We need better treatments for all of our patients, especially for those with schizophrenia. The only plausible path toward developing fundamentally new treatments for psychiatric illnesses is to continue in the pursuit of understanding their underlying neurobiology. These investigations need to be focused on developing a mechanistic understanding of the factors driving the diverse phenotypic presentations, symptoms, and developmental time courses of the illnesses that we treat. A first step is to identify and characterize the function of the neural circuits that underlie normal cognitive, emotional, and behavioral functioning and, from this perspective, to understand the alterations in these circuits that play an etiological or pathophysiological role in mediating psychiatric illnesses. Because most psychiatric illnesses, or the disposition to develop them, have fetal or early-life origins, a critical issue is to understand the factors that affect the normative development of relevant neural circuits. Genetic and epigenetic influences are at play here, as the genetic programs that provide the blueprint for neural circuit development are environmentally modifiable via such mechanisms as DNA methylation and chromatin remodeling, which can influence gene expression. Neurotransmitters, neurotrophic factors, receptors, and intracellular signaling molecules are key as they not only mediate neural transmission and communication but also are involved in guiding the development of neural pathways and circuits. It is also essential to understand mechanisms underlying neuroplasticity, which in response to later-life stressors, or at critical developmental transitions such as adolescence, can promote adaptive or maladaptive neural modifications in illness-related neural circuits. Understanding mechanisms underlying neuroplasticity may also be key in developing treatment strategies focused on repairing affected neural pathways or on enhancing pathways that could help compensate for other deficits.
Although schizophrenia is commonly diagnosed in late adolescence and early adulthood, it is an illness with clear neurodevelopmental origins. The profound effects of this illness on perception, cognition, emotion, and behavior reflect the brain-wide alterations that have been well documented with genetic, molecular, and neuroimaging approaches. While many of these findings indicate an association between a specific biological process and schizophrenia, it is important to realize that data demonstrating associations do not provide evidence for causal involvement in mediating the illness. Such findings could reflect other factors associated with having the illness, like illness chronicity or long-term medication exposure. Animal model work, as well as in vitro studies, such as those using neurons derived from stem cells of patients with schizophrenia, are a critical component of the research efforts, which can directly test causal hypotheses generated from human studies.
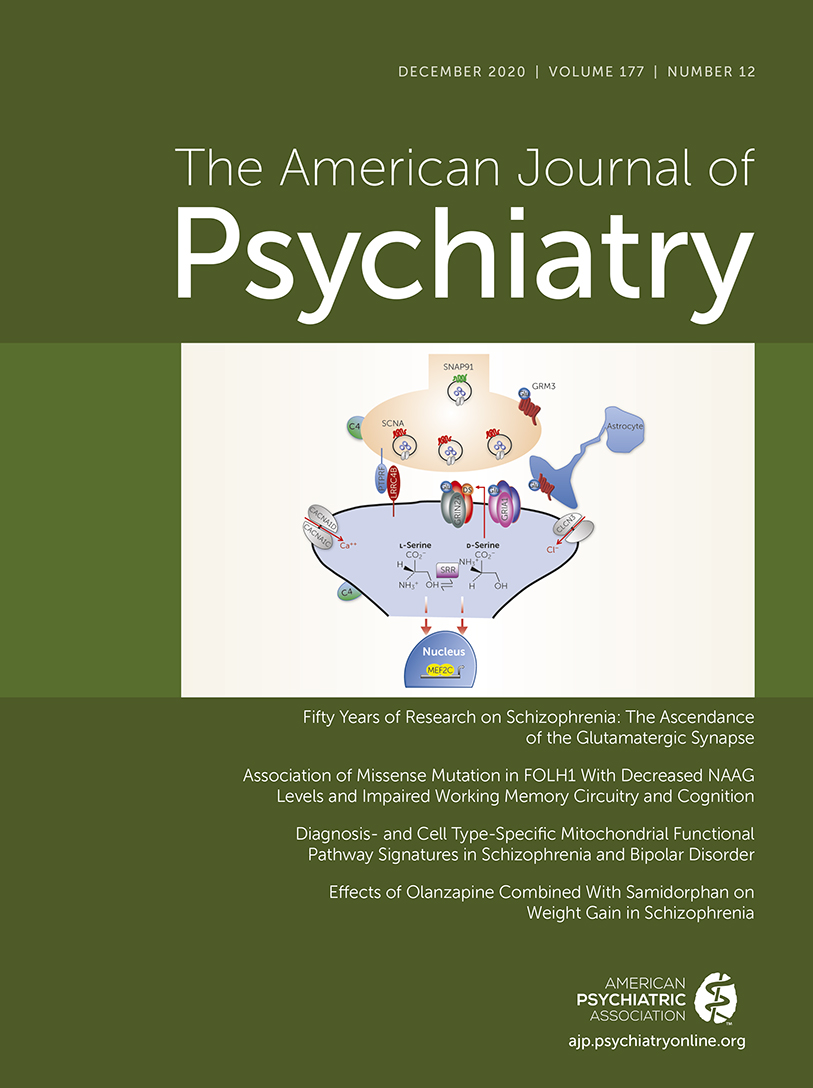
This issue of the
