An extensive literature has documented an elevated risk of medical morbidity and early mortality among individuals with mental illnesses (
1,
2). Although this problem was first described nearly a century ago (
3), it has only recently become a major focus of mental health advocacy and policy efforts (
4).
For many patients with serious mental disorders, the primary point of contact with the health care system is through public-sector mental health programs rather than primary medical care. There has been a growing interest in developing “specialty care medical homes” for managing medical care for this population in community mental health settings (
5). Care management, in which staff provide education, advocacy, and linkages to community-based medical services, is a potentially promising approach to delivering care to this population, given its flexibility and its relatively low cost (
5). However, there are currently few evidence-based models for delivering that care (
6,
7).
The Primary Care Access, Referral, and Evaluation (PCARE) study is a randomized trial of a medical care management intervention for persons with serious mental illnesses treated in community mental health settings. Our group previously reported (
8) that the intervention improved the quality and outcomes of primary medical care at 1 year.
In this article, we report on costs for each year and 2-year outcomes of this intervention. Costs are presented from two vantage points: a health system perspective (which is most relevant to policy makers) and a managerial perspective (which is most relevant to clinic directors considering implementing medical care management for persons with mental illnesses). The goals of the study were to assess clinical sustainability (whether 1-year improvements were maintained) and financial sustainability (whether the intervention provided value from a health system perspective and was sustainable under routine funding conditions).
Method
Details of the PCARE study design and intervention have been described previously (
8). They are briefly outlined here to provide context for the 2-year outcome and cost data.
Study Setting
The study was conducted in an urban community mental health center (CMHC) in Atlanta. The target population was individuals age 18 and older from the area who were economically disadvantaged and who had serious and persistent mental illness with or without comorbid substance use disorders. With the exception of the study intervention, the clinic did not provide any formal medical or mental health care case management or any on-site medical care.
Recruitment
The sample was assembled through flyers posted at the CMHC, waiting room recruitment, and provider referrals; about one-third of potential participants were identified through each of the three approaches. To be eligible, individuals had to be on the active patient roster at the CMHC, have a severe mental illness (
9), and have the capacity to provide informed consent. Inclusion criteria were kept broad to optimize generalizability to community mental health settings.
Randomization and Follow-Up
A computerized algorithm was used to randomize assignment of patients to the intervention or usual care group. After randomization, interviews were conducted every 6 months throughout the course of the study. Interviewers were blinded to participants' group assignment. Annual chart reviews were used to gather data for calculation of quality measures.
Intervention
Two full-time registered nurses provided care management activities combining patient education and activation and logistical support in obtaining access to ongoing comprehensive primary care services. Each care manager had a caseload of approximately 75 patients at any given time, each of whom had an initial intake visit followed by monthly follow-up visits.
Care managers enhanced activation using motivational interviewing techniques (
10) and action plans (
11), which set and tracked short-term achievable goals for medical care or lifestyle change. Coaching was provided to patients to help them interact more effectively with their providers. With the participant's permission, providers were notified about changes in the patient's medication regimen and medical status. The care manager worked to helped clients overcome barriers to attending medical appointments.
Usual Care
Participants assigned to the usual care condition were given a list with contact information for local primary care medical clinics that accept uninsured and Medicaid clients. Participants in the usual care condition were not restricted in the medical care or other services that they sought.
Measures
An interview battery administered at baseline and then every 6 months throughout the study was used to identify sites where patients had received medical or mental health services as well as to collect clinical data. Reviews of all medical and mental health charts from these sites at baseline, 12 months, and 24 months assessed quality of preventive and cardiometabolic care and health service use.
Quality of primary care was assessed at baseline and 12 months using 23 indicators drawn from the U.S. Preventive Services Task Force guidelines (
12). For patients with a cardiometabolic condition (diabetes, hypertension, hypercholesterolemia, or coronary artery disease), quality indicators were drawn from chart reviews using the RAND Community Quality Index study (
13). For both of these sets of quality indicators, an aggregate indicator was created that represented the proportion of services the patient actually received from among those for which he or she was eligible.
