Childhood Maltreatment Predicts Unfavorable Course of Illness and Treatment Outcome in Depression: A Meta-Analysis
Abstract
Objectives:
Method:
Results:
Conclusions:
Method
Inclusion Criteria
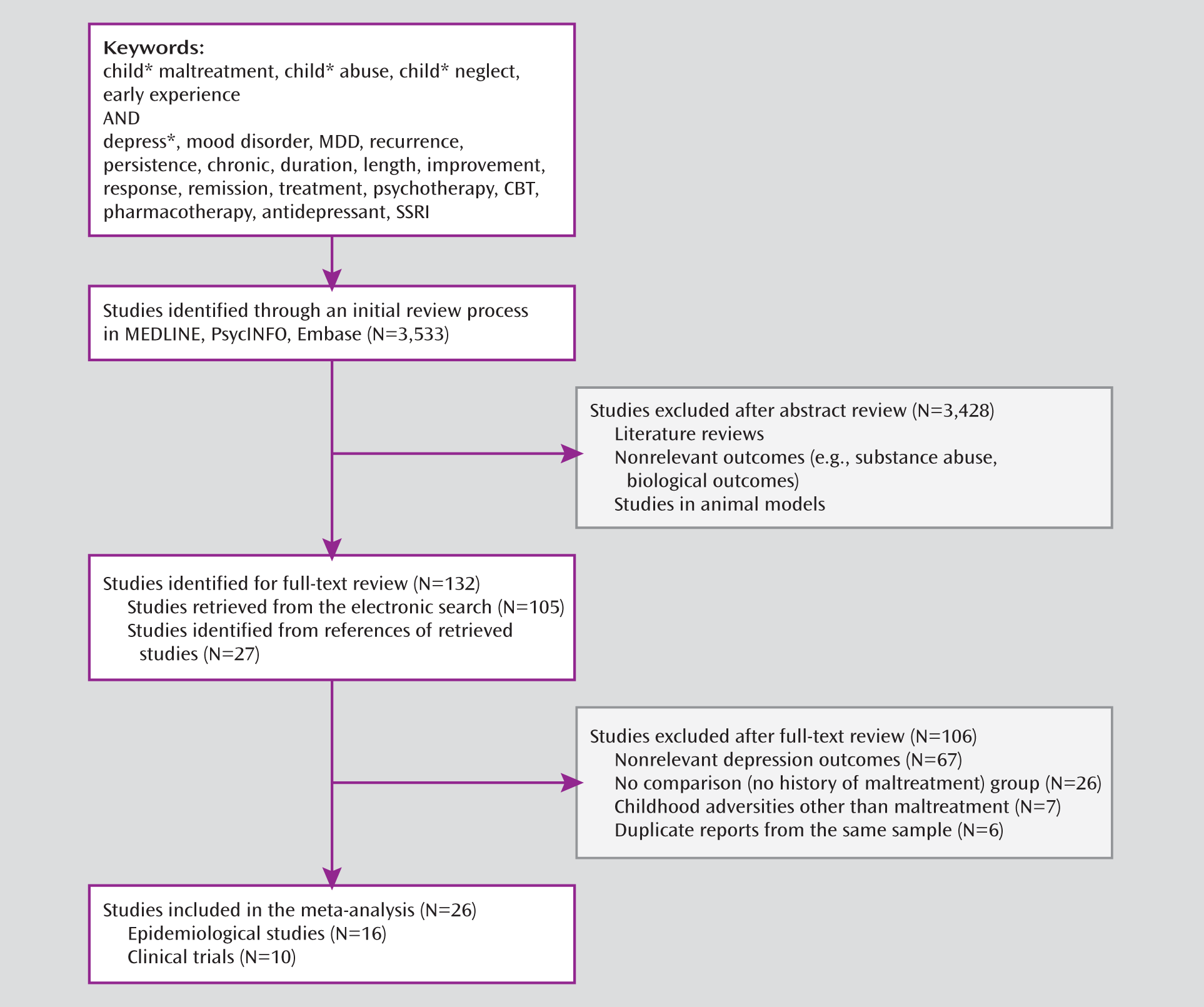
Identification of Studies
Data Extraction
Statistical Analysis
Results
Epidemiological Studies
| Authors (Reference) | Study N | Mean Age or Range (Years) | % Female | Sample Type | Depression Measure | Maltreatment Measure | Outcome Definition | Length of Observation (Years) | Results |
|---|---|---|---|---|---|---|---|---|---|
| Kessler and Magee (30) | 1,024 | 33 | 50 | Population | DIS, FHRDC | Own questionnaire | Recurrence: new depressive episode(s) in individuals with history of depression | 16 | Family violence associated with greater recurrence (odds ratio=2.04, 95% CI=1.42–2.93) |
| Brown and Moran (31) | 404 | 18–50 | 100 | Population | PSE | CECA | Persistence: depressive episode lasting 12 months or more | 3 | Childhood adversity associated with greater persistence (odds ratio=4.02, 95% CI=1.59–10.15) |
| Brown et al. (32) | 125 | 18–60 | 100 | Clinical | PSE | CECA | Persistence: nonrecovery from depression over 12 months | 2 | Childhood adversity associated with greater persistence (odds ratio=1.93, 95% CI=1.05–3.54) |
| Zlotnick et al. (33) | 37 | 100 | Clinical | Semi-structured interview | Own questionnaire | Persistence: non-recovery (HAM-D <7 for 3 consecutive months after hospital discharge) | 1 | Childhood adversity not associated with persistence (odds ratio=2.29, 95% CI=0.49–10.61) | |
