In 2009, 29% of young adults lacked health insurance, exceeding rates for other age groups. Because of this historically low insurance rate, coverage is expected to change most for young adults as a result of the March 2010 Patient Protection and Affordable Care Act (ACA) (
1). The first major provision of the ACA, which required insurers to extend dependent coverage eligibility until age 26, took effect in September 2010. Since then, insurance coverage has risen by 3 to 10 percentage points for 19- to 25-year-olds, originating largely from private insurance coverage (
2–
5). As the ACA’s implementation continues, the major questions shift from tracking uninsurance rates to understanding changes in access to care and health care use. To date, limited evidence on early effects of ACA coverage suggests that patients face fewer financial barriers to care, that the share of emergency department visits covered by private insurance has increased, and that the likelihood of having a usual source of care has not changed (
5,
6).
In this study, we examined young adults’ hospital-based care for psychiatric diagnoses (all mental disorders as well as substance use disorders specifically). Mental disorders are the most prominent health conditions facing young adults. Most mental disorders emerge by age 24 (
12), and the prevalence of mental illness peaks at ages 18–25 (
13). Primary diagnoses of psychiatric disorders constitute 16% of non-childbirth-related inpatient admissions in this age group (
14). Mental health conditions have additional significance because they often coincide with poor education and employment outcomes (
15–
17). Hospital-based care is important for this age group. For example, young adults have high rates of emergency department use; one in four 18- to 24-year-olds visited an emergency department in 2010 (
18).
The ACA, and its reinforcement of the 2008 federal parity law, increased the generosity of coverage for mental health care (
19). However, the implications of coverage expansions for young adult utilization of care are poorly understood, and some fear that mental health treatment will accelerate cost growth for this age group (
20). A recent study of the 2006 health reform in Massachusetts (
14) found that young adults, after experiencing significant insurance coverage gains, had fewer inpatient admissions and emergency department visits for psychiatric problems compared with other states and age groups. These results may not generalize to the ACA dependent coverage expansion, given that Massachusetts has more psychiatrists per capita and higher hospitalization rates than other states. In addition, the ACA’s extension of private dependent coverage to 19- to 25-year-olds was more limited than the Massachusetts reforms, which enacted individual mandates, insurance reforms, and expansions of public and private insurance coverage simultaneously. Using national inpatient discharge data and California inpatient discharge data and emergency department visit data, we investigated short-term changes in hospital-based care for psychiatric diagnoses and source of payment for this care among young adults after implementation of the ACA dependent coverage expansions.
Method
We used three data sources from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project. To study patterns of inpatient hospitalization, we used the 2005–2011 data from the National Inpatient Samples (NIS), which are annual random samples of 20% of U.S. community hospitals. Although these data exclude specialty mental health or substance use treatment facilities, the majority of psychiatric inpatient admissions in the United States occur in nonspecialty community hospitals (
21). Using the NIS sample weights, the data are nationally representative of all inpatient admissions in the sampling frame. We complemented the NIS data by studying utilization patterns for all inpatient admissions in California’s State Inpatient Database (SID), which includes admissions to specialty mental health or substance use treatment facilities.
We studied emergency department use from 2005 through 2011 in California’s State Emergency Department Databases (SEDD), which includes the universe of emergency department records in the state. The SEDD excludes emergency department visits leading to an inpatient admission at the same facility. We confirmed our findings in a sensitivity analysis examining the unduplicated count of total emergency department visits in California, including inpatient admissions in the SID originating from any emergency department.
We selected California for analysis because it is the most populous state and because, unlike other large states, its databases of inpatient and emergency department discharges, including specialty mental health and substance use facilities, were available throughout the study period. We also selected California because insurance coverage for young adult Californians grew substantially after implementation of the ACA’s dependent coverage provision (
4). California’s discharge data employ selected age masking to protect patient confidentiality, which could bias estimated changes in hospital-based service use toward zero. (For a discussion of the methods and scope of age masking and its likely limited impact for our analysis, see the Supplemental Methods section of the
data supplement that accompanies the online edition of this article.)
