Alcohol use disorder (AUD) afflicts approximately 14,500,000 Americans (
1). Alcohol misuse is the primary reason given for 1,714,757 emergency department visits and 88,000 deaths in the United States annually (
2). These morbidity and mortality metrics far exceed those for any illicit substance of abuse, with 90% of completed suicides involving a psychiatric disorder (primarily depression) and/or substance use disorder (primarily AUD). A white paper report on suicide suggested that such concurrent disorders should be expected and treated simultaneously (
3). Left untreated, AUD can impede the accurate diagnosis and successful treatment of co-occurring psychiatric disorders. The goal of concurrent treatment may be undermined by the low utilization of medications approved by the U.S. Food and Drug Administration (FDA) for the treatment of AUD. Three medications are FDA approved for the treatment of AUD: disulfiram, naltrexone, and acamprosate. A nationwide pharmacy survey indicated that less than 4% of patients with AUD receive prescriptions for an FDA-approved medication to treat their disorder (
4). Meta-analyses of acamprosate and naltrexone show effect sizes that are equivalent to those reported in recent meta-analyses of controlled trials of antidepressants for major depressive episodes (
5 –
7). However, despite 5.3% of Americans meeting DSM-5 criteria for AUD, it has been many decades since a new compound has been introduced by the pharmaceutical industry to treat AUD.
The clinical trial by Sinha et al. reported in this issue (
8) seeks both to advance the repurposing of prazosin for the treatment of AUD and to identify a subgroup of patients likely to respond to prazosin treatment. Prazosin is a centrally and peripherally active alpha-1 adrenergic antagonist that was FDA approved for the treatment of hypertension in 1976 and is used off-label to treat anxiety, posttraumatic stress disorder, and trauma-related nightmares. Sinha et al. hypothesized that alcohol withdrawal symptoms would moderate prazosin effects on drinking outcomes over the course of a 12-week trial. One hundred community-recruited adults with AUD were randomly assigned to treatment with prazosin, titrated to 16 mg/day, or double-blind placebo. The Clinical Institute Withdrawal Assessment for Alcohol–Revised (CIWA-Ar) was used to evaluate the severity of withdrawal symptoms (
9). A significant interaction was observed between baseline CIWA-Ar score and drinking outcome, such that the subgroup of 44 patients who were treated with prazosin and had baseline CIWA-Ar scores ≥3 (mean=8.07, SD=5.44) showed a significant reduction in the percentage of drinking days and heavy drinking days during the study. In the subgroup of 56 patients who had baseline CIWA-Ar scores ≤2 (mean=0.86, SD=0.78), no advantage was observed with prazosin treatment (as illustrated in Figure S2 in the article’s online supplement). Importantly, among the subgroup with CIWA-Ar scores ≥3, those treated with prazosin also showed improvement in symptoms of depression, anxiety, and craving relative to those in the placebo group.
The DSM-5 criteria for alcohol withdrawal describe acute symptoms of autonomic nervous system activation that rarely exceed 5 days in duration. The CIWA-Ar was developed to measure the severity of these symptoms, with a cutoff score of ≥10 indicating clinically significant withdrawal that may require medical intervention. The Sinha et al. study used a cutoff score of 3 to define a “high” alcohol withdrawal subgroup responsive to treatment with prazosin. This cutoff score is well below the cutoff of 10 that has historically been used to identify patients at significant risk of alcohol withdrawal. However, anxiety was one of the three most common CIWA-Ar symptoms reported in this sample, and about half of the sample reported antecedent lifetime anxiety. These findings suggest that prazosin may yet join the growing number of treatments for the dark side of AUD. The “dark side of AUD” refers to the loss of brain reward function and gain of stress function that underlie symptoms of negative affect, such as anxiety, dysphoria, irritability, and insomnia, that persist beyond acute withdrawal into an indeterminate period designated as “protracted withdrawal” or “protracted abstinence.” Such symptoms of negative affect have more motivational significance for drinking relapse than the somatic symptoms of acute withdrawal captured by the CIWA-Ar. Pharmacotherapies to reverse the dark side of AUD offer new treatment opportunities for this pervasive and undertreated disorder (
10).
Academic researchers have sought to independently advance AUD treatment either by identifying subgroups of patients likely to respond to an AUD medication or by repurposing medications that are FDA approved for other indications. An example of the former is a pharmacometabolomic study conducted at the Mayo Clinic (
11) showing that high baseline serum glutamate levels predict response to acamprosate and revert to the normal range in patients who respond to acamprosate, thus identifying a subgroup of patients with AUD likely to show an optimum response to acamprosate treatment. Examples of medications successfully repurposed for the treatment of AUD include gabapentin and topiramate, both of which have been included in the APA “Practice Guideline for the Pharmacological Treatment of Patients With Alcohol Use Disorder” (
12).
An advantage of repurposing an old drug for a new indication of AUD is a known safety and tolerability profile. A disadvantage is the lack of a sponsor to fund the two positive multisite 6-month randomized controlled trials that are typically required for FDA approval of AUD as a new indication for an old drug. The availability of low-cost generic formulations provides no financial incentive to invest in FDA approval of AUD as a new indication. Consequently, the positive clinical trials of drugs repurposed for the treatment of AUD historically languished, with little impetus for clinical implementation. The APA guideline provides evidence-based recommendations that may facilitate appropriate prescribing of existing medications to treat AUD, and it also includes recommendations for prescribing two repurposed medications, gabapentin and topiramate, to treat AUD, based on an evaluation of the clinical trial literature generated by academic investigators. Including evidence-based repurposed medications in the APA guideline widens the available options for effectively treating AUD.
