After more than 150 years of studies examining the association between mental disorders and excess mortality (
1,
2), it is well established that mortality rates are significantly elevated in depressed patients. A significant association between depression and excess mortality has been confirmed in several hundred studies in many different populations, including community samples (
3) and patients with heart disease (
4), cancer (
5), stroke (
6), and diabetes (
7).
Although no single comprehensive model has yet described the causal mechanisms linking depression to excess mortality, several key mechanisms have been proposed. Some of these are more or less disease specific. In cancer research, for example, it has been suggested that depression-related stress may have a negative effect on the cellular processes involved in the repair of damaged DNA (
8) and may accelerate tumor cell growth and promote tumor migration and invasive capacity (
9), which subsequently results in poorer cancer outcomes (
10). In heart disease research, it has been hypothesized that the excess mortality in depression is associated with factors such as vascular endothelial dysfunction (
11), a prolonged QT interval (
12), lower heart rate variability reflecting altered cardiac autonomic tone (
13), and increased platelet aggregation (
11). In addition, in patients with somatic diseases, depression could have an unfavorable impact on adherence to a prescribed treatment regimen (
14), in turn having a direct impact on survival.
On the other hand, several of the mechanisms that have been proposed to mediate the association between depression and mortality are not specific to one disease and may lead to different diseases and multiple pathways to death. For example, there is evidence suggesting that dysregulation of central biological stress systems, including hypothalamic-pituitary-adrenal axis hyperactivity (
15), neuroimmune dysregulations (
16), and sympathoadrenergic dysregulation, may have a causal role in the association between depression and overall mortality (
3). Furthermore, rates of negative lifestyle factors, such as physical inactivity, smoking, alcohol consumption, and unhealthy eating patterns (
14), are higher in depressed patients and may explain part of the association between depression and mortality, independent of whether an individual already has a somatic disease.
If excess mortality in depression is caused by disease-specific mechanisms, it can be expected that mortality risks associated with depression would be higher in depressed patients than in other patients or community samples. However, if the excess mortality is more related to generic factors that are not specific to one disease, we would expect a comparable association between depression and mortality in any patient or community sample.
To the best of our knowledge, no meta-analytic research has yet examined whether or not excess mortality in depression is higher in specific patient groups. Meta-analyses are an excellent method for examining this research question because they can integrate the results of multiple studies and thereby provide a better estimate of the true mortality risk of depression across different types of populations. We conducted a comprehensive meta-analysis of prospective studies examining the association between depression at baseline and mortality at follow-up. We included specific patient populations as well as the much healthier community-based samples and any other study in which the association between depression at baseline and mortality at follow-up was examined.
Method
Selection of Studies
Studies were identified by several methods. First, we conducted comprehensive literature searches (up to April 2013) in three bibliographical databases—PubMed, PsycINFO, and Embase—combining terms indicating depression (such as major depression, mood disorder, depression, depressive), mortality (death, survival), and prospective design (incidence, follow-up studies, longitudinal studies, prospective studies). Both text terms and keywords were used. The detailed search string for our PubMed search is provided in Appendix A in the
data supplement that accompanies the online edition of this article. We also examined the references of included studies, as well as the references of earlier meta-analyses examining the association between depression and mortality (see Appendix B in the
data supplement). We retrieved the full-text papers of studies that possibly met our inclusion criteria. Full-text papers were examined by two independent raters for possible inclusion. Disagreements were resolved by discussion.
We included studies with a prospective design in which depression was examined at baseline and all-cause mortality was reported at follow-up. Depression had to be assessed with a standardized depression measure (either a diagnostic interview or a self-report questionnaire). We included studies in any target group (community, patient, and any other sample) as well as case-control studies. Studies were excluded if insufficient data were presented to calculate mortality rates at follow-up in the depressed and nondepressed groups. We excluded studies in which the instrument for assessing depression was not standardized (e.g., studies relying on self-report of antidepressant use to assess depression, those using nonstandardized interviews, and those using only one question), studies based on trials examining the effects of an intervention, and studies in children and adolescents.