Two of our three primary outcome measures were rates of non-childbirth-related psychiatric inpatient admissions and emergency department visits. For inpatient hospitalizations, we considered admissions with a primary diagnosis of any psychiatric disorder at discharge (ICD-9 codes 290.xx–319.xx), stratifying analyses for primary diagnoses of depression, psychosis/schizophrenia, substance use disorders, and all other psychiatric diagnoses as described in Table S1 in the online data supplement.
The SEDD data do not distinguish primary from other diagnoses, so we studied visits with any psychiatric diagnosis associated with the visit. We created mutually exclusive categories: depression only, psychosis only, substance use disorder only, substance use disorder and any other mental disorder, more than one mental disorder, and all other psychiatric diagnoses (see Table S1 in the data supplement), where “only” indicates the absence of other psychiatric diagnoses for that visit.
The 2005–2011 NIS data include 2,670,463 non-childbirth-related admissions, of which 430,583 had a primary psychiatric diagnosis. After applying the NIS sampling weights, those observations represent 2,136,503 admissions with a primary psychiatric diagnosis nationally, or 16% of all non-childbirth-related admissions. The 2005–2011 California SID data include 1,265,314 non-childbirth-related inpatient admissions, 254,664 (20%) of which had a primary psychiatric diagnosis. The 2005–2011 California SEDD data include 11,139,689 non-childbirth-related emergency department visits, 1,577,850 (14%) of which had any psychiatric diagnosis.
Our third primary outcome measure was the expected primary payer of each inpatient admission and emergency department visit. This measure allowed us to assess whether the likelihood that services were uninsured, or were covered by private insurance, changed after the dependent coverage expansion.
We measured inpatient admissions and emergency department visits as rates per 1,000 population, following methods used to study the effects of previous insurance expansions (
14,
22). We created 616 “cells” defined by age (for each year from ages 19 to 29), sex, and quarter (for 2005 through 2011). In each cell, numerators reflect total admissions for that age-sex-quarter group. The denominators are the U.S. Census Bureau’s national and state-level population estimates corresponding to the numerators from the NIS, the SID, and the SEDD (
23).
Statistical Analysis
We used a difference-in-differences research design, estimating differential changes in hospital-based service use among young adults with psychiatric diagnoses before and after the dependent coverage expansions. We compared changes for ages targeted by the provision, 19- to 25-year-olds, relative to 26- to 29-year-olds, an otherwise similar group in terms of levels and trends in service use but not targeted by dependent coverage changes.
Although the dependent coverage provision went into effect on September 23, 2010, a number of large insurers extended dependent coverage through age 25 before the formal implementation date to prevent gaps in coverage for new graduates (
24). Previous research (
2) found significant increases in parental employer-sponsored insurance coverage during this interim period, although these increases appear to reflect shifting of sources of insurance for young adults, and rates of insurance coverage remained unchanged. Because of this complex transition, we defined the second and third quarters of 2010 as the “interim” expansion period, and we defined the fourth quarter of 2010 and later as the post-dependent coverage expansion period.
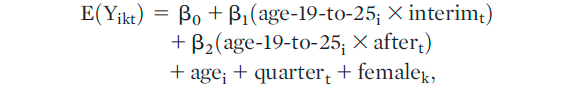
For each outcome, we estimated the following linear regression model:
where Y
ikt=admissions or visits per 1,000 population for age
i, sex
k, and quarter
t. The term age
i represents a set of 10 indicator variables for each individual year of age. Quarter
t is a set of 27 indicator variables for each quarter (excluding the first), which controls for secular trends and seasonality in the outcome. We created an interaction term between the variables “interim” (coded as 1 for April through September 2010, and 0 otherwise) and “age 19 to 25
i” (coded as 1 for age 19–25 rates, and 0 otherwise). We created a second interaction between “after
t” (coded 1 for after September 2010, and 0 otherwise) and “age 19 to 25
i”. The coefficient β
1 is interpreted as the differential change in inpatient or emergency department use between the affected age group and the comparison age group during the interim implementation period of the dependent coverage expansion, and the coefficient β
2 yields the differential change in inpatient or emergency department use between the affected and comparison age groups after the dependent coverage expansion went into effect. The inclusion of the full set of indicator variables for single year of age and quarter obviates the need to include main effects for the “age 19–25,” “interim,” and “after” variables. We estimated additional models stratified by sex, because of known sex differences in the incidence and prevalence of specific mental disorders and in initiation and course of treatment (
25–
28). We estimated our regression models with robust Huber-White standard errors, and we report p values based on two-tailed t statistics.
