This issue of the
Journal brings together interesting papers that shed light on the genetics and mechanisms underlying obsessive-compulsive disorder (OCD) and autism spectrum disorder (ASD). Although these illnesses are very different, their symptoms can be comorbid, and both illnesses are associated with lifelong suffering and disability. OCD is estimated to be approximately 40% heritable, with a mean age at onset of 19 years and an estimated lifetime prevalence of 2.3% (
1–
3). Interestingly, males have an earlier age at onset, with 25% of male cases emerging before 10 years of age, and earlier onset appears to be more heritable. Up to 50% of OCD cases are associated with serious impairment, with 90% of OCD patients having other comorbid psychiatric disorders—the most common being anxiety, depression, and impulse control disorders (
1,
2). Serotonin reuptake inhibitors and cognitive-behavioral therapy (CBT) with exposure and response prevention are the mainstays of treatment. However, the symptoms of a large proportion of patients with OCD fail to adequately respond to treatment, and these patients continue to suffer from significant and very impairing symptoms. In the most severe refractory cases, deep brain stimulation aimed at modulating components of the putative OCD circuit has shown promise in symptom reduction. In this issue of the
Journal, Drs. Wayne Goodman, Eric Storch, and Sameer Sheth from Baylor College of Medicine contribute an excellent overview on OCD that comprehensively integrates recent thinking regarding mechanisms underlying OCD as they relate to current and new treatment development (
4).
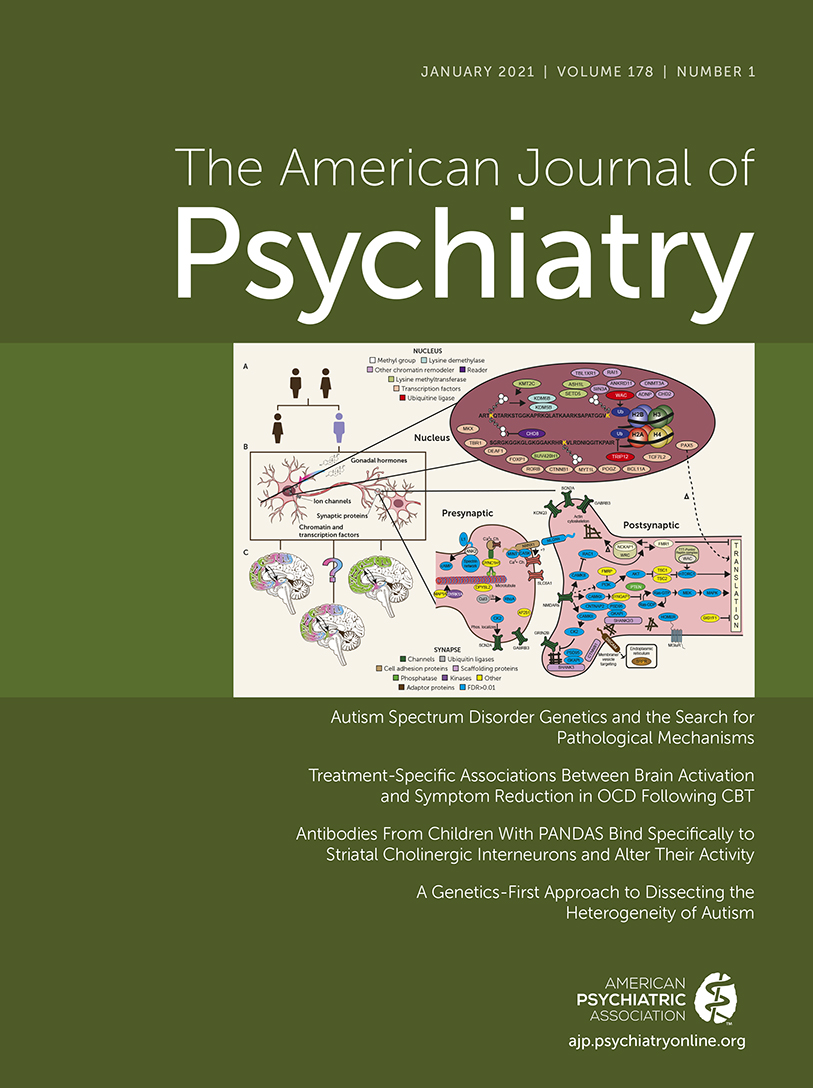
ASD is a pervasive neurodevelopmental disorder that can be diagnosed in young children and is characterized by marked deficits in social interactions, communication, and behavior. ASD is very heterogeneous in its presentation, which likely reflects different genetically driven alterations in neurodevelopmental pathways. It is estimated that approximately 33% of individuals with ASD also have an intellectual disability (IQ <70). The overall prevalence of ASD is around 2%, with a marked prevalence in boys (3%) compared with girls (0.7%) (
5). ASD is frequently associated with other comorbid psychiatric symptoms, including anxiety and OCD-like symptoms. Although ASD is heritable, and the estimates of its heritability vary, considerable recent progress has identified genetic variation that is associated with the risk to develop ASD. In this issue of the
Journal, Drs. Matthew State and Devanand Manoli provide an outstanding overview on the genetics of ASD (
6). Of particular interest is the discussion focused on how alterations in molecular systems occurring during neonatal development likely contribute to the risk to develop ASD and mediate its pathophysiology. It is the hope that future insights gained from such a genetic-neurodevelopmental approach will provide ideas about how to conceptualize, develop, and test new early-life treatments for children with ASD.