Data Extraction and Quality Assessment
We assessed the validity of studies with a quality rating scale based on the instrument developed by Hayden et al. (
17). We adapted the specific items but retained five of the six basic areas of potential bias: study participation (the study sample represents the population of interest on key characteristics), study attrition, adequate outcome measurement, adequate measurement of confounding variables, and adequate statistical analysis. The sixth area of potential bias (the prognostic factor of interest is adequately measured) was not used because an adequate measure of depression was used as an inclusion criterion for this study. The instrument is presented in Appendix C in the online
data supplement, and the ratings for included studies are presented in Appendix D. Ratings were conducted by two independent researchers, and disagreements were resolved by discussion. Agreement between raters after the first ratings was good for four of the five areas (kappa values for attrition, outcome measurement, measurement of confounders, and statistical analysis ranged from 0.69 to 0.78) but was moderate (0.56) for study participation (
18).
To assess excess mortality in different community and patient groups, we first categorized the studies into community samples and various patient samples by disease. We also rated several other characteristics of the included studies: definition of depression (depression according to a self-report measure or a diagnostic interview), prevalence of depression, follow-up period, type of outcome measure (hazard ratio, relative risk, odds ratio, or exact numbers of deaths in depressed and nondepressed participants), and country/continent where the study was conducted.
Meta-Analyses
The included studies used different outcome measures to characterize the association between depression and mortality. Some reported the exact number of deaths in the depressed and nondepressed groups, while others reported the hazard ratio, the relative risk, or the odds ratio. We used the relative risk as the main outcome measure (hazard ratio can be considered to be a specific type of relative risk adjusted for time to death; the odds ratio approximates the relative risk when the outcome, in our case mortality, is 10% or lower, which was the case in most studies; relative risk was calculated directly when the exact numbers of deaths per group were reported). In sensitivity analyses, we examined whether the pooled relative risks differed for each of these four types of outcome statistics.
To calculate pooled relative risks, we used the computer program Comprehensive Meta-Analysis, version 2.2.021 (
www.meta-analysis.com). Because we expected considerable heterogeneity among the studies, we calculated the pooled relative risk using a random-effects model.
To examine heterogeneity, we calculated the I
2 statistic. A value of 0% indicates no observed heterogeneity, and larger values show increasing heterogeneity, with 25% considered low, 50% moderate, and 75% high heterogeneity (
19). We calculated 95% confidence intervals around I
