Since that time, however, only one study has systematically assessed the disturbed but nonpsychotic cognitions of patients with borderline personality disorder and axis II comparison subjects (
34). In a cross-sectional study, patients in the borderline group reported experiencing ideas of reference (e.g., “I’m a bad person,” “I’m damaged beyond repair”), experiences of depersonalization or derealization (e.g., people and things seem unreal), and undue suspiciousness (e.g., “Other people hate me,” “I’m being abused”) a substantial percentage of the time (on average, for these examples, 18%–46% of the time). These cognitions not only were reported a significantly higher percentage of the time by borderline patients than axis II comparison subjects but also were quite specific to those with the borderline diagnosis.
The present study is, to our knowledge, the first prospective study to assess the cognitive features of a rigorously diagnosed group of patients with borderline personality disorder over time. The study also assessed the cognitive features of a group of axis II comparison subjects over the follow-up period. Three types of disturbed but nonpsychotic thought were examined—odd thinking, unusual perceptual experiences, and nondelusional paranoia—as well as quasi-psychotic and true psychotic thought.
Method
This study is part of the McLean Study of Adult Development, a multifaceted longitudinal study of the course of borderline personality disorder. The methodology of this study, which was reviewed and approved by the McLean Hospital Institutional Review Board, has been described in detail elsewhere (
35). Briefly, all participants were initially inpatients at McLean Hospital in Belmont, Mass. Each patient was screened to determine that he or she was between the ages of 18 and 35 years; had a known or estimated IQ of 71 or higher; had no history or current symptoms of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause serious psychiatric symptoms; and spoke English fluently.
All participants provided written informed consent after receiving an explanation of the study procedures. Each patient then met with a master’s-level interviewer blind to the patient’s clinical diagnoses for a thorough diagnostic assessment. Three semistructured interviews were administered: the Structured Clinical Interview for DSM-III-R Axis I Disorders (
36), the Revised Diagnostic Interview for Borderlines (
37), and the Diagnostic Interview for DSM-III-R Personality Disorders (
38). The interrater and test-retest reliability of all three of these measures have been found to be good to excellent (
39,
40).
At each of eight follow-up assessments separated by 24 months, axis I and II psychopathology were reassessed by interview methods similar to those used at baseline by staff members blind to baseline diagnoses. After informed consent was obtained, our interview battery was readministered. The follow-up interrater reliability (within one generation of follow-up raters) and follow-up longitudinal reliability (from one generation of raters to the next) of these three measures have been found to be good to excellent (
39,
40).
The cognitive experiences of borderline patients and axis II comparison subjects were assessed using the cognitive section of the Revised Diagnostic Interview for Borderlines. Six items (each involving multiple questions) assess the presence of odd thinking, three assess the presence of unusual perceptual experiences, three assess the presence of nondelusional paranoia, 12 assess the presence of quasi-psychotic delusions, and three assess the presence of quasi-psychotic hallucinations. The same 15 sets of questions are used to assess the presence of true delusions and hallucinations as were used to assess the presence of their quasi-psychotic counterparts.
As for differentiating between quasi and true psychotic experiences, quasi-psychotic experiences were defined as delusions or hallucinations that were circumscribed (i.e., pertaining to limited aspects of thought or perception), short-lived (i.e., lasting only hours to days), and nonbizarre (e.g., belief that childhood adversity was deserved). In contrast, true psychotic experiences were defined as delusions or hallucinations that were widespread (i.e., pertaining to broad aspects of thought or perception), long-standing (i.e., lasting weeks to months or longer), and disconnected from shared reality (e.g., a dead parent was now alive).
Statistical Analysis
Generalized estimating equations, with diagnosis and time as main effects, were used in longitudinal analyses of prevalence data. Tests of diagnosis-by-time interactions were conducted. These analyses modeled the log prevalence, yielding an adjusted relative risk ratio and 95% confidence interval (CI) for diagnosis and time (and their interaction, as appropriate). Gender was also included in these analyses as a covariate, as borderline patients were significantly more likely than axis II comparison subjects to be women. Alpha was set at 0.05 (two-tailed).
Given the large number of comparisons, we applied the Bonferroni correction for multiple comparisons to each of the five types of cognition studied. This resulted in the following adjusted alpha levels: odd thinking (0.05/7=0.007), unusual perceptual experiences (0.05/4=0.013), nondelusional paranoia (0.05/4=0.013), and both quasi and true psychotic experiences (0.05/3=0.017).