Neural Predictors of CBT Efficacy in Patients With OCD
Norman et al. (
7) report findings in patients with OCD demonstrating the possibility of using pretreatment neuroimaging measures, including exposure-response prevention, to predict the likelihood of response to CBT. As Goodman et al. discuss in their overview, cingulo-opercular, orbitostriatal, and amygdalar regions have been implicated in the pathophysiology of OCD. Important aspects of this study design include the inclusion of adolescents and the comparison of CBT with an “active control therapy,” stress management therapy (SMT). From the 87 patients who participated in the study, somewhat surprisingly, both treatments resulted in symptom reduction with no significant between-group difference in the magnitude of response. However, the rate of improvement was greater with CBT treatment. In the CBT group, when assessed prior to treatment, cognitive control–related activation of the right temporal lobe and rostral anterior cingulate predicted treatment response, whereas during reward processing, activation in regions of the prefrontal cortex and amygdala predicted CBT response. These findings also did not differ by age as they were present in both the adolescent and adult patients. In general, these findings are consistent with the idea that better treatment outcomes are associated with the relative preservation of the function of neural circuits that are impaired in an illness and that are frequently involved in cognitive and emotional processing. Interestingly, treatment response in the SMT group was generally associated with reduced activation in the same regions in which increased activation predicted CBT response. Why this is the case is unclear. Although the sample size in this study was modest, the study supports the possibility of using pretreatment imaging measures in patients with OCD to predict treatment response and to select a psychotherapeutic intervention that is most likely to be successful.
Molecular Mechanisms Associated With PANDAS
The abrupt onset of OCD symptoms in some children has been suggested to be due to an innate immune response to a recent streptococcal infection, frequently group A beta-hemolytic
Streptococcus. In addition to OCD-like symptoms, children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) often exhibit choreiform movements. Also, individuals with Sydenham’s chorea, an illness associated with rheumatic fever and group A beta-hemolytic streptococcal infection, frequently have OCD symptoms. Based on this and other observations, it has been suggested that an autoimmune response targeted at basal ganglia neurons may underlie the symptoms observed in children with PANDAS. Further support for the autoimmune nature of PANDAS is provided by the demonstration of increased serum antibodies to various neuronal targets and by the fact that some patients’ symptoms respond to immune modulatory therapy, such as intravenous immunoglobulin (Ig) administration. Xu and colleagues (
8) collected Ig antibodies from the serum of 27 children with PANDAS before and after intravenous Ig treatment. In the laboratory, the investigators studied the effects of these antibodies on mouse brain slices. The findings demonstrated that the IgG from children with PANDAS selectively bound to striatal cholinergic interneurons, and this finding was confirmed using sections of human brain. Furthermore, the presence of these antibodies was associated with a reduction in the activity of striatal cholinergic interneurons but not specific types of GABAergic interneurons. The investigators also found that the reduction in IgG binding to striatal cholinergic interneurons after treatment correlated with individual treatment responses. These cross-species translational data are potentially exciting and serve to focus the search for the pathophysiology of PANDAS toward a specific class of interneurons within the striatum that are known to fine tune and regulate striatal output via their influences on the abundant medium spiny GABAergic neurons that project to effector sites. Because of the similarities between PANDAS and bona fide OCD, these studies raise the possibility that striatal cholinergic interneurons are mechanistically involved in the pathophysiology of childhood OCD. In his editorial (
9), Dr. Steve Hyman from Harvard University critically appraises this study and suggests that, in addition to the mechanism suggested by the findings in this article, other immune-related molecular pathways may also be important.
Combining Imaging Data From a Primate Genetic Model of Autism With Human Data to Inform ASD and OCD
Zhan et al. (
10) creatively use resting-state functional MRI data collected from monkeys that were genetically engineered to overexpress the methyl-CpG binding protein 2 (
MECP2) to inform human imaging data and diagnoses. By using machine learning techniques with the monkey imaging data along with imaging data from humans with OCD, ASD, and attention deficit hyperactivity disorder (ADHD), the investigators developed a highly accurate neuroimaging-based classifier for autism. They also found that this cross-species, machine learning–derived classifier predicted compulsivity scores in OCD patients but was not helpful in distinguishing individuals with ADHD. Key brain regions found to be involved included frontal and temporal regions. Previous groundbreaking work in the monkeys used in this study demonstrated the ability to develop a transgenic model in a primate species by specifically overexpressing
MECP2, a gene that is associated with Rett syndrome, a rare and severely impairing developmental disorder. Importantly, the monkeys with this genetic alteration exhibited abnormal behaviors and impaired social interactions similar to those observed in ASD individuals (
11). Thus, by using data from this causal primate model, the authors demonstrate neural circuit alterations that are attributable to the developmental consequences of altering a specific gene and relate this to imaging data in patients with ASD. In addition, the findings shed light onto the comorbidity, and at times the similarities in symptoms, between ASD and OCD. More generally, these findings suggest that further efforts integrating databases from nonhuman primates and humans may be very helpful in developing diagnostic and treatment approaches for human neurodevelopmental and psychiatric disorders. In her editorial, Dr. Odile van den Heuvel from the University of Amsterdam explains the findings in depth, offers plausible mechanisms by which
MECP2 may affect neurodevelopment, and places in context the suggested role of
MECP2 as being mechanistically involved in ASD (
12).