2 (
2,
20) using the noncentral chi-square-based approach within the heterogi module for Stata (
21). We tested for significant heterogeneity with the Q statistic.
Subgroup analyses were conducted according to the mixed-effects model (
22), in which studies within subgroups are pooled with the random-effects model while tests for significant differences between subgroups are conducted with the fixed-effects model. Bivariate meta-regression analyses were conducted according to the procedures implemented in Comprehensive Meta-Analysis. Multivariate meta-regression analyses were conducted in Stata, version 11.0 (StataCorp, College Station, Tex.).
Possible publication bias was tested by inspecting the funnel plot and by Duval and Tweedie’s trim-and-fill procedure (
23), which yields an estimate of the effect size after the publication bias has been taken into account. We also conducted Egger’s test of the intercept to quantify the bias captured by the funnel plot and tested whether it was significant.
Results
Selection of Studies
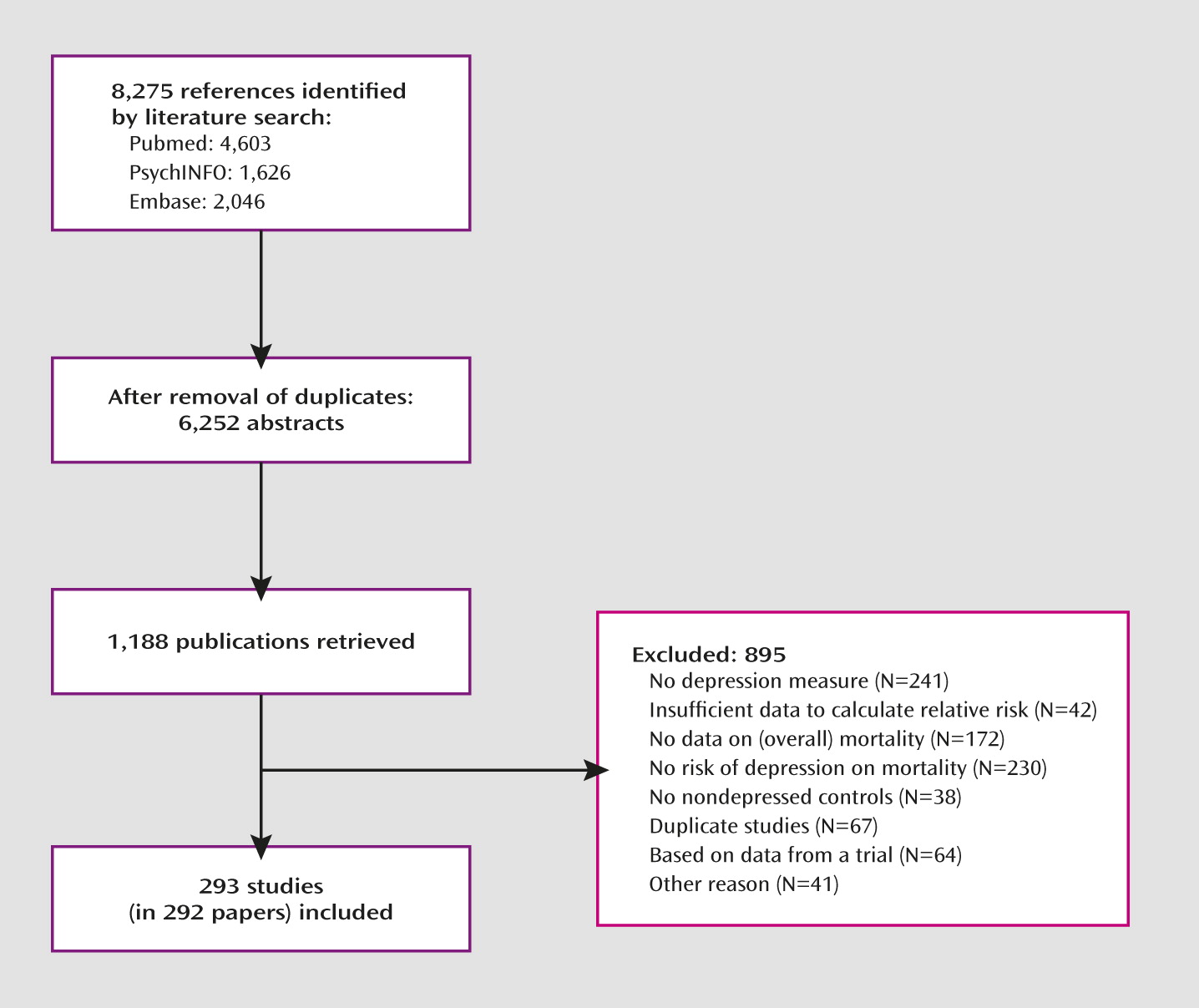
Figure 1 summarizes the study selection process. After examining a total of 8,275 abstracts (6,252 after removal of duplicates), we retrieved 1,188 full-text articles for further consideration. We excluded 895 of the retrieved articles (reasons for exclusion are provided in
Figure 1). A total of 293 studies met inclusion criteria. Characteristics of the individual studies are provided in Appendix D in the online
data supplement (references are listed in Appendix E).
Characteristics of Included Studies
The 293 studies included a total of 1,813,733 respondents, of whom 135,007 were depressed and 1,678,726 were not depressed (in studies with missing prevalence rates, we imputed these values with the pooled prevalence rates of all other studies). Selected characteristics of the 293 studies are presented in
Table 1.
The studies were conducted in 35 countries from all populated continents, although most studies were conducted in the United States (N=114) and Europe (N=115). Most studies were conducted in samples recruited from the general population (N=104), heart disease patients (N=69), cancer patients (N=29), and other patient populations (N=84). Depression was established by diagnostic interview in 82 studies and by a self-report measure in 211 studies. Follow-up periods varied widely; we categorized them as <1 year (N=56), 1–5 years (N=125), 6–10 years (N=84), and >10 years (N=38). Most studies were conducted after the year 2000 (N=216). All case-control studies were nested case-control studies.
The quality of the included studies varied (see Appendix D in the online
data supplement). In the domain of study participation, 164 studies (56%) scored positive; 186 studies (64%) scored positive on study attrition, 201 (69%) on outcome measurement, 121 (41%) on confounding measurement and account, and 217 (74%) on analyses. After summing up the individual items, we found that 90 studies (31%) had a total score of 3 or less, 104 (36%) a score of 3.5–4, and 99 (34%) a score of 4.5–5.