Health-related quality of life was assessed using the 36-item Short-Form Health Survey developed for the Medical Outcomes Study (
14,
15). Physical component summary and mental component summary scores can be constructed from the survey, ranging from 0 (poor health) to 100 (perfect health) (
16). The oblique method, which is the preferred approach when examining persons with comorbid physical and mental conditions (
17,
18), was selected a priori as the approach for calculating the summary scores. Individual subscales were also calculated to provide context for these summary scores (
19).
For patients with available fasting laboratory values, the Framingham cardiovascular risk index was used to estimate the 10-year risk of developing cardiovascular disease.
Intervention Costs
Staff costs for the nurse care managers were calculated using data from the Bureau of Labor Statistics on median salaries for registered nurses (
20). A mean fringe rate of 29% for benefits was included based on national averages for nurses employed in public-sector facilities (
20). Training costs were calculated based on daily salaries and fringe rates for the senior staff providing training.
Equipment costs were divided into one-time setup costs (e.g., examination table, sphygmomanometer, scale) and recurring expenses (e.g., gloves, bandages). All prices were drawn from the national medical supply company where the products were purchased.
A rate of 15% was applied to all intervention expenses to account for clinic space and administrative support (
21).
Costs From the Health System Perspective
A cost analysis was calculated from the health system perspective using standard approaches from the cost-effectiveness literature (
22–
24). The quantity of each type of health service (mental and medical outpatient, emergency, and inpatient) was drawn from chart review data from each site where participants obtained services. Unit costs were assigned to each service type based on median national expenditures for each type of service from the 2007 Medical Expenditure Panel Survey (
25). This survey is well suited for assessing unit costs from a health system perspective because it uses direct payments, not charges, and captures costs across all insurance groups. All expenditures for each type of service were inflated to 2010 dollars.
Given initial expenditures in setting up a new program, costs were examined separately for each of the 2 years of the study. Costs for each intervention visit were calculated by applying the hourly intervention cost, based on staff salaries, fringe benefits, equipment, and overhead, to each visit.
Costs From a Managerial Perspective: Budget Impact Analysis
A budget impact analysis involves a careful accounting of the costs of implementing a new program, coupled with the expected returns (
26,
27). The methods we used followed the approach proposed by the International Society for Pharmacoeconomics and Outcomes Research Task Force on Good Research Practices (
28). In contrast to cost-effectiveness analyses, budget impact analyses adopt a managerial rather than societal perspective and have a shorter-term horizon.
For the budget impact analysis, only services provided at the CMHC were considered. Medicaid reimbursement rates were calculated based on 2010 payment rates for clinical nurse visits from Georgia's Medicaid program. As with the health system-level analysis, intervention expenditures were treated as positive costs. However, individual visit reimbursements were treated as negative expenditures (i.e., revenues).
As is typical of CMHCs (
29), nearly all clients at the study site either had Medicaid or were uninsured. Costs for uninsured clients were covered by capitated annual state block grants provided to the clinics. Medicaid services were reimbursed on a fee-for-service basis for each visit. Under varying case-mix scenarios, we calculated a break-even point where the total reimbursement offset the costs of funding the care management service during the first year.
Statistical Analysis
All analyses were conducted using the intent-to-treat approach. Two-year clinical outcome analyses were conducted using random regression to calculate the relative difference in change over time. For each outcome measure, the model assessed the outcome as a function of randomization group, time since randomization, and group-by-time interaction. The group-by-time interaction, which reflects the relative difference in change in the parameters over time, was the primary measure of statistical significance.
To mitigate the potential impact of missing data from interviews, we performed multiple imputation by a Monte Carlo Markov Chain approach to impute missing scores for interview data. The covariates used in multiple imputation were age, gender, race, psychiatric diagnosis, medical comorbidity, and SF-36 scores for the eight domains at baseline, 6 months, 12 months, 18 months, and 24 months.