| Kessler et al. (34) | 5,877 | 15–54 | 50 | Population | CIDI | Own questionnaire | Persistence: risk of dysthymia | 40 | Childhood adversity associated with greater persistence (odds ratio=2.81, p<0.05) |
| Bernet and Stein (35) | 88 | 42 | 50 | Clinical | SCID | CTQ | Recurrence: number of depressive episodes | 25 | Childhood trauma associated with greater recurrence (t=4.78, p<0.0005) |
| Hayden and Klein (36) | 86 | 31.1 | 75.6 | Clinical | SCID, longitudinal interval follow-up evaluation | EHEI | Persistence: nonrecovery from dysthymic disorder (<8 consecutive weeks with minimal or no symptoms) | 5 | Physical abuse associated with greater persistence (smaller recovery: hazard ratio=0.83, 95% CI=0.60–1.15) |
| Wainwright and Surtees (37) | 3,353 | 62.3 | 55.2 | Population | Structured self-assessment | Own questionnaire | Recurrence: number of depressive episodes | 46 | Physical abuse not associated with greater recurrence (relative risk=1.27; 95% CI=0.77–1.99) |
| Brown et al. (38) | 198 | 34 | 100 | Population | SCAN | CECA | Persistence: depressive episode lasting ≥12 months | 17 | Childhood adversity associated with greater recurrence (odds ratio=14.9, 95% CI=6.0–37.0) |
| Collishaw et al. (39) | 3,624 | 44.2 | 50 | Population | SADS-L | CECA | Recurrence: ≥3 lifetime depressive episodes | 28 | Childhood adversity associated with greater recurrence (odds ratio=7.80, 95% CI=1.7–35.5) |