Excess Mortality in Depressed Versus Nondepressed Participants: Unadjusted Relative Risks
Of the included 293 studies, 238 reported unadjusted outcomes. The overall unadjusted relative risk of mortality in depressed relative to nondepressed participants in these 238 studies was 1.64 (95% CI=1.56–1.72). Heterogeneity was high and significant (I
2=83, 95% CI=80–84). Exclusion of potential outliers (studies reporting a relative risk ≥4 or <0.25) did not reduce heterogeneity and had only a small effect on the overall relative risk (1.58, 95% CI=1.51–1.65). The results of these meta-analyses are summarized in
Table 2.
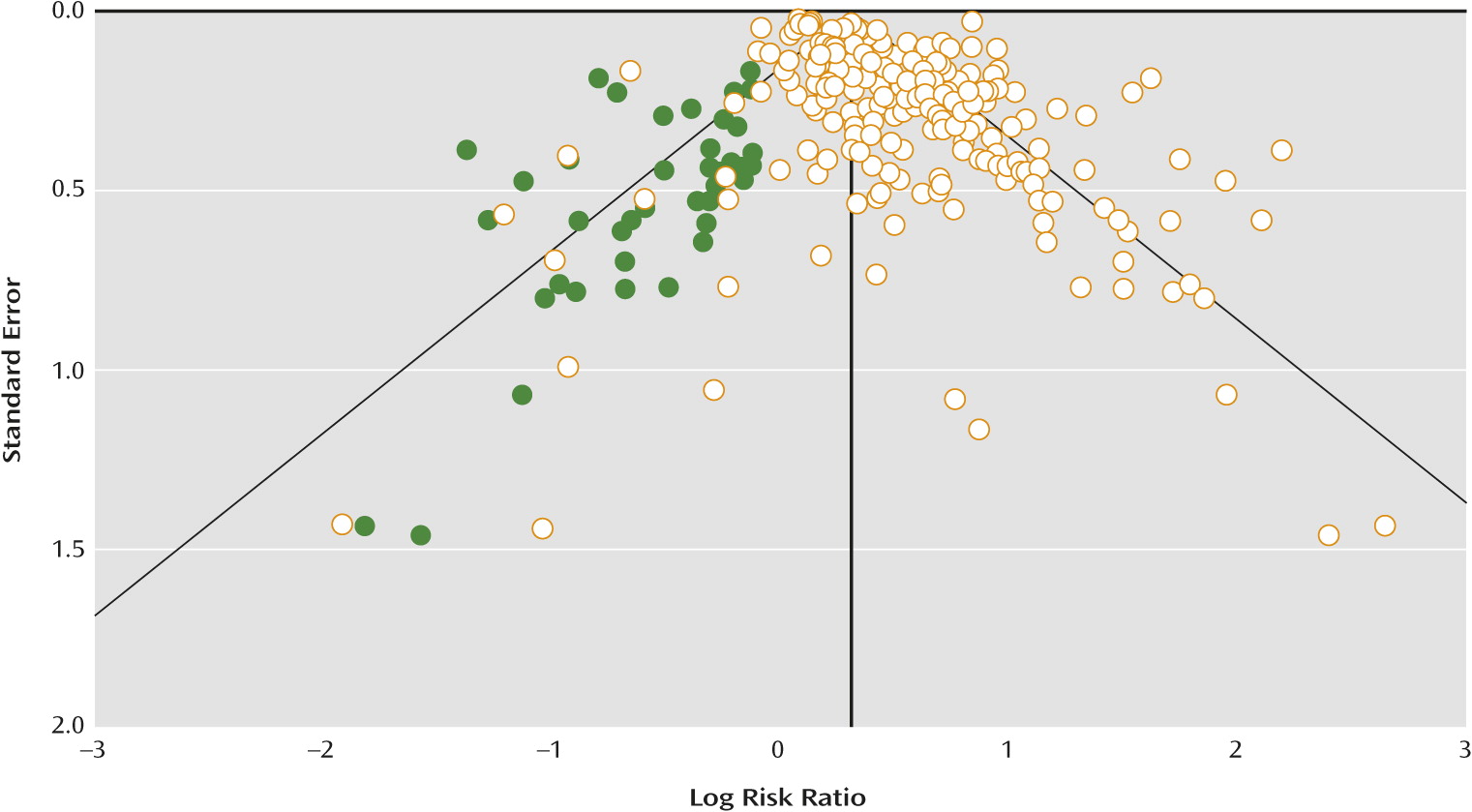
After adjustment for publication bias with Duvall and Tweedie’s trim-and-fill procedure, the overall relative risk was reduced to 1.52 (95% CI=1.45–1.59; the number of filled studies was 41). Egger’s test also pointed toward significant publication bias (intercept=1.40, 95% CI=1.01–1.81; p<0.001). A funnel plot with the imputed studies is presented in
Figure 2.