We used bootstrap analysis to generate 95% confidence intervals (CIs) and to estimate the probability that total health care costs were lower in the intervention group than in the usual care group (i.e., a “cost offset”) for each cost category. Bootstrap analysis was conducted by constructing 1,000 samples from the study data set and, for each one, computing the difference in mean costs (defined as the mean for participants in the intervention group minus the mean for participants in the usual care group). The 95% confidence interval was then derived from the resulting distribution of differences in mean costs across the 1,000 bootstrap samples. The probability of a cost offset was estimated by dividing the number of bootstrap samples in which the intervention group had lower health care costs than the usual care group by 1,000.
Initial analyses indicated that cost data were highly non-normally distributed. Removing extreme outliers (the 3% of the sample beyond three standard deviations above or below the mean) substantially improved the normality of the distribution. Confidence intervals and probability of cost offset were computed both with and without inclusion of these extreme outliers.
Results
A total of 407 patients provided informed consent and underwent randomized assignment to either the medical care management intervention or usual care. Of those assigned, 68.1% completed interviews at 12 months and 55.8% completed interviews at 24 months. Complete 12-month chart review data were available for 89.2% of the sample, and complete 24-month chart review data for 79.1% (see Figure S1 in the data supplement that accompanies the online edition of this article).
Baseline Characteristics
Table 1 summarizes participants' demographic and clinical characteristics. The sample was predominantly African American (77.9%) and poor (median annual income, $3,400). A total of 40% had Medicaid coverage, 59% were uninsured, and 1% had private insurance. The most common psychiatric diagnoses were schizophrenia (42.8%), depression (32.7%), and bipolar disorder (17.2%). A total of 25.3% of the sample had a comorbid substance use disorder. The most common medical comorbidities were hypertension (45.6%), arthritis (36.6%), tooth/gum disease (25.6%), asthma (20.1%), and diabetes (17.9%). There were no significant differences between the groups in any of the demographic or diagnostic characteristics at baseline.
Two-Year Clinical Outcomes
Table 2 summarizes results of the quality and outcome measures during the first 2 years. Overall, the gains in quality and outcomes of care at 1 year persisted at 2 years. The total proportion of preventive services for which a client was eligible that were received by the client (primary outcome measure) more than doubled between baseline and year 1 and remained highly significant by year 2 (56.2% compared with 17.4%, p<0.001 for group-by-time interaction). Among the subset of individuals with cardiometabolic diagnoses (diabetes, hypertension, high cholesterol, heart disease), the proportion receiving guideline-concordant cardiometabolic care increased in the intervention group from 28.2% to 43.5%, while declining slightly in the usual care group (31.5% to 27.8%), resulting in a significant group-by-time interaction (p<0.001).
Over the 2-year follow-up period, there was a significantly greater improvement in the mental component summary of the 36-item Short-Form Health Survey for the intervention group than for the usual care group (4.1 points compared with 3 points, p<0.001 for the group-by-time interaction). The relative improvement on the physical component summary of the Short-Form Health Survey was smaller and not statistically significant (2 points compared with 1.3 points). Significant improvements, as reflected in significant group-by-time interactions, were seen in the physical functioning, pain, role-emotional, social functioning, general health, and mental health subscales (all p values <0.001) (see Table S1 in the data supplement that accompanies the online edition of this article).
Among patients for whom fasting blood tests were available (N=121), the Framingham cardiovascular risk index, which represents the risk of developing cardiovascular disease in 10 years, was significantly lower at 2 years in the intervention group than in the usual care group (7.6% compared with 10%, p=0.01), although the group-by-time interaction for the relative change over time was not significant.
Costs: Health System Perspective
The mean annual costs of implementing the intervention, including staff salaries, fringe benefits, supplies and equipment, and overhead, were estimated at $973 per patient for the first year and $915 per patient for the second year, which did not include one-time equipment and training costs.