| Danese et al. (7) | 1,037 | 32 | 48 | Population | DIS | Prospective observation + retrospective reports | Recurrence: ≥2 lifetime depressive episodes | 21 | Childhood adversity associated with greater recurrence (odds ratio=2.60, 95% CI=1.60–4.24) |
| Ritchie et al. (40) | 942 | 72 | 58 | Population | MINI diagnosis or CES-D >16 or current antidepressant treatment | Own questionnaire | Recurrence: ≥2 depressive episodes | 4 | Childhood adversity associated with greater recurrence (odds ratio=2.89, 95% CI=1.83–4.57) |
| Wiersma et al. (41) | 1,230 | 40.7 | 67.3 | Clinical | CIDI | CTI | Persistence: depressive episode lasting ≥24 months | 4 | Physical abuse associated with greater persistence (odds ratio=1.99, 95% CI=1.37–2.88) |
| Angst et al. (42) | 110 | 27–41 | 60 | Clinical | SPIKE | Own questionnaire | Persistence: depressive symptoms for most days over 2 years or daily for 12 months | 13 | Childhood adversity associated with greater persistence (p=0.05) |
| McLaughlin et al. (43) | 5,692 | 36.7 | 42 | Population | CIDI | Own questionnaire | Persistence: time since more recent episode, controlling for age at onset and time since onset | 20 | Physical abuse associated with greater persistence (odds ratio=1.9, 95% CI=1.5–2.4) |
| Suija et al. (44) | 123 | 39 | 85 | Clinical | CIDI | CTI | Recurrence: new depressive episode in individuals with history of depression | 1 | Childhood trauma associated with greater recurrence (odds ratio=1.58, 95% CI=1.05–2.38) |
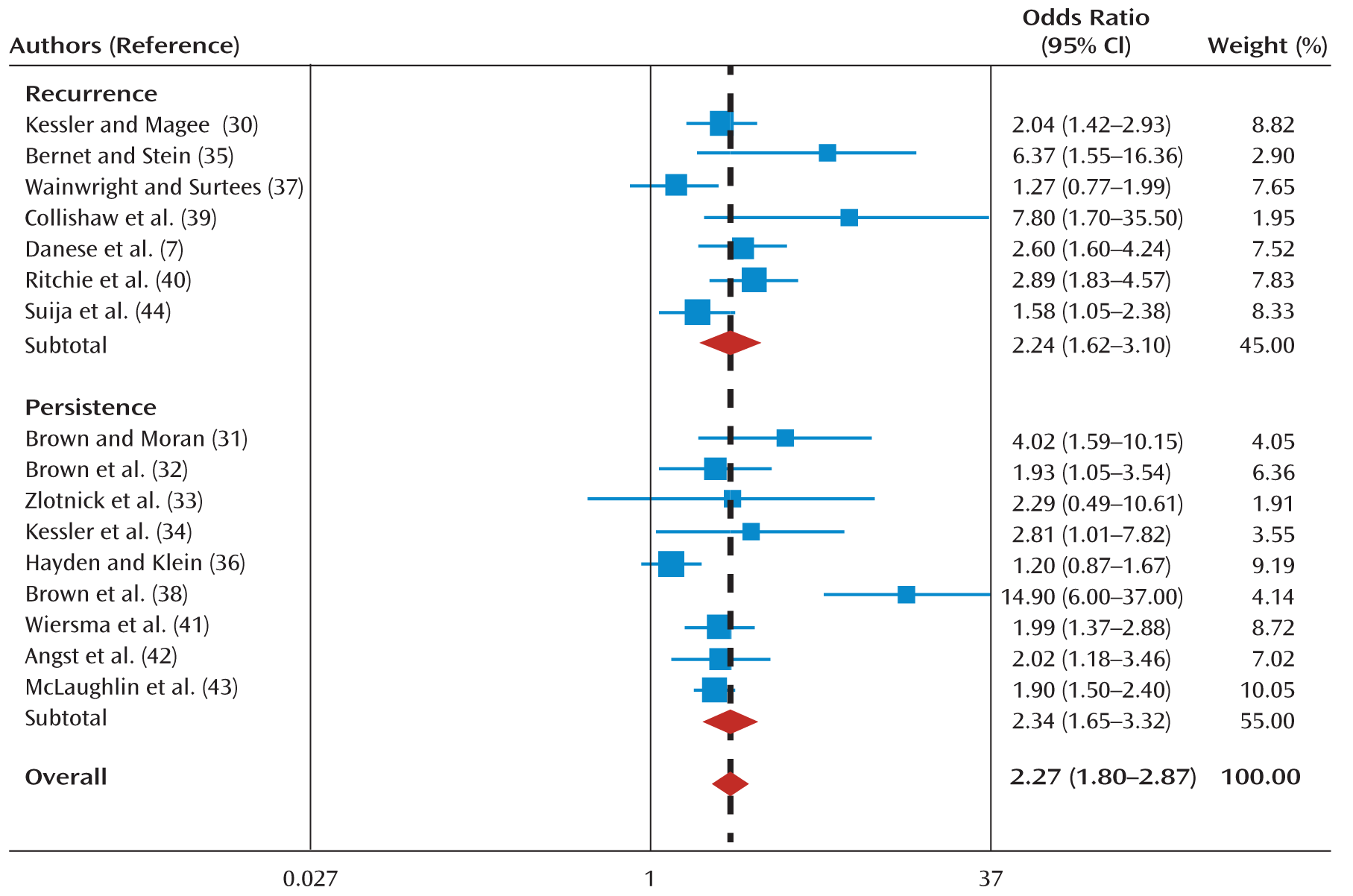
Publication bias.