Journal is dedicated to presenting scientific advances that are related to deepening the understanding of the etiological and pathophysiological mechanisms relevant to schizophrenia. Ultimately, these lines of research have the potential to inform the development of novel and improved treatment strategies. The centerpiece of this issue is an overview by Dr. Joseph Coyle and Dr. Brad Ruzicka (
1) that presents a historical perspective on schizophrenia research that is followed by an update on evidence supporting the critical role of glutamatergic neurons and
N-methyl-
d-aspartate (NMDA) receptors in the pathogenesis of schizophrenia. Dr. Coyle, from McLean Hospital and Harvard Medical School, is a distinguished leader in the field who has dedicated his career to psychiatric research specifically focusing on glutamatergic mechanisms relevant to the neurobiology of schizophrenia. As he has made fundamental discoveries at the molecular level and has attempted to translate these findings to new treatments, his work exemplifies the importance of having both a deep understanding of the illnesses that we treat as well as the critical scientific knowledge necessary to pursue important translational research questions.
Insights Into Genetic Variation Mediating Alterations in Glutamatergic Function and Impaired Working Memory
By using a combination of molecular and imaging methods in tissue from postmortem brains and in clinical studies, Zink and colleagues (
2) provide compelling evidence in humans that increased levels of the neurotransmitter
N-acetyl-aspartyl-glutamate (NAAG) are associated with better cognition. NAAG is a neurotransmitter that acts as an agonist of the metabotropic glutamate receptor 3 (mGluR3) and as an antagonist of the NMDA receptor. The authors studied individuals with a missense mutation in the folate hydrolase gene (FOLH1) that regulates the amount of synaptic NAAG. The product of FOLH1 is glutamate carboxypeptidase II (GCPII), which functions to break down NAAG into
N-acetlyaspartate and glutamate. Findings from the postmortem studies demonstrated that a mutation in the FOLH1 gene resulted in an increase in its expression in the dorsolateral prefrontal cortex (DLPFC). In the clinical studies, this mutation was also associated with decreased NAAG levels, decreases in visual memory performance, and lower IQ. These findings were present across both healthy subjects and patients with schizophrenia and did not differ between the groups. The FOLH1 mutation was also associated with less efficient cortical activation during a working memory task. Although schizophrenia is an illness that is associated with cognitive impairments, especially in working memory, the findings from this study suggest that this pathway may be a viable target for enhancing memory and other cognitive functions across diagnostic categories. In an editorial, Dr. Amy Arnsten, a neuroscientist and professor at Yale University, provides along with her colleague Min Wang a highly informative overview focused on the functioning and relevance of the mGluR3-NAAG-GCPII pathway in relation to memory and schizophrenia and as a potential treatment target (
3). In this editorial, they importantly point out the differences between rodents and primates in the neuroanatomical localization of mGluR3 and assert that with evolution the function of the mGluR3-NAAG-GCPII pathway has changed.