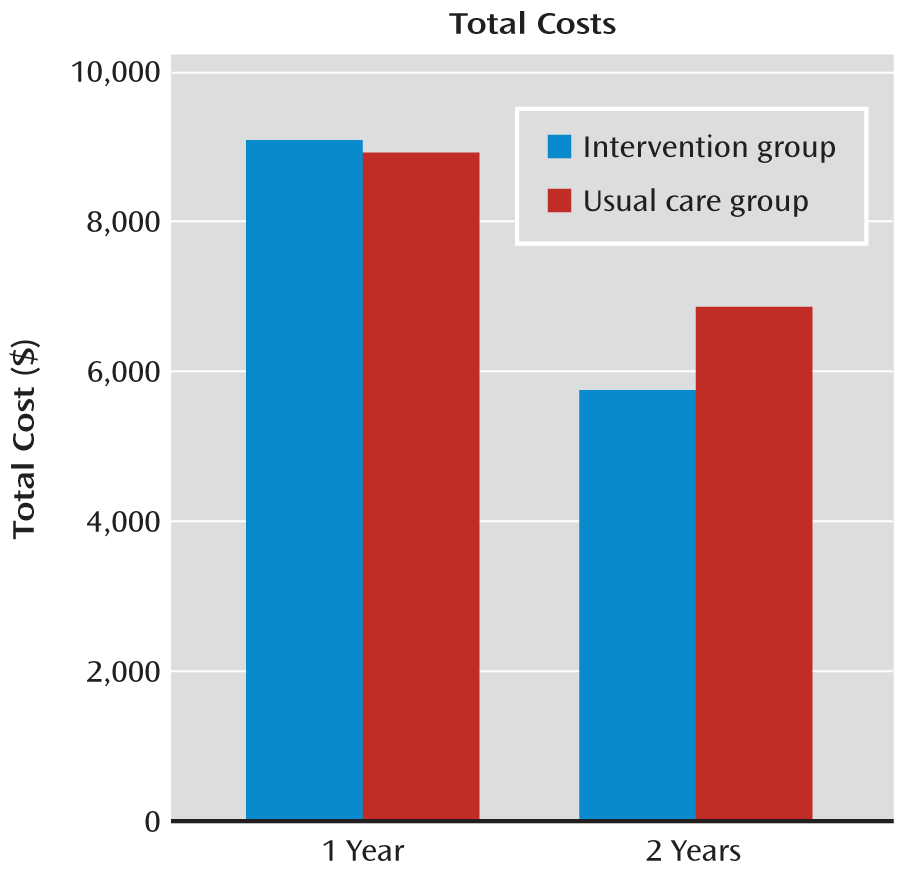
Table 3 lists the costs for various types of care and total costs of care for the two groups, as well as the difference between groups, at 1 and 2 years.
Figure 1 illustrates total costs for the two groups at 1 and 2 years.
In the health system perspective analysis at 1 year, with all study participants included, the mean total costs per patient were $218 higher for the intervention group than for the usual care group (95% CI=–1,190 to 1,585), which reflected a 38.4% probability of a cost offset. With extreme outliers (3% of participants) excluded, the mean total costs at 1 year were $93 higher for patients in the intervention group than for those in the usual care group (95% CI=–871 to 1,012), which reflected a 44.2% probability of a cost offset.
For the second year, the mean costs for patients in the intervention group were $932 less than for those in the usual care group, reflecting a 92.3% probability of a cost offset (95% CI=–1,973 to 102). With extreme outliers (3% of participants) excluded, the mean costs for patients in the intervention group were $920 less than for those in the usual care group, reflecting a 96.1% probability of a cost offset (95% CI=–1,718 to 54).
Costs: Managerial Perspective
Revenues were calculated based on the typical patient flow patterns seen for the nurses in the study (one new patient and five follow-up visits each day). Once caseloads were full, maximum revenue that could be achieved for the program using two nurse care managers working at full capacity, with all clients covered by Medicaid or other insurance, would be $360,840. Assuming minimal or no out-of-pocket payments by uninsured clients (which was the case for this clinic and is typical of CMHCs generally) (
30), the program would break even financially—i.e., revenues would equal or exceed expenditures—if at least 58% of clients had Medicaid coverage or some other health insurance coverage. Because only 40.5% of clients in the study clinic had Medicaid coverage, the program was not financially sustainable under existing conditions. Largely because of challenges in financing, the program closed after the grant was completed.