Results
A total of 290 patients met criteria for borderline personality disorder according to both the Revised Diagnostic Interview for Borderlines and DSM-III-R, and 72 met DSM-III-R criteria for at least one non-borderline axis II disorder but neither criteria set for borderline personality disorder. Of these 72 comparison subjects, 4% met DSM-III-R criteria for an odd cluster personality disorder, 33% met criteria for an anxious cluster personality disorder, 18% met criteria for a non-borderline dramatic cluster personality disorder, and 53% met criteria for personality disorder not otherwise specified (which was operationally defined in the Diagnostic Interview for DSM-III-R Personality Disorders as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R).
Baseline demographic data have been reported before (
35). Briefly, 77.1% (N=279) of the participants were women and 87% (N=315) were white. Participants’ mean age was 27 years (SD=6.3), their mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest) (
41), and their mean score on the Global Assessment of Functioning Scale was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
Attrition over the course of the study was low; 87.5% (N=231/264) of surviving borderline patients (13 died by suicide and 13 died of other causes) were reinterviewed at all eight follow-up waves. The axis II comparison subjects had a similar participation rate, with 82.9% (N=58/70) of surviving patients in this study group (one died by suicide and one died of other causes) being reassessed at all eight follow-up waves.
Given space limitations, only data from baseline, the 4-year follow-up, the 8-year follow-up, the 12-year follow-up, and the 16-year follow-up are presented in
Tables 1–
5. However, data from baseline and all eight follow-up waves were used in our analyses and are presented in the
data supplement that accompanies the online edition of this article.
Table 1 details the nonpsychotic odd thinking reported by borderline patients and axis II comparisons subjects over 16 years of prospective follow-up. As can be seen,
a significantly higher percentage of borderline patients than axis II comparison subjects reported magical thinking, overvalued ideas (of being, for example, ugly, stupid, fat, bad), and any type of odd thinking. However, both study groups reported similar low rates of marked superstitiousness, sixth sense, telepathy, and clairvoyance. Rates of all types of odd thinking and the overall category of odd thinking declined significantly over time for patients in both study groups. No diagnostic group-by-time interactions in this or other types of thought were found to be significant, indicating similar rates of decline in both groups.
As the relative risk ratios for diagnosis and time in this and subsequent tables contain more fine-grained information, an illustrative example might be useful. As can be seen in
Table 1, about 75% of borderline patients (and about 43% of axis II comparison subjects) reported having overvalued ideas at baseline. By the time of their 16-year follow-up, these prevalence rates had declined to about 21% and 7%, respectively. The relative risk ratio of 2.10 for study group indicates that borderline patients were approximately twice as likely to report this type of odd thinking as axis II comparison subjects. The relative risk ratio of 0.16 for time indicates that the prevalence of overvalued ideas decreased by 84% ([1–0.16]×100%) for both groups over the course of 16 years of prospective follow-up.
Table 2 details the unusual perceptual experiences reported by borderline patients and axis II comparisons subjects over the follow-up period. A significantly higher percentage of borderline patients than axis II comparison subjects reported recurrent illusions, depersonalization, derealization, and any type of unusual perceptual experience. All three types of unusual perceptual experience studied and the overall category of unusual perceptual experiences declined significantly over time for participants in both groups.
Table 3 details the nondelusional paranoid experiences reported by borderline patients and axis II comparison subjects over the follow-up period. A significantly higher percentage of borderline patients than axis II comparison subjects reported undue suspiciousness, ideas of reference, other paranoid ideation (e.g., “Often thought that people were giving you a hard time or were out to get you?”), or any type of nondelusional paranoia. In addition, all four of these symptoms or symptom clusters declined significantly over time for participants in both groups.
Table 4 details the quasi-psychotic experiences reported by borderline patients and axis II comparisons subjects over the follow-up period. A significantly higher percentage of borderline patients than axis II comparison subjects reported quasi-psychotic delusions, hallucinations, and any type of quasi-psychotic thought. For those in both groups, all three symptom clusters declined significantly over time.
Table 5 details the true psychotic experiences reported by borderline patients and axis II comparisons subjects over the follow-up period. Because of the sparseness of data in
Table 5, especially for the axis II comparison group, the comparisons of prevalence rates in
Table 5 must be interpreted cautiously. With this caveat, it appears that a significantly higher percentage of borderline patients than axis II comparison subjects reported true psychotic hallucinations (but not delusions) and any type of true psychotic thought. However, none of these types of thought appeared to decline significantly for patients in either group, as their low rates were relatively stable over time.