Dartmouth College’s Committee for the Protection of Human Subjects reviewed the study and deemed it exempt from the need for consent because it uses secondary data.
Results
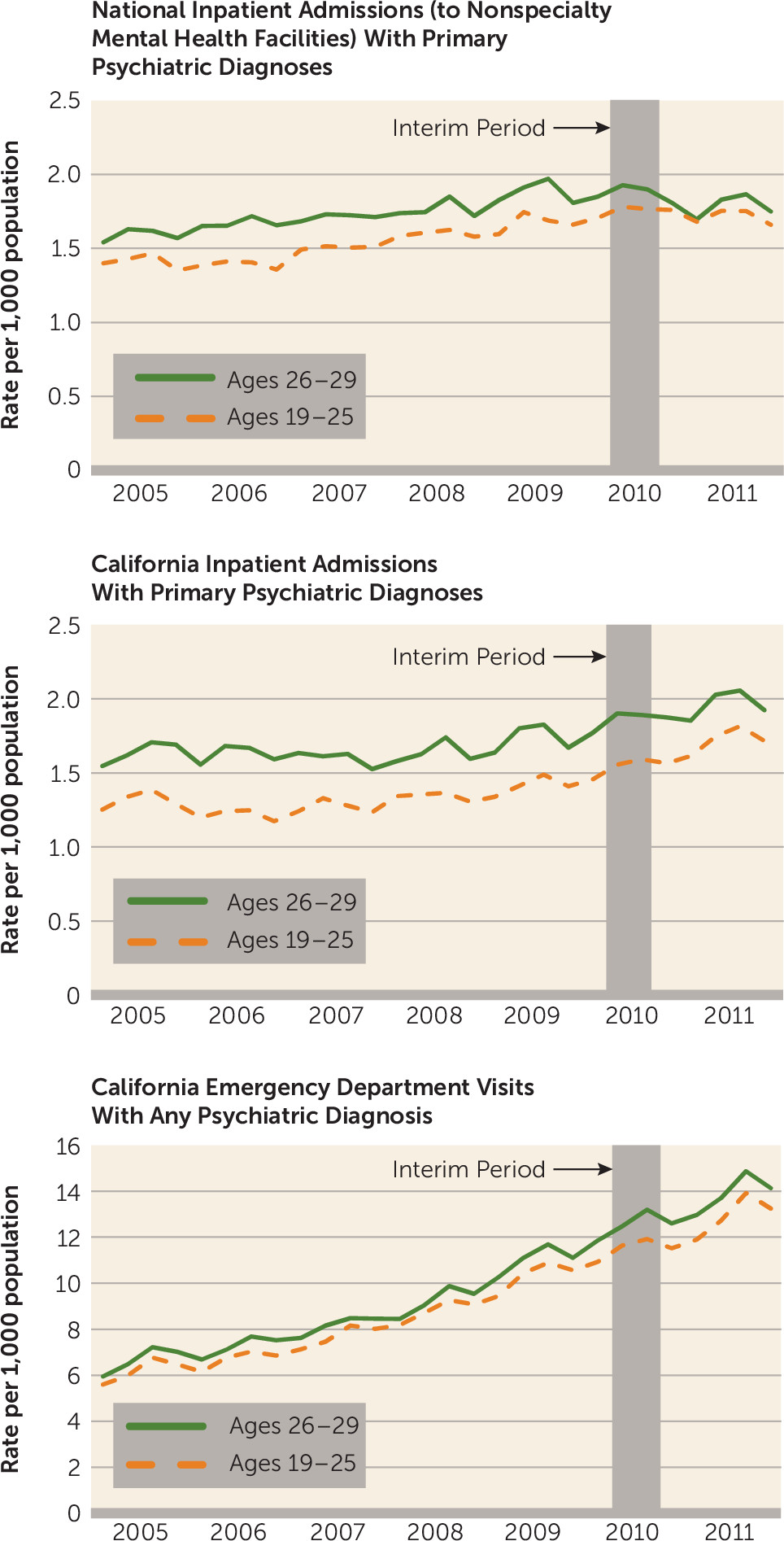
Use of hospital-based services increased over the study period (
Figure 1). Trends in outcomes were similar between the two age groups before the dependent coverage expansion, validating the difference-in-differences research design. The national quarterly inpatient hospitalization rate at nonspecialty hospitals during the study period was 1.58 per 1,000 for 19- to 25-year-olds and 1.75 per 1,000 for 26- to 29-year-olds, with slightly lower rates in females than in males. In California, the average quarterly inpatient admission rate was 1.40 per 1,000 for 19- to 25-year-olds and 1.72 per 1,000 for 26- to 29-year-olds, while the average quarterly emergency department visit rates were 9.17 per 1,000 for 19- to 25-year-olds and 9.83 per 1,000 for 26- to 29-year-olds (
Table 1). The trends in the emergency department visit rates before implementation of the ACA dependent coverage expansion were similar across age groups, just as they were for inpatient admissions, validating our choice of comparison group (for statistical evidence that trends were parallel, see the Supplemental Methods section in the online
data supplement). Psychiatric diagnoses were common: 16% of non-childbirth-related inpatient admissions to community hospitals nationally involved a psychiatric diagnosis, 20% of non-childbirth-related inpatient admissions in California for 19-to 25-year-olds had a primary psychiatric diagnosis, and 14% of emergency department visits in California for 19- to 25-year-olds involved a psychiatric diagnosis.
