Infections as a Risk Factor for and Prognostic Factor After Substance-Induced Psychoses
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
Population
Substance-Induced Psychosis
Infections
Schizophrenia
Potential Confounders
Statistical Analysis
Results
| Characteristic | N | % |
|---|---|---|
| Male | 1,158,251 | 51.3 |
| Alcohol or substance use disordera | 67,046 | 3.0 |
| Highest paternal level of education | ||
| Ninth or 10th grade | 429,852 | 19.0 |
| High school or vocational education | 1,167,151 | 51.7 |
| Bachelor’s degree or equivalent | 294,030 | 13.0 |
| Master’s-level university degree | 261,217 | 11.6 |
| Not registered in Statistics Denmark | 104,529 | 4.6 |
| Highest maternal level of education | ||
| Ninth or 10th grade | 401,047 | 17.8 |
| High school or vocational education | 982,271 | 43.5 |
| Bachelor’s degree or equivalent | 571,159 | 25.9 |
| Master’s-level university degree | 228,349 | 10.1 |
| Not registered in Statistics Denmark | 73,953 | 3.3 |
| Paternal substance use disorder | 221,283 | 9.8 |
| Maternal substance use disorder | 111,161 | 4.9 |
| Paternal psychotic disorder | 22,151 | 1.0 |
| Maternal psychotic disorder | 21,879 | 1.0 |
| Other paternal psychiatric disorder | 186,267 | 8.3 |
| Other maternal psychiatric disorder | 275,011 | 12.2 |
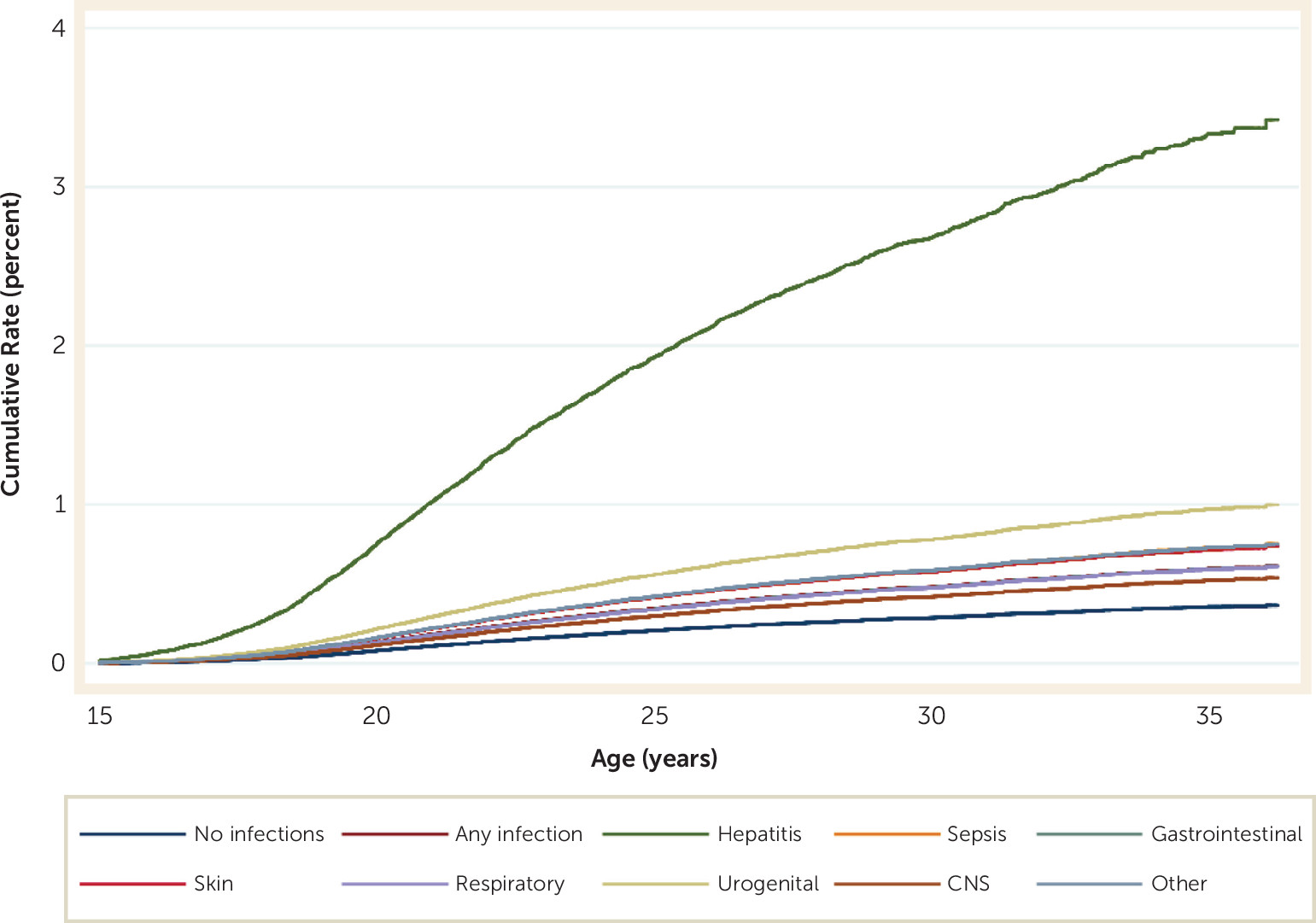
Infections as Predictors of Substance-Induced Psychosis
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Infection | Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p |
| Any infection | 1.66 | 1.56–1.76 | <0.001 | 1.30 | 1.22–1.39 | <0.001 |
| Hepatitis | 7.70 | 5.57–10.64 | <0.001 | 3.42 | 2.47–4.74 | <0.001 |
| Sepsis | 1.66 | 1.32–2.09 | <0.001 | 1.40 | 1.11–1.76 | 0.004 |
| Gastrointestinal infection | 1.39 | 1.26–1.53 | <0.001 | 1.13 | 1.02–1.24 | 0.02 |
| Skin infection | 1.69 | 1.52–1.87 | <0.001 | 1.31 | 1.18–1.46 | <0.001 |
| Respiratory infection | 1.42 | 1.31–1.53 | <0.001 | 1.11 | 1.03–1.20 | 0.006 |