Because so many specific forms of thought were found to decline significantly over time for borderline patients, it is of interest to compare the longitudinal course of the cognitive symptoms of borderline personality disorder with symptoms of the disorder in the other three sectors of borderline psychopathology.
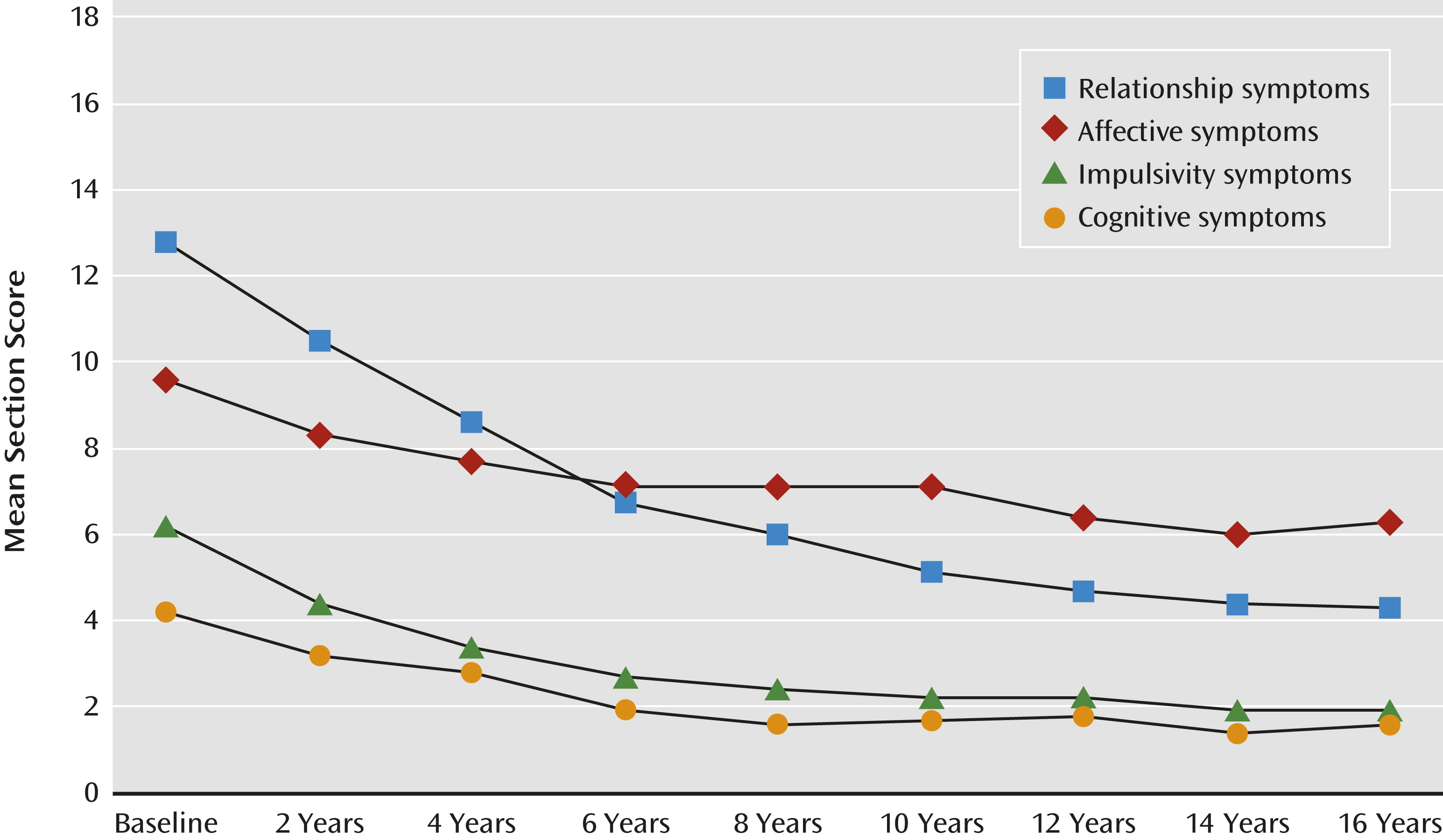
Figure 1 details the mean section scores of the Revised Diagnostic Interview for Borderlines of borderline patients over 16 years of prospective follow-up. The score ranges for these four sections of borderline psychopathology were as follows: affective, 0–10; cognitive, 0–6; impulsivity, 0–10; and troubled relationships, 0–18. Because the ranges of scores varied, we examined relative declines, in terms of percent change. Using longitudinal regression analyses with log-transformed outcome scores, we found that all four of these dimensional scores declined significantly for borderline patients: affective section scores declined by 42% (p<0.001), cognitive section scores by 55% (p<0.001), impulse action patterns section scores by 63% (p<0.001), and troubled relationships by 71% (p<0.001).