Discussion
From a clinical perspective, improvements observed at 1 year (
8) in the quality of primary care in the PCARE study persisted at 2 years. From a health system perspective, the cost profile was highly favorable and led to a trend toward a cost offset by the second year, suggesting a good value. However, from a managerial perspective, the program was not financially sustainable under current reimbursement conditions; with a greater proportion of insured clients, it could have been supported. These results, in particular the differences between societal and managerial cost perspectives, shed light on barriers to implementing these and other evidence-based practices in routine settings and on how expansion of insurance under health reform might help resolve such obstacles.
The intervention led to sustained improvement in the quality and outcomes of primary care. The majority of gains in quality and outcomes were seen during the first year, with continuing but smaller improvements during the second year. This asymptotic pattern is similar to that described in other quality improvement interventions, which typically have the greatest relative impact in the first 6–12 months as the greatest deficiencies in care are addressed, with subsequent efforts focused on maintaining those improvements (
31,
32).
For physical health outcomes, even a 2-year horizon may be a relatively brief window to reverse the cumulative effects of the socioeconomic deprivation, adverse health behaviors, and poor quality of medical care that lead to compromised health in this population (
33). Particularly for patients with high levels of medical morbidity, more aggressive programs that include medication management hold potential for substantial improvements in medical outcomes (
34). Nonetheless, in this study we observed significant improvements in a majority of 36-item Short-Form Health Survey subscales related to physical health (general health, physical functioning, and pain), and the intervention group had a significantly better cardiovascular risk profile at 2-year follow-up. Stepped-care models may be able to combine these two approaches, using care management for general mental health clinic populations, with more intensive treatment protocols for patients with preexisting cardiovascular risk factors or other illnesses.
From the health system perspective, there was a strong trend toward cost savings by the second year, with a 92.3% chance of a cost offset. This result is consistent with research on treating depression in primary care, which has found that these savings may become evident over the long term, particularly for the costliest and most complex patients (
35,
36). Given the relatively modest costs of establishing care management programs, and the ability of such programs to steer patients from inappropriate to more appropriate forms of care, these approaches may represent a particularly good value for society.
However, from a managerial perspective, assessing the business case for the intervention was more complex. Because of the high rate of uninsured clients (59%), revenues would not have covered the costs of running the program in the absence of grant funding. And despite data supporting the intervention's effectiveness and high levels of satisfaction by providers and patients, clinic management was unable to continue the program after the grant was completed. Challenges in achieving financial sustainability are not unique to medical care management programs; they apply to any new clinical programs in public-sector mental health systems with large numbers of uninsured clients. More generally, the mismatch between societal and managerial perspectives, coupled with a lack of a clear locus of accountability for improving quality, may underlie the failure of many cost-effective interventions to be effectively disseminated in routine clinical settings (
26,
37).
Several limitations of this study should be noted. The intervention was tested at a single site; care management approaches might need to differ in other types of settings (e.g., in rural areas without nearby medical providers). Similarly, the business case for these programs could differ in sites with lower numbers of eligible patients or in states with different mechanisms for paying for Medicaid patients or for the uninsured. Nonetheless, the characteristics of the site and payment approaches in the study clinic are typical of urban community health centers nationwide (
38). Also, 2-year follow-up interview rates were relatively low; however, because cost data, which were the primary outcomes examined in this study, were derived from patient charts, follow-up interviews were less of a concern for these analyses.
Expansion of Medicaid under the Patient Protection and Affordable Care Act is likely to disproportionately improve rates of insurance for persons with mental illness who are currently uninsured (
39). This could help improve the business case for implementing evidence-based programs like the one described here in community settings. Other new financing strategies to be tested under new models of care, such as bundled payments that include coverage for care managers, could also help reduce the barriers to implementation of these and other evidence-based quality improvement strategies for persons treated in safety net settings (
40). Finally, for persons with serious and persistent mental illnesses, new health home models will include the development of specialty care medical homes that provide primary care services through community mental health providers (
5). These new initiatives hold the potential to begin to better align financial incentives for improving physical health care in this vulnerable population and, more broadly, for disseminating evidence-based practices in community mental health settings.