Inpatient admissions with a psychiatric diagnosis to nonspecialty hospitals increased more for 19- to 25-year-olds than for 26- to 29-year-olds after the dependent coverage provision (0.14 per 1,000, p<0.001;
Table 2). The differential rise in inpatient admissions was smaller during the interim implementation period and fell short of statistical significance (β
1=0.06, p=0.063). The dependent coverage expansion was associated with significant increases in inpatient admission rates for all of the specific primary psychiatric diagnoses (see Table S2 in the online
data supplement). After stratification by sex, the increases in inpatient admissions were positive and statistically significant for both males and females. However, the increase was significantly larger for males. Inpatient admissions also differentially rose for males during the interim implementation period (β
1=0.10, p=0.008). Significant increases for males were found in each psychiatric category, but only depression and psychosis admissions increased significantly more for females among 19- to 25-year-olds compared with 26- to 29-year-olds (see Table S2). In the California inpatient data, estimates were similar to the national data, with smaller estimated effects and wider confidence intervals. Inpatient admission rates did not significantly increase overall or for females. However, for males, admissions grew 0.12 per 1,000 more among 19- to 25-year-olds compared with 26- to 29-year-olds (p=0.011). Among the specific psychiatric categories in the full California sample, only admission rates for substance use disorders and for other psychiatric diagnoses increased significantly (see Table S3 in the
data supplement). Both increases were significant for males, whereas only the increase in substance use disorder admissions was significant for females.
