relationship between patients and physicians, and the need for additional services and research.
The use of medical marijuana in the context of mental illness or substance abuse can be dangerous. While we cannot directly attribute Ms. H's two suicide attempts to marijuana use, the association between her increased use of marijuana and her suicide attempts is concerning, especially given the growing concern that frequent marijuana use is associated with suicide. This is especially concerning in Colorado, where the CDPHE recorded 940 suicides in 2009, a suicide rate of 18.4 deaths per 100,000 residents, the highest rate in Colorado since 1988 and nearly twice the national average (
17). Medical marijuana systems should attempt to identify not only the people who might benefit from medical marijuana but also those who might suffer from its use.
Amendment 20 does not require a laboratory, mental, physical, or other examination, only a physician's signature indicating that the user has a debilitating medical condition that “may be alleviated by the medical use of marijuana.” Ms. H saw the referring doctor only a single time and reports that she did not receive a physical examination. Until recently, physicians recommending marijuana were not required to seek or review the person's medical, substance use, or psychiatric records; to be available if complications arose; or to coordinate care with other physicians treating the patient. Permission to possess and use marijuana is excluded from the state's Prescription Drug Monitoring Program, which reports all other prescriptions for controlled substances.
Finally, Ms. H's case shows our need for rigorous investigations into the effects of marijuana on medical and psychiatric conditions, especially its association with impulsivity and suicidality. The medical marijuana industry, a system that encourages chronic and frequent use of marijuana, has expanded dramatically, and the ways in which this development will alter patterns of marijuana use and abuse remain unclear.