T
o the E
ditor: Previously, we described a late-life depression-executive dysfunction syndrome associated with disability (
1). Microstructural white matter abnormalities, common in this syndrome, are principally caused by cerebrovascular changes and contribute to executive dysfunction and resistance to antidepressants (
2).
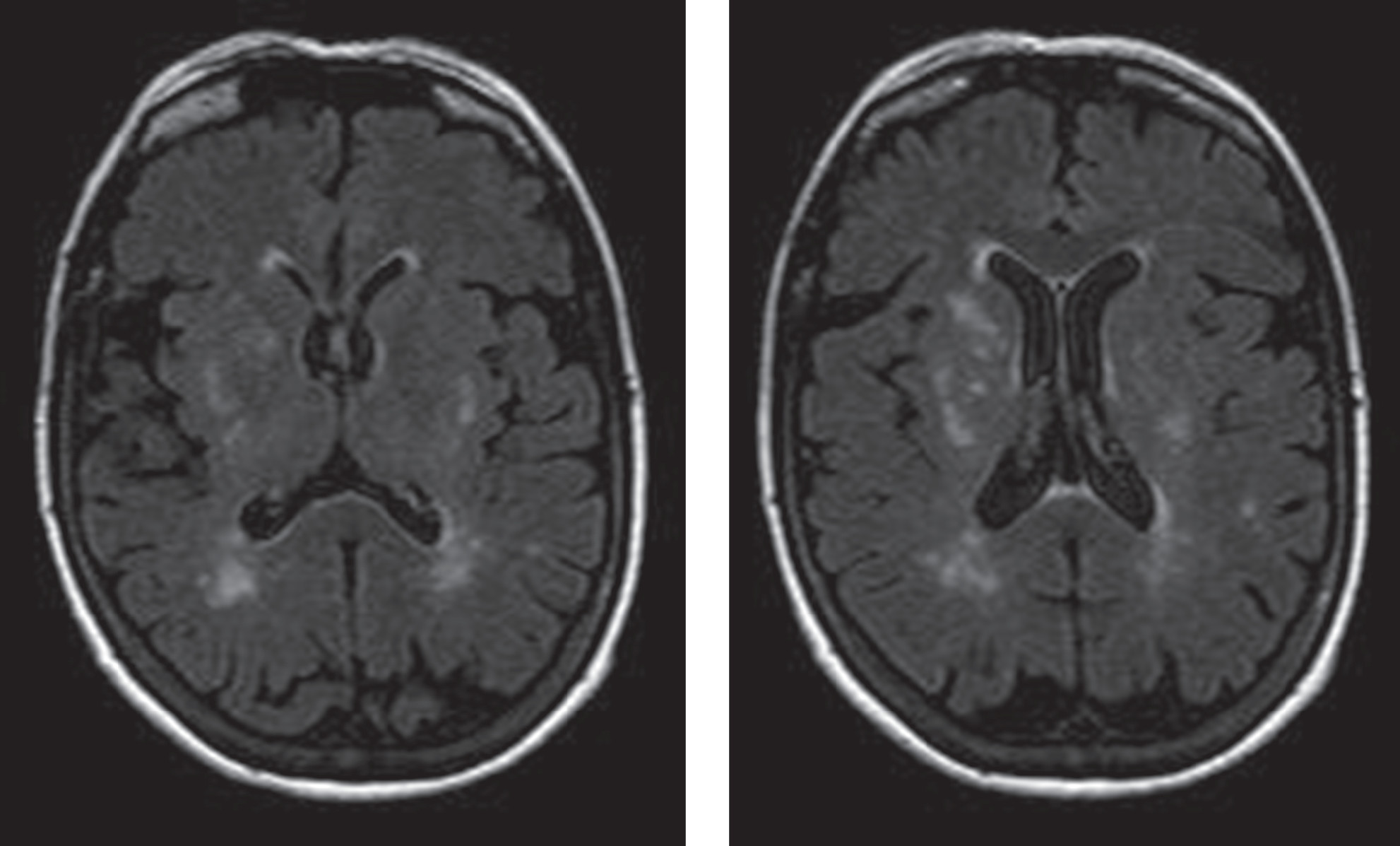
We recently treated a 71-year-old woman in the third episode of early-onset (mid-thirties) major depression, who was hospitalized after an overdose. She had a dysexecutive behavioral syndrome, prominent hyperintensities on MRI (
Figure 1), but no impairment on executive function tests. She presented with mood lability and poor monitoring of her own behavior (i.e., repetition, distractibility, and impulsivity). She performed in the average to superior range on tasks of processing speed (Trail-Making Test, Part A, 73rd percentile), cognitive inhibition (Stroop test, 66th percentile), set-shifting (Trail-Making Test, Part B, 96th percentile; Wisconsin Card Sorting Test, 61st percentile), and planning (Tower of London Test, 75th percentile). She was partially aware of her pathology, noting, “I want to change the habit of speaking out without thinking and acting impulsively.” Her husband’s report on the Frontal Systems Behavior Scale (
3) showed major abnormalities in “disinhibition,” with much milder abnormalities in the “dysexecutive” and “apathy” domains.
This patient’s behavior was consistent with ventromedial cortex dysfunction. Lesions in this area may disconnect frontal monitoring systems from limbic output, resulting in prominent mood lability, behavioral disinhibition, and inappropriate behavior and judgment (
4). Patients with ventromedial cortex dysfunction may have intact executive functioning primarily served by dorsolateral prefrontal cortex and dorsal anterior cingulate circuitry (
4).
Behavioral abnormalities related to the ventromedial cortex have seldom been investigated in late-life depression. We recently conducted a cluster analysis of 52 adults with late-life depression and identified three patient subgroups. Cluster 1 (N=20) performed poorly on a task requiring ventromedial cortex integrity (Iowa gambling task) but performed well on cognitive control tasks (Stroop Color and Word Test, Tower of London Test) and had no apathy. Cluster 2 (N=19) performed well on the Iowa gambling task, had impaired performance on the Stroop Color and Word and Tower of London tests, and had mild apathy. Cluster 3 (N=13) performed well on the Iowa gambling task, the Stroop Color and Word Test, and the Tower of London Test but had significant apathy. Impairment in risk-sensitive decision making has been documented in older suicide attempters (
5), suggesting that select patients may present with ventromedial cortex impairment. We suggest that disinhibited behavior, dissociable from cognitive control dysfunction, characterizes a subgroup of late-life depression whose neurobiology and treatment response require investigation.