Developments in Understanding the Genetics Underlying Autism and Its Heterogeneity
In their overview focused on the genetics of autism, State and Manoli review the current understanding of the complex genetic alterations that are associated with ASD and address how understanding these genetic alterations can help conceptualize and guide new treatment development. Also in this issue, Dr. Elisabeth Binder, from the Max-Planck Institute in Munich, contributes an editorial focused on how to think about genotype-phenotype associations in ASD (
13), commenting on the implications of two articles in this issue that address genetic alterations in relation to the heterogeneity of ASD.
The first article, by Chawner et al. (
14), examined the extent to which heterogeneity in the presentation and symptoms of autism can be accounted for by different rare copy number variants (CNVs) that are known to increase the risk for autism. The investigators began with a sample of individuals, not selected for ASD, all known to have rare CNVs that are associated with a high risk of autism. These were either deletions or duplications of the same chromosomal region, 16p11.2 or 22q11.2. In this sample, the authors found an increased incidence of autism ranging from 23% to 53% depending on the CNV. They also found that autism severity and symptom profiles significantly differed between CNV groups. However, the strength of the gene-to-phenotype prediction was weak, and notably the phenotypic variation related to a specific CNV was greater than that observed between groups with the different CNVs. Of note, 54% of the individuals in this sample who did not meet full criteria for ASD had traits of autism. Unique aspects of this study include a large sample with specific rare CNVs and the “genetics first” approach that was used to define genotype-autism phenotype relations. Overall, the findings suggest that while very informative in relation to autism risk, the CNVs explored in this study are not particularly helpful in predicting the heterogeneity in symptoms that are present across individuals with ASD.
In the second article, by Douard et al. (
15), the authors characterized all CNVs across the genome in two autism and two reference populations and then developed models to test the association between the genes associated with the CNVs and different phenotypic features of autism, including IQ. In general, the authors found that individuals who had greater numbers of CNVs that were associated with loss of function of a gene were more likely to have an increased risk for autism and a decreased nonverbal IQ. The findings suggest that CNVs characterized by deletions are more likely than those associated with duplications to be associated with reduced IQ. The data also suggested that CNV duplications were associated with other phenotypic components of autism, such as deficits in motor skills. These findings demonstrate that regardless of where the CNV is or which genes are affected, the more CNVs an individual has, the more severe the disability and risk to develop autism. In her editorial, Dr. Binder discusses the implications of these findings as well as those relative to genotype-phenotype predictions in autism and, more practically, in relation to how these data may inform genetic screening approaches.
Conclusions
This issue of the Journal is focused on the neural circuits and genetics relevant to OCD and ASD, two illnesses that contribute to considerable individual suffering and family burden. It is noteworthy that two of the articles in this issue use cross-species translational approaches to bring together data from preclinical animal studies with data from human studies to investigate questions of causality. Take-home points from the findings reported include: the possibility of using functional neuroimaging to predict response to CBT, incorporating exposure and response prevention in adolescents and adults with OCD; new ideas about mechanisms involving striatal cholinergic interneurons in underlying acute, poststreptococcal infection–related onset of OCD symptoms in children; insights from studies using genetically engineered nonhuman primates that shed light on how alterations in the MECP2 gene may relate to functional brain changes associated with ASD and OCD; and understanding how specific CNVs, and the total number of CNVs across an individual’s genome, relate to symptom presentation and severity in ASD.
The research presented in this issue is emblematic of the complexity of current approaches and methods used by scientists in our field to better understand the pathophysiological mechanisms underlying the illnesses that we treat. These strategies allow for analyses linking phenotype to neural circuits, to specific cell types within a brain region, and to genomics. The overviews on OCD and the genetics of ASD, along with the editorials in this issue, provide a foundation and framework for understanding the complexity of these areas and the potential clinical relevance of the findings. It is my hope that the papers in this issue provide our readership with an appreciation for the sophisticated scientific efforts that are necessary for unraveling the pathophysiological processes underlying ASD and OCD, as well as an understanding of how the data presented in these papers are steps toward better diagnosis and treatment selection and the development of novel early-life treatments.