The article by Zhan et al. (
1) in this issue of the
Journal is an inspiring example of innovative trans-species neuroscience with potential transdiagnostic clinical relevance. The aim of their study was to use the brain network characteristics of a monkey model for autism as classifiers in their machine-learning framework to differentiate between human cases of autism spectrum disorder (ASD) and control subjects and to translate this even further to other neurodevelopmental disorders such as obsessive-compulsive disorder (OCD).
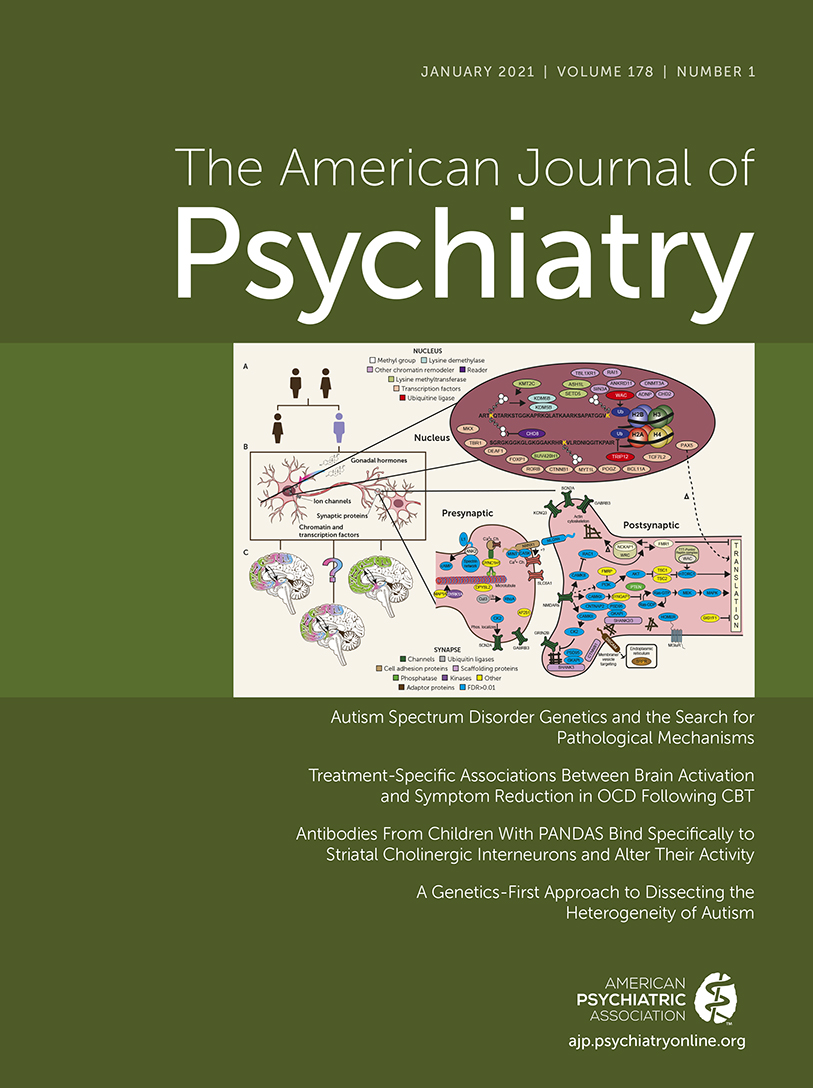
The basis of their work lies in the idea that methyl-CpG binding protein 2 (MECP2), expressed by the MECP2 gene on the X-chromosome, is important for optimal brain maturation by its supportive role in the formation of synaptic contacts. In clinical practice, MECP2 gene mutations are best known as the cause of Rett syndrome, a progressive neurological developmental disorder and one of the most common causes of cognitive disability in girls (
2). Some clinical characteristics of Rett syndrome and other MECP2-related neurodevelopmental disorders resemble the cognitive, emotional, and behavioral symptoms of autism: intellectual disability, motor dysfunction, social behavioral deficits, and anxiety (
3).
The first MECP2 duplication transgenic monkeys, studied at late infant and early juvenile developmental stages, appeared to show similar behavioral deficits as those found in MECP2-related human case subjects: the animals were less socially active and showed increased stereotyped motor behavior (
4). Overexpression of MECP2 also resulted in coexpression of genes related to the GABA-ergic system, affecting brain network function, as shown 2–3 years after the initial experiment when the same monkeys were remeasured using EEG (
5). The altered excitation-inhibition balance in the transgenic monkeys, compared with the wild-type, led to altered beta-synchronization in fronto-parieto-occipital circuits, which was associated with the increased repetitive locomotor behavior in the transgenic animals.
The high similarity between the human and nonhuman primate brain network architecture opens the way to use transgenic monkey-derived network features to support diagnostics in humans. That is why Zhan et al. measured these same 11 wild-type and five MECP2 duplication transgenic monkeys using MRI. Using the nine core regions that differed between wild-type and MECP2 duplication transgenic monkeys as seeds, they constructed monkey-derived classifiers consisting of the functional connections of the human functional connectome, using two open-access ASD cohorts, an open-access attention deficit hyperactivity disorder (ADHD) cohort, and one local OCD cohort. The same set of monkey-derived core regions that informed diagnostic classification in human autism with 75%−82% accuracy was also useful for diagnostic classification in the OCD cohort (78% accuracy) but not the ADHD cohort. Connectivity between the right ventrolateral prefrontal cortex and the left thalamus and the right prefrontal polar cortex predicted communication disabilities in the ASD sample and severity of compulsivity in the OCD sample, respectively.