Sensitivity analyses.
Bias owing to study quality.
Effect of age at illness onset.
Recall bias.
Clinical Trials
| Authors (Reference) | Study N | Mean Age (Years) | % Female | Depression Measure | Maltreatment Measure | Treatment Description | Length of Treatment (Weeks) | Outcome Definition | Results |
|---|---|---|---|---|---|---|---|---|---|
| Sakado et al. (45) | 60 | 43 | 50 | SCID | PBI | Tricyclic antidepressant | 16 | Remission: HAM-D-17 <8 | Low paternal care associated with lack of remission (odds ratio=1.9, 95% CI=1.7–2.2) |
| Nemeroff et al. (46) | 681 | 43 | 65.3 | SCID | CTS | CBASP, nefazodone, combination | 12 | Improvement: HAM-D-24 score reduction | Childhood abuse associated with poor outcome within the pharmacological treatment arm and good outcome within the psychotherapy treatment arm (trauma-by-treatment interaction F=3.13, df=1, 495, p=0.045) |
| Barbe et al. (47) | 107 | 15.8 | 75.7 | K-SADS; BDI ≥ 13 | CBQ | CBT, SBFT, NST | 12–16 | Remission: free from major depressive disorder diagnosis for ≥2 months | Family conflict associated with lack of remission (relative risk=0.95, 95% CI=0.91–0.998) |
| Enns and Cox (48) | 171 | 41.8 | 64.3 | Unstructured interview | DMQ, PBI | Various antidepressants and psychological treatments | 52 | Response: 50% decrease in BDI scoreRemission: BDI <10 | Sexual abuse associated with lack of response (χ2=4.32, p=0.038) and lack of remission (χ2=4.38, p=0.036); low parental care or overprotection were unrelated to outcome (p=0.58) |
| Asarnow et al. (49) | 287 | 15.9 | 69.8 | CDRS-R ≥40; CGI ≥4; resistance to SSRIs | CBQ, clinical interview | Medication switch alone (SSRI or venlafaxine), medication switch plus CBT | 12 | Response: CDRS-R score reduction ≥50% | Childhood abuse associated with lack of response to CBT but not to pharmacotherapy or combination (abuse-by-treatment interaction β=0.15, p<0.001) |
