Prenatal Primary Prevention of Mental Illness by Micronutrient Supplements in Pregnancy
Abstract
The Developmental Context of Prenatal Prevention
Possible Strategies for Prenatal Prevention and their Investigation
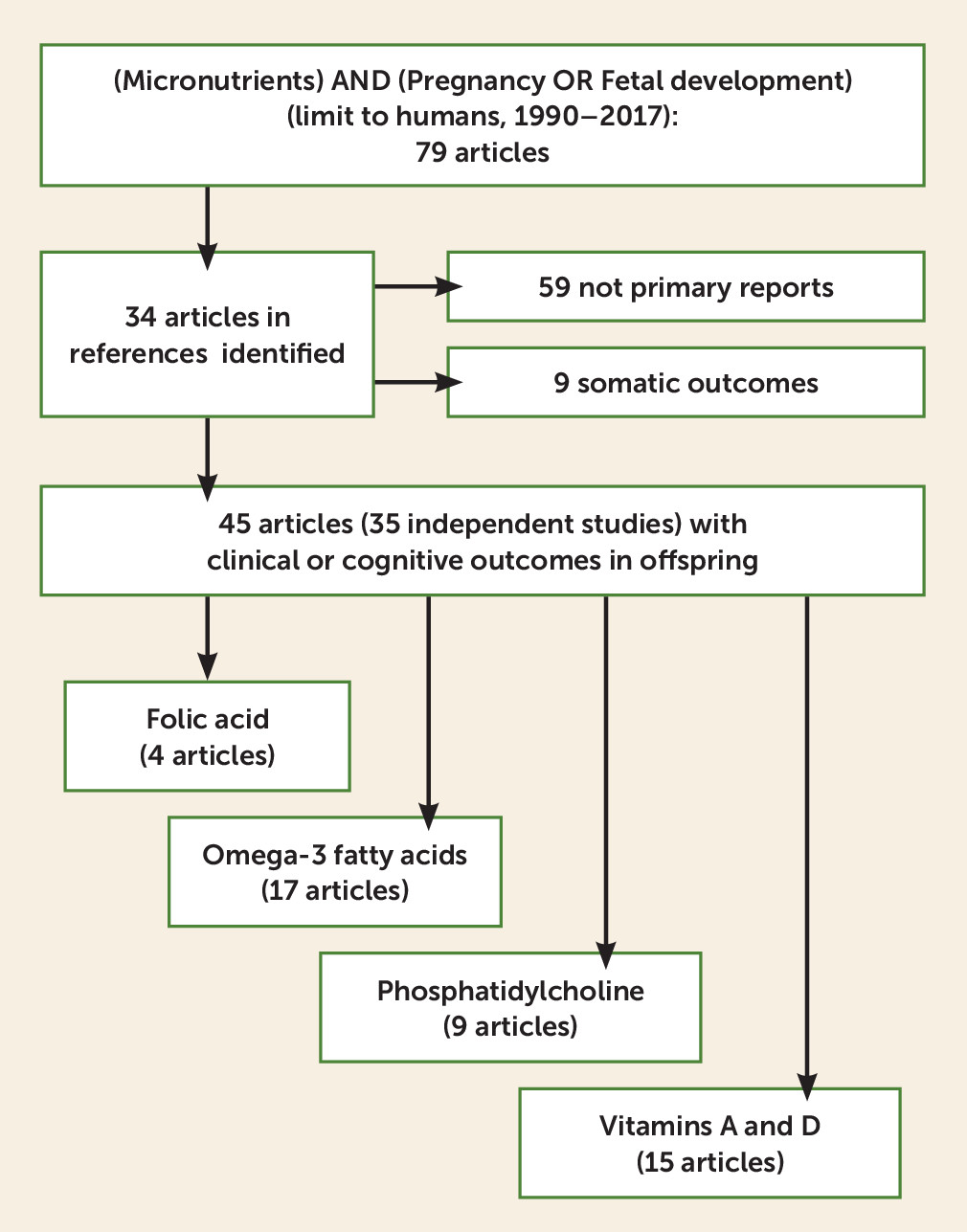
Method
| Type of Trial | Subjects | Region or Country | Dose or Level and First Timing During Gestation | Effect | Limitations |
|---|---|---|---|---|---|
| Folic acid | |||||
| Prospective, randomized (25) | 311 women | Europe | 400 μg of 5-methyltetrahydrofolate compared with placebo at 20 weeks | Decreased reaction time with distractor at 8.5 years (d′=0.32) | 130 of 311 children studied; no clinical ratings |
| Prospective, observational (26, 27) | 3,210 women | Netherlands | ≥400 μg of folic acid within first 10 weeks’ gestation compared with no or later use | CBCL problems at 18 and 36 months; top 17th percentile (odds ratio=1.45, 95% CI=1.14–1.84) | Groups differ in sociodemographics; folic acid neonates 200 g heavier |
| Prospective, observational (14) | 573 infants with facial clefts, 763 controls | Norway | ≥400 μg of folic acid within 9 weeks | Decreased facial clefts (odds ratio=0.61, 95% CI=0.39–0.96) | Not effective in cleft palate without cleft lip |
| Prospective, randomized (15) | 1,817 women, prior neural tube defect | U.K., Europe, Israel, Australia, Canada, U.S.S.R. | 4 mg of folic acid at preconception until 12 weeks | Decreased neural tube defects (odds ratio=0.28, 95% CI=0.12–0.71) | No follow-up of other developmental traits |
| Retrospective, observational (28) | 104,428 women | United States | 400 μg of folic acid at first trimester | Increased asthma at 4.5–6 years (odds ratio=1.2, 95% CI=1.1–1.3) | Data only from Medicaid claims |
| Phosphatidylcholine | |||||
| Prospective, randomized (29, 30) | 100 women | United States | 6,300 mg of phosphatidylcholine at 15 weeks | Increased 1-month EEG sensory gating; decreased 3.5-year CBCL attention (d′=0.59) and social (d′=0.79) problems | 50% attrition; parental CBCL reports only |
| Prospective, observational (31) | 154 women | Canada | Plasma choline at 16 weeks’ gestation | Increased Bayley cognition score at 18 months (β=6.054, SE=2.283) | Healthy women in uncontrolled study |
| Prospective, randomized (32) | 24 women | Canada | 550 mg compared with 100 mg of choline supplements in third trimester | Lower placental sFLT1, angiogenic factor in preeclampsia (d′=0.2) | Small study with no clinical outcome |
| Prospective, observational (33) | 817 adults 33–55 years old | United States | Plasma trimethyl amine oxide, a choline bacterial metabolite | No increase in cardiac disease (odds ratio=1.03, 95% CI=0.71–1.52) | Patients were not supplemented |
| Omega-3 fatty acids | |||||