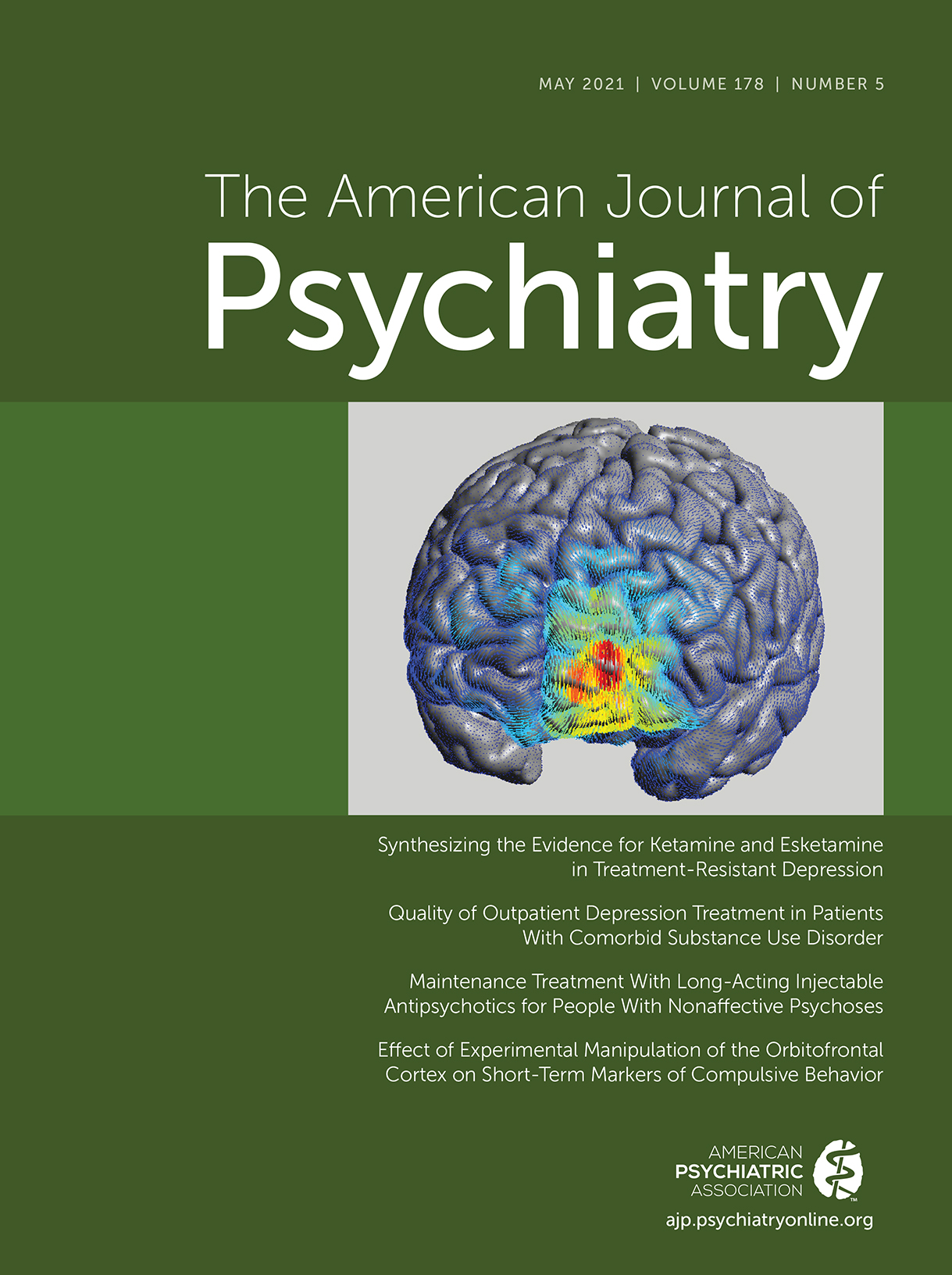
The original drugs to treat AUD, disulfiram and naltrexone, act by blocking the rewarding effects of drinking, but they do not treat the protracted withdrawal symptoms of negative affect, such as dysphoria, anxiety, irritability, and insomnia, that persist beyond acute withdrawal and heighten motivation for drinking relapse—symptoms that are collectively referred to as the dark side of addiction (
10). Conversely, many repurposed medications for AUD, such as gabapentin, act by restoring homeostasis in the brain’s stress response in the central nucleus of the extended amygdala that drives the protracted withdrawal symptoms encompassed by the dark side of AUD (
10,
13). Gabapentin was shown (
14) to significantly improve the two FDA-recommended outcomes of rate of complete abstinence and no heavy drinking (≥4 drinks/day for women, ≥5 drinks/day for men), and also to significantly reduce craving and alcohol-related disturbances in mood and sleep; results were dose dependent, with 1800 mg/day associated with optimal efficacy in 150 outpatients with AUD. Recent positive clinical studies of repurposed drugs that are hypothesized to act on the dark side of AUD include the glucocorticoid receptor antagonist mifepristone (
15), the vasopressin 1b antagonist ABT-436 (
16), and the nicotinic partial agonist varenicline (
17). Prazosin also fits into this category. Preclinical models of AUD showed that prazosin was effective in reducing both ethanol self-administration and anxiety-like behavior, particularly in animals that had relatively high levels of antecedent anxiety-like behavior (
18) or that were subjected to a stressor during alcohol deprivation (
19). Prazosin reduced cue- and stress-induced craving in human laboratory studies and showed mixed evidence of efficacy in clinical trials of patients with AUD, as summarized by Sinha et al. in their article. Altogether these older studies and the present study point to targeting the dark side of AUD as a viable approach to the development of much-needed medications to treat this devastating disorder.