Excess Mortality of Depression in Patient and Community Samples
We examined the difference in excess mortality between patient and community samples using subgroup analyses. We found some indications that the mortality rates differed among the populations in our meta-analysis (
Table 2; p<0.05). A higher mortality level was found especially in patients with chronic obstructive pulmonary disease (COPD). A direct comparison between the studies of COPD patients and other populations resulted in a highly significant difference (p=0.002). When we removed the studies of COPD patients from the analyses, the remaining populations did not differ significantly from each other.
We conducted several additional sensitivity analyses. First, we excluded the community samples from the analyses (these studies covered more than 90% of the total number of participants included in this meta-analysis; the studies on COPD were not included in these analyses either). The remaining subgroups of studies did not differ significantly from each other. In another analysis, we included only the three largest groups of studies (heart disease, cancer, and kidney diseases) and found no indication of a significant difference between these groups.
Other Subgroup Analyses
In another series of subgroup analyses, we examined whether excess mortality was higher in some groups than in others (
Table 2). We found no indication that the relative risk differed between studies that used different measures to define depression (depression according to a diagnostic interview or self-report measure); studies in which different outcome statistics were used (relative risk, hazard ratio, odds ratio, or reported numbers of deaths), and studies conducted in different parts of the world (United States, Europe, other Western countries, East Asia, and other countries).
We found that the relative risk was inversely related to the length of follow-up (p<0.001). We conducted a bivariate meta-regression analysis with time to follow-up (as a continuous variable) as predictor and excess mortality as dependent variable. These analyses also indicated that time to follow-up was a significant predictor of excess mortality (slope=−0.015; 95% CI=−0.017 to −0.013; p<0.000).
We also found that the quality of studies was associated with relative risk. Higher risk of bias indicated higher excess mortality of depression. After summing up the individual items to a total risk of bias score (ranging from 1 [lowest] to 5 [highest]), we conducted a subgroup analysis of the studies with the lowest to the highest risk of bias. As can be seen in
Table 2, these analyses indicated that the relative risk was higher in studies with a high risk of bias, while studies with a lower risk of bias indicated a lower, although still significantly elevated, relative risk (p=0.04).
Multivariate Meta-Regression Analyses
To examine the difference in excess mortality between the patient and community samples after adjustment for other characteristics, we conducted a multivariate meta-regression analysis. We used the relative risk as the dependent variable and the variables presented in
Table 2 as predictors. As shown in
Table 3, the higher relative risk in studies of COPD patients remained significant in these analyses. None of the other types of patient or community samples were significant after adjustment for the other characteristics of the studies. We also found that the two other variables that were significant in the subgroup analyses (time to follow-up and risk of bias) remained significant in the multivariate analyses.
We also conducted a (manual) back-step meta-regression analysis, in which we dropped the least significant variable in each step until only significant predictors were retained in the model (
Table 3). The results of this parsimonious model indicated that the three variables that were found to be significant in the full multivariate meta-regression analysis (COPD patients, time to follow-up, and risk of bias) remained significant.
Analyses of Adjusted Outcomes
A considerable number of studies reported the association between depression and excess mortality after adjustment for confounders. To pool the results of studies with adjusted outcomes, we grouped the studies reporting adjusted outcomes into four categories in which the relative risk was 1) adjusted for demographic variables; 2) adjusted for lifestyle (at least one lifestyle variable, such as smoking, body mass index, exercise, weight; some studies adjusted simultaneously for one or more demographic variables); 3) adjusted for illness-related variables indicating the severity of a disorder or the presence and severity of comorbid disorders (with or without simultaneous adjustment for demographic variables); and 4) adjusted for lifestyle and illness-related factors. As can be seen in
Table 4, the overall relative risk decreased somewhat after adjustment for these variables, with a lower relative risk when more categories of variables were entered into the models.
There were few indications of significant differences between community and patient samples for adjusted mortality risks. There was, however, a significant difference between subgroups in the studies in which the results were adjusted for illness-related factors (p<0.05). In studies of heart disease patients especially, the relative risk was higher than in other populations.