In addition, we fitted a joint longitudinal regression model that allowed for estimation of the correlations among each individual’s slopes for the four section scores. These results indicated that changes in cognitive section scores over time were highly correlated with corresponding changes in the other three section scores, with correlations of 0.76, 0.84, and 0.89 with changes in affective, impulse action patterns, and troubled relationships section scores, respectively. That is, individuals with the steepest declines in cognitive section scores also tended to have the steepest declines in the other three section scores.
Discussion
Four main findings emerge from the results of this study. The first is that all of the types of disturbed but nonpsychotic thought studied were common: 86% of borderline patients reported some type of odd thinking at study entry, 76% reported some type of unusual perceptual experience, and 87% reported some type of nondelusional paranoia. Over time, each of these three types of disturbed but nonpsychotic thinking was found to be significantly more common among borderline patients than axis II comparison subjects. Each was also found to decline significantly over time. However, even 16 years after the index admission, relatively high rates of these three types of thought were found among borderline patients: 37% reported odd thinking, 26% reported unusual perceptual experiences, and 43% reported nondelusional paranoia.
The second main finding is that quasi-psychotic thought was common among borderline patients at study entry (57%) but declined significantly over the 16 years of prospective follow-up (to 7%). It was also reported by a significantly higher percentage of borderline patients than axis II comparison subjects (19% at baseline and 0% at 16-year follow-up). The exact reasons for this decreasing rate are unclear. Clinical experience suggests that additional support and structure can be useful in the resolution of such symptoms. However, it cannot be overlooked that a relatively high percentage of borderline patients were taking antipsychotic medication during each wave of follow-up (
42). Given the naturalistic design of this study, it is not clear whether these medications were prescribed for their antipsychotic properties or for their anxiolytic properties. Nor is there strong empirical evidence that these agents are helpful in treating the relatively fleeting departures from reality that we have described as quasi-psychotic thought.
The third main finding is that true psychotic experiences of the type reported by persons with psychotic disorders were rare in our sample of borderline patients. At no time did the percentage of these patients reporting any true psychotic thought (delusions or hallucinations) exceed 7%.
The baseline figures we observed for the three types of disturbed but nonpsychotic thinking assessed in this study are similar to those seen in earlier cross-sectional studies of the cognition of borderline patients conducted over 20 years ago (
22,
33). At baseline, we also found high rates of quasi-psychotic (
22,
33) and low rates of true psychotic thought (
23,
33) that were similar to those reported in earlier cross-sectional studies.
The fourth main finding is that the cognitive symptoms of borderline personality disorder declined more sharply over time than affective symptoms but less sharply than impulsive and interpersonal symptoms. This finding is consistent with results our group reported (
43) on the 10-year course of 24 symptoms of borderline personality disorder that included symptoms from all four sectors of borderline psychopathology. It also makes clinical sense, as cognitions are often more resistant to change than forms of impulsivity and interpersonal patterns.
On a per-person rather than a group level, we found that borderline patients who had the sharpest declines in the severity of cognitive symptoms also had the sharpest declines in the severity of the other three areas of borderline psychopathology: affects, impulsive behaviors, and maladaptive relationship patterns. This is not surprising, as the cognitive symptoms almost certainly affect and are affected by symptoms in the other three sectors of borderline psychopathology. In the earlier study mentioned above (
43), the cognitive symptoms most frequently observed in the present study were found to remit relatively slowly and were termed temperamental symptoms. These symptoms were odd thinking (mostly ideas of reference), unusual perceptual experiences (most commonly experiences of depersonalization and derealization), and nondelusional paranoia (which includes distrust of others and the belief that others have malevolent intentions). In the earlier study, quasi-psychotic thought was found to remit relatively rapidly and was termed an acute symptom.