Insight into how specific genes, such as MECP2, are linked to the behavioral level (repetitive movements and decreased social behavior) and to the neural circuit level (altered network architecture) paves the way to innovative treatment discoveries.
The first example of how this field of research translates to the clinic follows the knowledge that MECP2 overexpression affects the GABA-ergic system. The efficacy of GABA-ergic inhibition is dependent on intracellular neuronal chloride. High levels of chloride (common in immature neurons) are related to excitatory effects of GABA. With maturation, chloride levels reduce, and GABA mainly supports inhibition. The normal GABA shift during delivery, stimulated by the abrupt neuroprotective oxytocin-mediated hyperpolarizing GABA action in the pyramidal neurons, is altered in animal models of ASD (
6). In a recent study using mutated mice, the MECP2-related abolition of the GABA shift could be restored by maternal administration of the specific NKCCI chloride-importer antagonist bumetanide just before delivery (
7). By restoring the chloride homeostasis, bumetanide normalizes the GABA-ergic inhibition. Recent randomized controlled studies on the therapeutic potential of bumetanide in children and adolescents with ASD showed a significant effect on the severity of ASD-related symptoms (
8,
9). Also, clinical improvement was associated with a reduction in the GABA/glutamate ratio in the occipital and insular cortex, as measured with magnetic resonance spectroscopy (
10). Whether bumetanide will be of added value to other neurodevelopmental disorders characterized by an excitation-inhibition imbalance will be a question for future studies.
The second example is the use of genome engineering approaches, using the Nobel Chemistry Prize 2020 winning technology CRISPR-Cas9, developed by Emmanuelle Charpentier and Jennifer Doudna. Components of ancient immune systems from bacteria are used as “gene scissors” to restore DNA overexpression (
11). Using this gene scissors approach, Yu et al. (
12) recently showed in MECP2 duplication mice that normalization of MECP2 levels in the medial prefrontal cortex using CRISPR-Cas9 reversed the social recognition deficit in the transgenic animals. It would be relevant to see whether this genome engineering technology can also improve social behavior and decrease stereotyped motor behavior in the transgenic nonhuman primates and, if so, whether this is accompanied by normalized network architecture. Further translation toward gene therapy in humans may be relevant for cases with Rett and MECP2 duplication syndrome and may also open new avenues for innovative treatments for ASD and other neurodevelopmental disorders.
Although very appealing, the relationship between MECP2 and ASD and other neurodevelopmental disorders is mostly unknown. Only a minor subset of patients with ASD show rare copy number variants in MECP2, and the link between MECP2 and OCD has not been described so far. Also, the clinical phenotype of MECP2-related neurodevelopmental disorders such as Rett is not limited to the characteristic autism-like deficits in social behavior and motor stereotypies. We can thus wonder whether MECP2 is the link underlying the abnormal network architecture in the transgenic monkeys of Zhan et al. and human cases with ASD and OCD, or instead a nonspecific phenomenon of altered neurodevelopment.
Psychiatrists do not need an MRI scan to differentiate between health and psychopathology, but the differentiation between, for instance, ASD and OCD can be hard in some cases, mainly when the repetitive ritualistic behaviors that are characteristic of both disorders form the core symptoms of impairment. Brain-based diagnostic tools are warranted in these circumstances. However, in cases where the network abnormalities in the transgenic monkeys and the human cases with ASD and OCD represent a nonspecific marker of altered neurodevelopment, the machine-learning framework will not be of added value in the differentiation between these related and often comorbid neurodevelopmental disorders.
Based on more than three decades of brain imaging studies, we know that the dysfunctions in the neural circuits implicated in emotional appraisal, cognitive control, behavioral inhibition, and sensorimotor processing are present in many mental disorders and not specific to one disorder. The OCD, ADHD, and ASD working groups of the Enhancing Neuroimaging and Genetics by Meta-Analysis (ENIGMA) consortium recently performed the largest transdiagnostic study on the overlap and specificity of structural brain markers, involving 12,198 individuals of 151 cohorts worldwide (
13). No shared differences were found among the three disorders, compared with control subjects, which fits with the low predictive value of the monkey network-based classifiers to detect ADHD cases. The only detected overlap between patients with OCD and ASD in the ENIGMA analysis was found in adults to be decreased volume of the hippocampus, a structure that is not typically associated with impaired behavioral inhibition, the key transdiagnostic trait within the impulsive-compulsive spectrum. It can be expected that resting-state functional MRI (fMRI) (as used by Zhan et al.), EEG- or magnetic resonance spectroscopy-based measures of excitation-inhibition ratio, and task-based fMRI using paradigms that test core cognitive, emotional, and behavioral dysfunctions underlying shared and disease-specific symptoms, will give more sensitive and specific biomarkers of disease that can also be used to predict and monitor the response to innovative therapies.