Mitochondrial Alterations in Schizophrenia and Bipolar Disorder
Mitochondria are considered the powerhouse of the cell, primarily functioning to generate ATP as an energy source. Numerous diseases have been associated with mitochondrial dysfunction, and it has been suggested that altered mitochondrial function may, in part, underlie altered neurotransmission in illnesses such as schizophrenia and bipolar disorder. Glausier et al. (
4) explore this possibility by analyzing data from publicly available RNA sequencing databases focusing on characterizing mitochondrial-related gene expression in DLPFC tissue and more specifically in layer 3 and layer 5 pyramidal neurons from the DLPFC. As in the study by Zink et al. (
2), the authors opted to examine DLPFC tissue because of the involvement of this region in the impaired cognitive function that occurs in schizophrenia. Overall, the DLPFC tissue and pyramidal neuron findings provided evidence for greater mitochondrial gene involvement in schizophrenia. In sum, 41% of mitochondrial-related genes were differentially expressed in the DLPFC of schizophrenia brains compared with 8% in brains from patients with bipolar disorder. In the patients with schizophrenia, many of these genes were related to energy production. To assess the possibility that this finding could be due to long-term antipsychotic exposure and not the illness itself, the authors performed experiments in monkeys that were administered clozapine, haloperidol, or olanzapine. In general, the long-term administration of these drugs did not significantly affect mitochondrial-related gene expression in the DLPFC or in layer 3 and 5 pyramidal neurons. The addition of this translational nonhuman primate study is an important complement to the human study as it allows for testing a causal hypothesis that informs the interpretation of the human data. Dr. Yogesh Dwivedi from the University of Alabama at Birmingham discusses in depth the evidence implicating mitochondrial dysfunction in schizophrenia and bipolar disorder, the analytic strategies used in the present study, and the implications of the findings (
5).
Neural Circuit Function Related to Delusions and the Genetic Risk for Schizophrenia
Greenman et al. (
6) use a creative approach to study patients with schizophrenia and healthy control subjects to understand how neural circuits that are associated with updating working memory are related to delusions and polygenic risk scores (PRSs) for schizophrenia. One way to think of the processes underlying delusions is that false beliefs can be sustained by a failure to update working memory when new, relevant information is available. It is argued that this could account for the fixed and inaccurate beliefs of individuals with delusions. In this article, using functional MRI and dynamic causal modeling, the authors first demonstrate that the process of updating working memory is related to feedforward connectivity between parietal regions and the DLPFC. They then show reduced effective connectivity between these regions in patients with schizophrenia and that it is related to the presence of delusions. Furthermore, in control subjects, the authors found that individual PRSs for schizophrenia were related to reduced connectivity between parietal and prefrontal regions when updating working memory. Finally, using imaging data from healthy subjects performing a memory task and a memory updating task, the authors developed a machine learning model that, when applied to the imaging data of schizophrenia patients, was able to predict the severity of delusions. This article uses a multifaceted and imaginative approach by combining a memory updating neuroimaging task with PRSs and machine learning in both healthy subjects and individuals with schizophrenia. It serves as an exemplar of how complex methods and large data sets can be integrated to understand mechanisms underlying symptoms and suggests the possibility of a circuit-based individualized treatment approach for delusions. Dr. Karl Friston, scientific director of the Wellcome Centre for Human Neuroimaging and professor at University College London, comments on the importance of the findings in an editorial (
7) where he brings together empirical data and theory with a discussion from the perspective of the “Bayesian brain.” (The Bayes theorem describes how using and updating germane information related to an event can be used to predict the future likelihood of its occurrence.)