It is clear that acute and temperamental cognitive symptoms can affect and be affected by acute and temperamental symptoms in other areas of borderline psychopathology. For example, experiences of depersonalization (i.e., feeling numb or dead), a temperamental cognitive symptom, have been found to be associated with episodes of self-harm (
44), an acute symptom in the realm of impulsivity. Similarly, profound abandonment concerns, a temperamental symptom of an interpersonal nature, is often one of the reasons for an acute cognitive symptom—quasi-psychotic delusions centering on the untrue belief that abandonment by a romantic partner or a mental health professional is imminent (
5).
Yet, it seems most likely, given their persistence, that temperamental symptoms in the other realms of borderline psychopathology most commonly interact over time with the temperamental cognitive symptoms associated with the disorder and vice versa, perhaps partially explaining why they are relatively slow to remit. For example, ideas of reference centering on the belief that one is bad or evil may exacerbate the affective symptoms of BPD, most of which are viewed as temperamental in nature. Such a belief may intensify feelings of depression, helplessness/hopelessness, and loneliness/emptiness. Similarly, general impulsivity (e.g., verbal outbursts, verbal threats, and physical assaults), a temperamental symptom in the behavioral realm, may intensify mistrust and suspiciousness of others who it is feared might retaliate by distancing themselves.
Taken together, the four main findings of the study have both nosological and treatment implications. In terms of nosology, neither DSM-III nor DSM-III-R criteria for borderline personality disorder included a cognitive criterion. Such a symptom cluster was added in 1994 in DSM-IV. It stated that borderline patients were prone to transient, stress-related paranoid ideation or severe dissociation. The proposed DSM-5 criteria for this disorder did not highlight cognitive distress or distortions at the trait level (
45). Rather, the proposed criteria set focused on negative affectivity, disinhibition, and antagonism.
Thus, our system of nosology did not appear to be planning to include symptoms that have been observed in numerous cross-sectional studies (
6–
33) and now in a long-term longitudinal study to be both common and relatively specific to borderline personality disorder. The reasons for this omission are unclear given how common and disabling these cognitive symptoms are in carefully diagnosed borderline patients. It may be that many of these symptoms are thought to be related more to schizotypal than borderline personality disorder, as in the DSM-III era high rates of borderline patients met criteria for co-occurring schizotypal personality disorder (
46). However, as a result of changes in the criteria required for a schizotypal diagnosis in DSM-III-R and DSM-IV, these symptoms in patients with schizotypal personality disorder are now concurrent with social isolation and/or behavioral and speech oddities not common among borderline patients. In fact, only 2.4% (N=7) of the borderline patients in the present study met criteria for this odd cluster disorder at study entry (
47).
In terms of treatment implications, all six of the major evidence-based treatments for borderline personality disorder focus on three main outcomes: episodes of self-mutilation, suicide efforts, and psychiatric hospitalizations (
48–
53). While four of the treatments pay attention to cognitive elements of the disorder (mindfulness [
54], mentalization [
49], schemas [
50], and transference distortions [
51]), none actually has treatment of the cognitive symptoms of borderline personality disorder as a major aim.
These findings also have psychosocial implications. Clearly, believing that one is evil, being mistrustful of others, and feeling numb can interfere with the establishment and maintenance of stable reciprocal relationships. These types of disturbed thought can also interfere with getting and keeping a job. Plainly, having consistently low self-esteem and frequent experiences of depersonalization coupled with chronic suspiciousness of others can make it difficult, if not impossible, to work consistently and competently. Or, looked at another way, the disturbed thought of borderline patients may be one of the factors behind the relatively low rates of recovery from borderline personality disorder that we have reported (i.e., symptomatic remission and concurrent good social and vocational functioning) (
55).
This study has several limitations. One is that all of the patients were seriously ill inpatients at the start of the study. Another is that about 90% of the patients in both groups were in individual therapy and taking psychotropic medications at baseline, and about 70% were participating in each of these outpatient modalities during each follow-up period (
42). Thus, it is difficult to know if these results would generalize to a less disturbed group of patients or to people meeting criteria for borderline personality disorder who were not in treatment. A third limitation is that we only used the cognition section of the Revised Diagnostic Interview for Borderlines to assess the cognitive experiences of study subjects. The use of an additional interview that was independent of our diagnostic battery to assess these symptoms would have added to the richness and the validity of our findings.
Taken together, the results of this study suggest that disturbed cognitions are common among borderline patients and are distinguishing for the disorder. Disturbed cognitions also decline substantially over time but remain a residual problem, particularly those of a nonpsychotic nature.