Because of the considerable differences between the variables for which the outcomes were adjusted in individual studies, the relatively small number of studies in each of the four categories, and the high level of heterogeneity of the pooled outcomes, we did not conduct any additional analyses with these samples.
Discussion
In this meta-analysis we did not find strong indications that excess mortality associated with depression is significantly higher in one or more patient groups or in community-based samples, except for a significantly higher risk in studies of COPD patients. Our observation that the association between depression and mortality is not strikingly different between community-based samples and patient samples suggests that the association between depression and mortality may be explained better by generic mechanisms, such as biological dysregulations and lifestyle factors that have a general impact on health, than by disorder-specific mechanisms, such as vascular endothelial dysfunction, stimulated tumor growth, or increased platelet aggregation.
It is not clear why the studies of COPD patients resulted in a higher risk of mortality than those of other (patient and community-based) samples. It is possible that this is a chance finding, because the number of studies was relatively low (N=7). However, it is also possible that this finding is related to COPD-related variables, such as airflow limitation, hypercapnia, hypoxemia, increased dyspnea, and poor nutritional status, all of which have been found to be risk factors for mortality in COPD patients (
24), which in turn may somehow be related to depression.
The fact that for most categories of studies no significant differences were found in mortality rates according to depression status should be considered with caution. The specific patient groups may not be as distinct as they appear, as these patients may very well have suffered from all kinds of comorbidities. Quite a few patients with cancer also have heart disease, and many patients with diabetes also have renal disease. Thus, deaths occurring in these populations may not be related to the disease being studied but to a comorbid disease. For example, cardiac death is common among diabetes patients. In addition, even when mortality rates are comparable in different populations, that does not automatically mean that the mechanisms leading to death are the same in the different populations. For example, nonadherence to medication use may be life-threatening in one population but not in another, and elevations of a particular inflammatory marker may have different implications for a cancer patient than for a patient with heart disease.
We also found in our meta-analysis that heterogeneity of the pooled relative risk was considerable. This suggests that other factors that we did not examine in this meta-analysis had a considerable influence on the outcomes, and we cannot rule out the possibility that some of these factors are disease specific. It is also possible that the heterogeneity may be explained in part by depression-related variables that we did not measure, such as severity, number of depressive episodes, and duration of illness. However, in this context it is remarkable that we did not find any significant differences in the excess mortality rates for psychiatric diagnoses of depression, which are generally more severe, than for self-reported symptoms of depression, which often indicate subthreshold depression (
25). Therefore, more research is needed to establish the exact mechanisms connecting depression and excess mortality.
This meta-analysis confirmed that there is a highly significant association between depression and excess mortality at follow-up. However, we found indications that this association may have been overestimated in earlier research because of publication bias and because of a stronger association between depression and excess mortality in studies of lower quality. Despite the likely overestimation, the association remains highly significant, even after adjustment for publication bias and low quality.
This study showed once again that depression is an important clinical and public health problem. Because of the high prevalence of depression, the associated excess mortality may have a high impact on public health. An earlier study (
25) found, for example, that the population attributable fraction of major depression was 10%, indicating that mortality rates would go down 10% if depression could be eliminated completely. For clinicians, it is also important to realize that depression is associated with excess mortality, and the assessment of physical health in depressed patients is always important.
Prevalence rates of depression may vary, with higher rates in patient groups than in community samples. When the prevalence of depression is higher, the public health impact on mortality is also higher (i.e., higher population attributable risk), although the relative risk is the same in higher- and lower-prevalence populations.
This study has several strengths and limitations. The major strength is its broad scope and the large number of included studies and participants, which allowed us to directly examine whether excess mortality is comparable across different populations. At the same time, however, this is also one of the limitations of the study. Such a broad scope inevitably results in high levels of heterogeneity, and we were unable to identify the causes that can fully explain this heterogeneity. Another limitation is that the quality of many of the included studies was not optimal, and this may have affected our outcomes, especially since we found a significant association between study quality and outcome.
Despite these limitations, however, this study has once again confirmed a significant association between depression and excess mortality at follow-up. This excess mortality is comparable in community samples and most patient populations, and although the evidence is not conclusive, this suggests that generic and not disease-specific mechanisms may be the most likely mechanisms for the excess mortality among depressed persons.