Decreased Volumes of Specific Thalamic Nuclei in Psychotic Disorders
The thalamus has long been implicated in the pathophysiology of schizophrenia, and previous studies have demonstrated reduced thalamic volumes in patients with psychotic disorders. Huang and colleagues (
8) report on findings from a thorough study using a sophisticated method to assess thalamic nuclear volumes in a large sample of adults (293 individuals with psychosis, including psychotic bipolar disorder, and 179 healthy individuals) and youths (398 youths with psychosis spectrum symptoms, 609 youths with other psychopathology, and 386 typically developing youths). The data demonstrate that both patients with psychotic disorders and youths at risk for these disorders have reduced volumes in specific thalamic association nuclei, including the pulvinar and the mediodorsal nucleus. The pulvinar is part of the visual attention network, and the medial dorsal nucleus is highly interconnected with the amygdala and prefrontal cortex. The authors also found that individual differences in pulvinar volumes were predictive of general cognitive function. The data used from at-risk youths with psychosis spectrum symptoms are an important addition to the study and were obtained from the Philadelphia Neurodevelopmental Cohort. In their analysis, the authors compared youths with psychosis spectrum symptoms with typically developing youths and with youths with other psychopathology and found that thalamic nuclear volume reductions were selectively observed in youths with psychotic spectrum symptoms. This points to the specificity of this finding and, importantly, demonstrates pathological involvement of the thalamus prior to illness onset.
Further Evidence Supporting Opiate Antagonism in Reducing Antipsychotic-Induced Weight Gain
Building on previous work (
9), Correll et al. (
10) present data from a phase 3 clinical trial assessing the effects of a combined preparation of olanzapine and samidorphan compared with olanzapine alone on weight gain in patients with schizophrenia. Among its other effects on the opiate system, samidorphan is a μ-opiate receptor antagonist, and considerable preclinical and clinical data point to its capacity to mitigate olanzapine-related weight gain. The present study assesses the effects of samidorphan over a period of 24 weeks, which is important as antipsychotics are typically used over prolonged periods of time. Over the course of the study, significantly fewer patients taking the olanzapine/samidorphan combination, compared with those taking olanzapine alone, gained greater than 10% of their body weight, and the combination treatment was also associated with significantly reduced increases in waist circumference. The effects on reducing weight gain were not apparent until 6 weeks of treatment and, consistent with earlier data, the addition of samidorphan did not influence the efficacy of olanzapine. Importantly, while the olanzapine/samidorphan combination affected weight gain and waist circumference, it was without significant effect on metabolic parameters (i.e., measurements of cholesterol, triglycerides, glucose, insulin, and hemoglobin A
1c) that are frequently increased in association with olanzapine and other antipsychotic use. In an editorial (
11), Dr. Robert Buchanan from the University of Maryland School of Medicine focuses on the meaningfulness of these findings in relation to the lack of samidorphan’s effects on metabolic parameters and discusses other strategies for reducing antipsychotic-induced weight gain, including using antipsychotics that appear to have less potential for weight gain and metabolic alterations.
Conclusions
This issue of the Journal presents papers that represent the sophisticated efforts of researchers dedicated to improving the lives of patients with schizophrenia and other psychotic disorders. The methods used are complex and reflect state-of-the-art genetic, neuroimaging, and machine learning approaches. Exciting findings include: implication of brain NAAG levels in cognition, a finding particularly relevant to schizophrenia; altered prefrontal expression of genes that regulate mitochondrial function in schizophrenia; decreased connectivity between parietal and prefrontal regions associated with delusions, and the capacity to use such data to predict symptom severity; evidence for involvement of thalamic nuclei (i.e., pulvinar and medial dorsal nucleus) in youths at risk for developing psychotic disorders; and further support for the strategy of using opiate antagonism as a means to reduce olanzapine-induced weight gain.
Science is complicated and methodical, and although it may seem distant from the pragmatic needs of providers, it is important for clinicians to value the work and understand the concepts. The main findings of the articles presented in this issue provide evidence to support the targeting of specific genes, molecules, and neural circuits in the pursuit of new treatments that will improve the lives of patients with schizophrenia.