In contrast to the inpatient results, the dependent coverage expansion was associated with significantly slower growth in the rates of emergency department use with any psychiatric diagnosis. In California, growth in emergency department visits not leading to inpatient admission was 0.45 per 1,000 (p<0.001) lower among 19- to 25-year-olds than among 26- to 29-year-olds after the coverage expansion (
Table 2). The differential reduction in emergency department use was observed in the interim implementation period as well (β
1=−0.51, p<0.001). After stratification by sex, the slower growth in emergency department visits with psychiatric diagnoses after the coverage expansion was significant for females (β
2=−0.81; p<0.001) but not for males (β
2=−0.09; p=0.544). The difference in trends of emergency department use significantly dropped during the interim implementation period for females (β
1=−0.69, p<0.001) but not for males (β
1=−0.32, p=0.063). We found significantly slower growth in emergency department visits within all diagnostic categories except other psychiatric diagnoses (see Table S4 in the online
data supplement). Mirroring the results for all emergency department visits with psychiatric diagnoses, the slower growth in visits for specific diagnoses were significant, except visits for other psychiatric diagnoses for females. For males, only the reduction in psychosis-related emergency department visits was significant, and rates of emergency department visits categorized as other psychiatric diagnoses increased faster among 19- to 25-year-olds than among 26- to 29-year-olds (0.11; 95% CI=0.03, 0.19). Sensitivity analyses estimating trends in rates of emergency department visits, including visits resulting in admissions at the same facility, yielded virtually identical results (see Table S5 in the
data supplement).
After the dependent coverage expansion, the probability that inpatient admissions and emergency department visits for psychiatric diagnoses were uninsured decreased (
Table 3). The probability that inpatient admissions were uninsured fell 2.9 percentage points nationally among 19- to 25-year-olds compared with 26- to 29-year-olds after dependent coverage expansions (p<0.001), and by 2.8 percentage points in California (p<0.001). The probability of uninsured emergency department visits in California dropped by 3.9 percentage points (p<0.001). After stratification by sex, estimated reductions in uninsured discharges were statistically significant, though larger in magnitude for males than females. The likelihood that hospital-based care was uninsured did not significantly change during the interim implementation period. However, the share of hospital-based care that was covered by private insurance increased significantly both in the interim implementation period and in the postexpansion period (see Table S6 in the online
data supplement).
Discussion
After the ACA’s expansion of dependent coverage eligibility until age 26, use of inpatient psychiatric care in nonspecialty hospitals rose modestly faster for young adults targeted by the expansion compared with young adults above the age cutoff. These increases were stronger for males, led by growth in admissions for psychosis and substance use disorders. The picture from emergency departments in California differs. Dependent coverage expansions coincided with slightly smaller increases in rates of emergency department visits with psychiatric diagnoses among 19- to 25-year-olds compared with 26- to 29-year-olds. After implementation of the dependent coverage expansions in the ACA, both inpatient and emergency department services with psychiatric diagnoses for 19- to 25-year-olds were less likely to be uninsured, consistent with early evidence provided by Mulcahy and colleagues on emergency department use for emergent conditions (
6). The likelihood that hospital-based care for psychiatric diagnoses was covered by private insurance also rose. This rise started immediately after enactment of the ACA and increased after the dependent coverage expansion was fully implemented, consistent with evidence provided by Akosa Antwi and colleagues (
2). That the increase in private insurance preceded declines in uninsurance may suggest that early adopters of dependent coverage moved from government-sponsored coverage, although we cannot rule out other explanations.