| Retrospective, observational (34) | 57 adult cases and 95 controls | United States | DHA acid >1.45% of fatty acids in second or third trimester | Increased schizophrenia spectrum (odds ratio=2.38, 95% CI=1.19–4.76) | Mercury from high fish diet not tested |
| Prospective, randomized (24) | 543 women | Australia | 800 mg of fish oil at 20 weeks | Increased 7-year Conners ADHD score (d′=0.1) | Small effect in large sample |
| Prospective, randomized (23) | 736 women and children | Denmark | 2.4 g of fish oil at 24–26 weeks | Decreased wheezing at 3–5 years (odds ratio=0.69, 95% CI=0.49–0.97) | Trend suggests vitamin D equally effective |
| Prospective, randomized (35) | 2,399 women | Australia | 800 mg of fish oil at 20 weeks | Fewer gestations at <34 weeks (odds ratio=0.49, 95% CI=0.25–0.94) | More DHA induction (odds ratio=1.28, 95% CI=1.06–1.54) |
| Vitamins A and D | |||||
| Retrospective, observational (36) | 430 adult cases, 430 controls | Denmark | 25(OH)D3 <19.7 nM compared with >51 nM, low versus high quintiles | Increased schizophrenia (odds ratio=2.1, 95% CI=1.3–3.5) | Confounded with summer birth in high quintile |
| Retrospective, observational (37) | 51 male adult cases, 4,616 in cohort | Finland | 2,000 IU of vitamin D in first year of life | Decreased schizophrenia (odds ratio=0.23, 95% CI=0.06–0.95) | Effects only in males |
| Prospective, observational (38) | 68 cases in birth cohort of 4,334 | Netherlands | <25 nmol/L of vitamin D at 20 weeks | Increased autism spectrum at 6–9 years (odds ratio=2.42, 95% CI=1.09–5.07) | Small number of cases |
| Retrospective, observational (39) | 186 cases in cohort of 1,194 | New Zealand | Vitamin D intake >724 IU (highest quartile) | Decreased recurrent wheeze at 3 years (odds ratio=0.39, 95% CI=0.25–0.62) | Infection-related wheeze, not new incident asthma |
| Retrospective, observational (40) | 55 cases, 106 controls | United States | <30 μg/dL of vitamin A at second trimester | Increased schizophrenia (odds ratio=3.05, 95% CI=1.06–8.79) | Higher levels in more educated women |
| Supplement | Effect | Model Mechanism |
|---|---|---|
| Folic acid | Increased neuronal development | Deficiency lowers Stat3, allowing increased neurite outgrowth (41) |
| Imprinting of maternal genes | Biochemical role in one-carbon metabolism and methylation of DNA (42) | |
| Phosphatidylcholine | Development of inhibitory neurotransmission | Activation of α7-nicotinic receptors induces the chloride transporter NKCC1, establishing a chloride gradient for GABA inhibition (43); effects blocked in CHRNA7 null mice (43, 44) |
| Omega-3 fatty acids | Antiseizure effect in ketogenic diet but could also affect synapse formation in development | Accelerates inactivation and retards recovery of sodium and calcium channels in vitro, which decreases neuronal excitation (45) |
| Reduces preterm birth | Reduces prostaglandin E2 and F2α in uterine decidual cells (46) | |