| Johnstone et al. (50) | 195 | 32 | 57 | Not specified | PBI, own questionnaire | Fluoxetine, nortriptyline | 6 | Improvement: MADRS score percentage reduction | Maternal overprotection was associated with less improvement (odds ratio=0.93, 95% CI=0.89–0.97). Parental care and childhood abuse were unrelated to outcome |
| Klein et al. (51) | 808 | 43.6 | 55 | SCID, HAM-D-17 ≥20 | MOPS, CTQ | Texas Medication Algorithm | 12 | Remission: HAM-D-17 <8 | Childhood abuse associated with lack of remission (odds ratio=0.52, p<0.01) |
| Shirk et al. (52) | 50 | 15.9 | 68 | C-DISC-IV | LEQ | CBT | 12 | Remission: free from major depressive disorder diagnosis at the end of treatment Improvement: BDI score reduction | Childhood trauma associated with lack of remission (ρ=–0.31 to –0.35, p<0.05) |
| Lewis et al. (53) | 427 | 14.6 | 54 | K-SADS-PL, CDRS-R >45 | PTSD section of K-SADS-PL | Fluoxetine, CBT, combination, placebo | 12 | Improvement: reduction in CDRS-R score | Childhood trauma associated with poor response to CBT but not with response to fluoxetine or combination treatment (trauma-by-treatment-by-time interaction F=2.02, p<0.05) |
| Miniati et al. (54) | 312 | 39 | 73 | SCID | Clinical interview | Medication (citalopram or escitalopram), IPT, combination | 12 | Time to remission (Remission: HAM-D-17 <8) | Childhood abuse associated with longer time to remission across treatments (hazard ratio=1.68, 95% CI=1.09–2.59) |
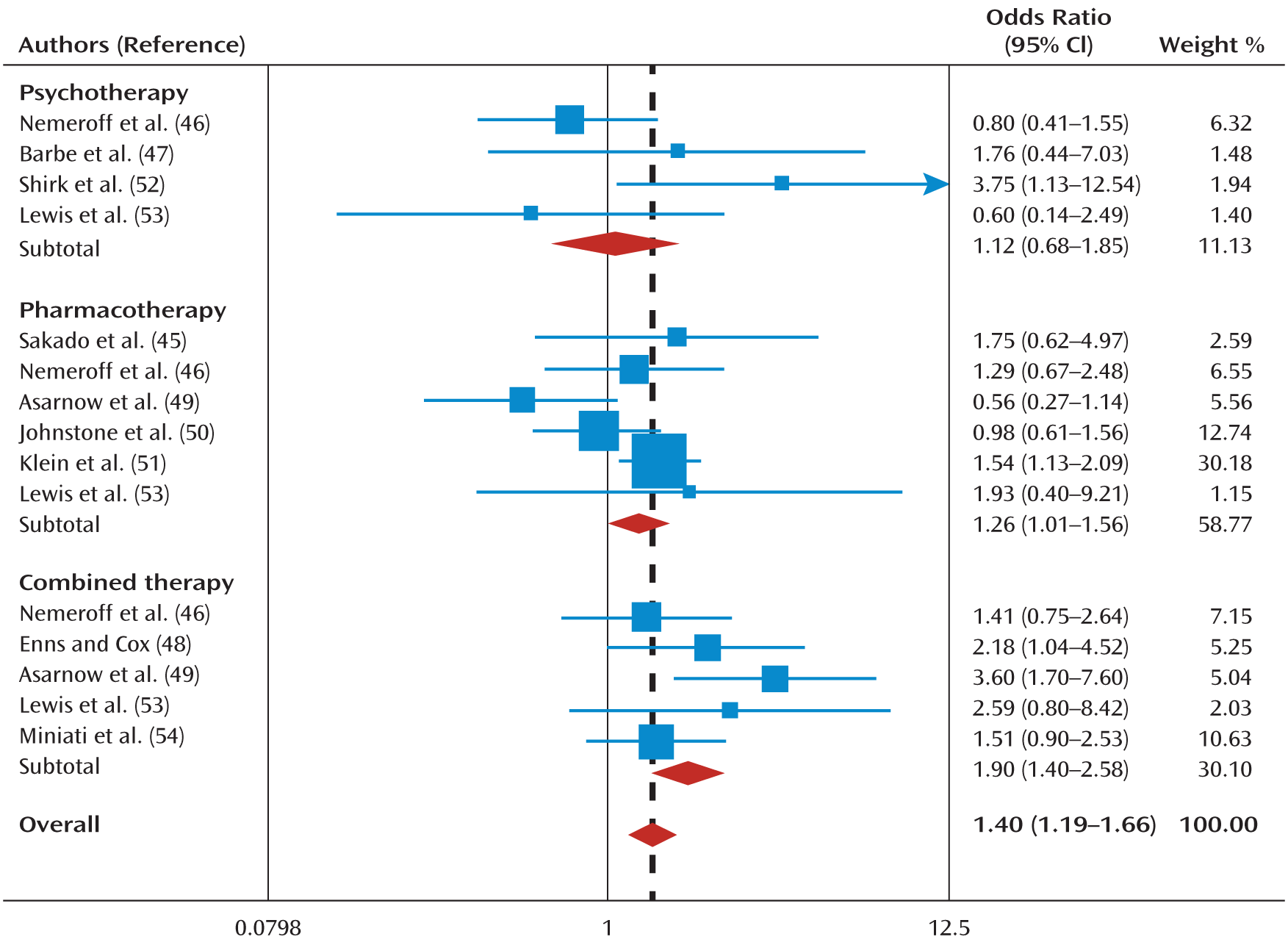
Publication bias.
Sensitivity analyses.
Bias owing to study quality.
Age effect.
Discussion
Limitations
Implications
Future research.
Clinical care.
Public health.
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 296.70 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