Rates of inpatient admissions for psychiatric diagnoses increased 8.4% relative to the pre-expansion rates. Our results, combined with the U.S. Census Bureau’s 2010 estimate of 29.7 million Americans ages 19–25, imply an increase of 16,632 mental health-related inpatient admissions per year. To put these findings in perspective, consider that the existing research using data through 2011 finds that the proportion of 19- to 25-year-olds with insurance increased by between 4.8% and 6.9% relative to levels of coverage before the dependent coverage expansion, with over 3 million gaining coverage by the end of 2011 (
2,
4,
5,
29). In addition, many more young adults responded to the ACA’s dependent coverage expansion by switching from individually purchased or employer-sponsored plans in their own names to parental plans (
2,
30). It is plausible that these young adults received more comprehensive and generous coverage under parental policies. Increased insurance could lead to more clinically appropriate hospitalizations if necessary services become more affordable because of expanded insurance, or if greater access to outpatient services identifies the need for hospitalization. To the extent that this happened, additional hospitalizations, though cost increasing, would coincide with good clinical care. Changes in emergency department visit rates after ACA implementation suggest beneficial effects of the dependent coverage expansion. In California, emergency department visits with psychiatric diagnoses were 4.9% lower than before coverage expansion. Based on the size of the 19- to 25-year-old population in 2010 in California (
23), our results imply that the number of annual emergency department visits with psychiatric diagnoses dropped by 7,044 in a large and diverse state with low levels of insurance coverage relative to national averages. One possible explanation for this result is that improved access to outpatient psychiatric care more than offset any increased incentives to use the emergency department because of expanded private insurance coverage. We find that the reductions in emergency department use started immediately after the ACA was enacted and that the proportion of visits covered by private insurance also started to rise during the 6-month interim implementation period. Understanding how patterns of outpatient psychiatric service use change in response to the ACA’s insurance expansions is a priority for future research. However, this result may also reflect the possibility that the insurance coverage that was gained after the dependent coverage expansion relied on managed behavioral health techniques (such as 24-hour nurse triage lines) to facilitate the use of less-expensive outpatient settings and minimize more expensive treatment modalities such as emergency departments (
31).
Our inpatient results mirror findings describing inpatient admissions for mental illness (
10), but to our knowledge, no previous evidence has captured differences by sex or by emergency department visits, nor have any previous studies captured care in specialty mental health and substance abuse treatment facilities, as we did using California discharge data. In contrast to the recent experimental Oregon Health Study, which found overall increases in emergency department use but no increases in mental health-related emergency department use, we find declines for emergency department visits with psychiatric diagnoses (
11). The discrepancy may reflect two key differences between the Oregon study and ours. The Medicaid-eligible population in Oregon has a lower mean income and was older on average than our study population. Also, Medicaid coverage could affect emergency department use very differently than private insurance. Associations between the dependent coverage expansion and hospital-based care differed by sex. Insurance gains after the ACA were higher for males than for females, although the differences were modest (
4,
5). Inpatient admission growth was greater for males than for females, while declines in emergency department use were concentrated among females. One possible explanation is that females took greater advantage of increased access to insurance to use effective outpatient psychiatric services that reduced the need for hospital-based care. This represents an important avenue for future investigation.
Although we used a strong quasi-experimental design, our study has some limitations. First, discharge data lack clinical information to determine whether higher admission rates reflect clinically appropriate, cost-effective services or services of marginal efficacy. Second, because we did not include data on outpatient treatment, we cannot determine whether our findings are due to the provision of more effective or more frequent outpatient treatments, changes in the underlying health of the population, or restrictions on emergency department visits under managed care contracts. These gaps in knowledge underscore the importance of comprehensive data across care settings to understand the ACA’s effects.
Third, the NIS data exclude admissions to specialty psychiatric or substance use treatment facilities. However, only 58% of total inpatient mental health spending and 71% of total inpatient substance abuse spending nationwide occurs in nonspecialty hospitals (
21). In addition, we complemented the NIS data with SID data from California, which did include specialty mental health facilities, and the results were similar. However, the SID results do not achieve the level of statistical significance seen in the NIS, because of a smaller sample and the aforementioned age masking, which could shrink the magnitude of our estimates since some adults have randomly misclassified ages. Finally, we considered only the first 15 months of ACA implementation and thus cannot describe medium-term or long-term trends in hospital-based care.
As the ACA expands insurance coverage to millions of Americans, it is crucial to understand the effects of new coverage on patterns of care and spending. For young adults, a group with significant psychiatric service needs and a group likely to experience large gains in coverage as a result of the ACA, inpatient care for psychiatric diagnoses rose, emergency department use for psychiatric diagnoses fell, and the proportion of hospital-based services that were uninsured dropped after the dependent coverage expansion. Future research will assess whether these patterns will hold as the ACA expands insurance more broadly.