| Vitamin D | Neuronal development | Interacts with Nurr1 to support development of dopamine neurons (47); activates low voltage (l-type) calcium channels to increase neurofilament phosphorylation (48) |
Results
Folic Acid and the Baby’s Risk for Mental Illness
Omega-3 Fatty Acids (Fish Oil)
Phosphatidylcholine
Vitamins D and A
Discussion
| Intervention | Current Recommended Daily Allowance | Study Dose, Timing | Major Developmental Finding | Other Conditions | Known Adverse Effects |
|---|---|---|---|---|---|
| Folic acid | 400–800 μgb plus 200 μg from diet | 400 μg at preconception to 10 weeks’ gestation (27) | Decreased emotional problems (child) | Decrease in cleft lip, spina bifida | Infant wheezing increased |
| Phosphatidylcholine | 3,150 mg (450 mg of choline) from diet | 6,300 mg at preconception to 16 weeks’ gestation (30) | Decreased social and attention problems (child) | Possible decrease in preeclampsia | Trimethylamine N-oxide cardiotoxicity (in men with cardiac disease) |
| Omega-3 fatty acids (fish oil) | Up to 300 g of low mercury–containing fish per week | 2.4 g of fish oil daily at 24–26 weeks’ gestation for wheeze (23) | Increased risk for schizophrenia spectrum (adult) | Premature birth and infant wheezing decreased | Increased ADHD symptoms at 7 years |
| Vitamins A and D | Supplement of 2,567 IUb of vitamin A and 600 IUb of vitamin D, plus amounts from diet and sunlight | 1,000 IU of vitamin D3 for infants up to 1 year of age, 2,000 IU in northern countries (37) | Decreased schizophrenia (adult) with both vitamins A and D | Infant wheezing decreased | Teratogenicity with vitamin A intake >8,000 IU (diet plus supplement) |
| Principal Investigator, Country | Title | Type of Trial, Dose, Timing | Principal Outcome | Registry and Date |
|---|---|---|---|---|
| C. Grant, Australia | Randomized placebo-controlled study of vitamin D during pregnancy and infancy | Randomized; mothers receive 2,000 IU of vitamin D and infants receive 800 IU, compared with 1,000 IU and 400 IU for each | Infant 25(OH) vitamin D >75 nM at 6 months | Australian New Zealand Clinical Trials Registry, ACTRN12610000483055; 2010 |
| M.C. Hoffman, United States | Choline supplementation during pregnancy: impact on attention and social withdrawal | Randomized; 9 g of phosphatidylcholine at 15 weeks | Child Behavior Checklist rating at 3.5 years | ClinicalTrials.gov, NCT03028857; 2017 |
| J. Zhu, China | Effects of genomic and metabolomic variations of choline on risk of preterm birth and clinical outcomes in preterms | Prospective, observational; effects of plasma choline level during gestation | Preterm birth incidence | ClinicalTrials.gov, NCT02841813; 2016 |
Acknowledgments
Supplementary Material
- View/Download
- 316.14 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).