| Urogenital infection | 2.30 | 1.91–2.76 | <0.001 | 1.65 | 1.39–1.99 | <0.001 |
| CNS infection | 1.19 | 0.89–1.61 | 0.25 | 1.00 | 0.74–1.34 | 0.99 |
| Other infections | 1.73 | 1.57–1.91 | <0.001 | 1.39 | 1.26–1.53 | <0.001 |
Infections and Specific Types of Substance-Induced Psychosis
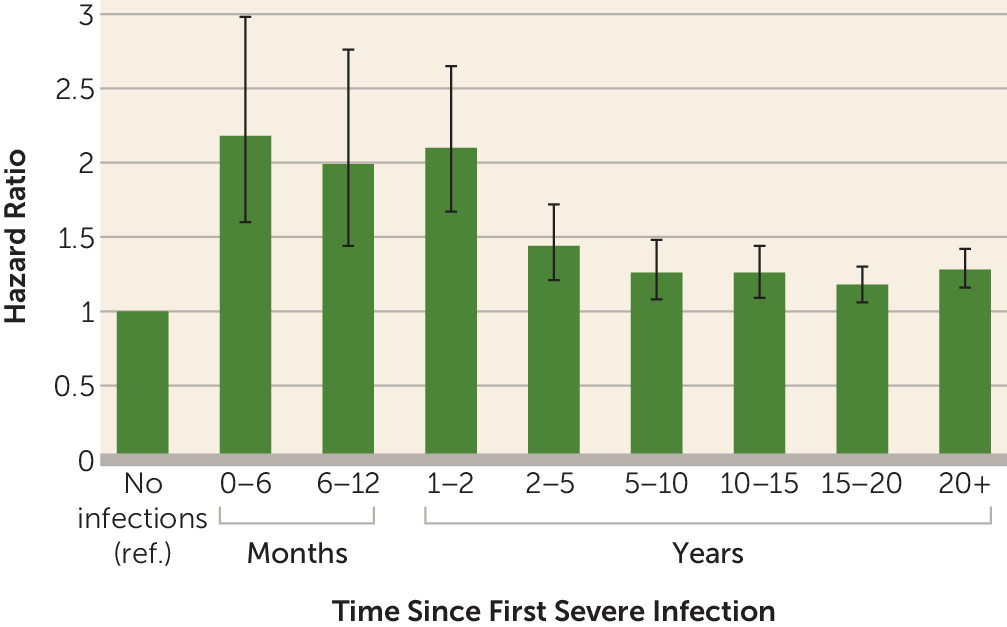
Infections as Predictors of Conversion From Substance-Induced Psychosis to Schizophrenia
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Infection and Timing Relative to SIP | Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p |
| Any infection prior to SIP | 0.95 | 0.83–1.09 | 0.48 | 0.96 | 0.83–1.10 | 0.55 | |||
| Any infection after SIP | 0.88 | 0.66–1.16 | 0.36 | 0.88 | 0.66–1.17 | 0.38 | 0.88 | 0.66–1.18 | 0.40 |
| Hepatitis after SIP | 1.89 | 1.09–3.30 | 0.02 | 1.89 | 1.09–3.30 | 0.02 | 1.87 | 1.07–3.26 | 0.03 |
| Sepsis after SIP | 0.74 | 0.19–5.24 | 0.76 | 0.74 | 0.10–5.30 | 0.77 | 0.66 | 0.09–4.70 | 0.68 |
| Gastrointestinal infection after SIP | 1.10 | 0.60–2.01 | 0.76 | 1.11 | 0.61–2.03 | 0.73 | 1.14 | 0.62–2.08 | 0.67 |
| Skin infection after SIP | 0.93 | 0.60–1.44 | 0.74 | 0.93 | 0.60–1.45 | 0.75 | 0.94 | 0.60–1.46 | 0.78 |
| Respiratory infection after SIP | 0.72 | 0.37–1.39 | 0.32 | 0.72 | 0.37–1.39 | 0.33 | 0.72 | 0.37–1.41 | 0.34 |
| Urogenital infection after SIP | 0.67 | 0.25–1.80 | 0.43 | 0.67 | 0.25–1.81 | 0.43 | 0.67 | 0.25–1.81 | 0.43 |
| CNS infection after SIP | Inestimable | Inestimable | Inestimable | ||||||
| Other infections after SIP | 0.92 | 0.52–1.64 | 0.77 | 0.93 | 0.52–1.65 | 0.79 | 0.94 | 0.53–1.68 | 0.85 |
Discussion
The Association Between Infections and Substance-Induced Psychosis
The Association Between Infections and Specific Types of Substance-Induced Psychosis
The Association Between Infections and Conversion From Substance-Induced Psychosis to Schizophrenia
Implications
Strengths and Limitations
Conclusions
Supplementary Material
- View/Download
- 172.41 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).