Suicide-related behavior (SRB) is defined as any self-inflicted behavior for which there is explicit or implicit evidence of intent to kill or harm oneself, or that may or may not result in injury, including self-harm, self-inflicted unintentional death, suicide, and self-inflicted deaths or injuries of undetermined intent (
1). The term groups together fatal and nonfatal events, since even a nonfatal SRB event is a strong predictor of subsequent suicide (
2–
4). A systematic review (
5) found that within 12 months of a hospital presentation of SRB, 16% (95% CI=11–21) of people will have a repeat presentation and about 2% (95% CI=1.5–4.5) will die by suicide.
According to minority stress theory, first conceptualized by Meyer (
6), minorities (including sexual minorities) experience unique stressors and subsequent negative health outcomes as a result of conflicts with the dominant culture. Conflicts with heteronormative culture shape environments in which sexual minorities face unique stressors, including internalization of homophobic attitudes, expectations of rejection, and experiences of discrimination (
6,
7).
Research to date, relying on self-report data, has found that lesbian, gay, and bisexual individuals (LGB) are at higher risk of SRB events compared with their heterosexual counterparts (
8), which may be due to stigma and minority stress (i.e., culmination of excess stress uniquely attributable to being in a socially disadvantaged group). A meta-analysis of 30 cross-sectional studies (
8) found that, based on self-report data, the lifetime prevalence of suicide attempts among LGB individuals was 2 to 5 times higher than among heterosexuals. A recent integrative review (a mix of nine quantitative, two qualitative, and two mixed-method studies) examining emergency care of youths who identify as lesbian, gay, bisexual, transgender, queer/questioning+ (LGBTQ+) for suicidality highlighted the need for high-quality and representative quantitative evidence (
9). The review noted that existing studies relied on convenience samples and survey measures of suicidality (typically through a single self-reported item), which may not provide valid and reliable estimates. Previous studies examining SRB by sexual orientation have been limited by small samples (
10–
15), convenience samples or selection bias (
13,
14,
16,
17), and cross-sectional design (
8,
11,
12,
15–
17). The vast majority of studies, including the few longitudinal studies (
10,
13,
18,
19), rely only on self-report data. While self-report data are useful in identifying nonfatal, subclinical, or minor SRB events, they do not provide a complete picture. They are limited by survivorship bias in that SRB may only be reported by those who survive or are healthy enough to participate in surveys. Self-reported SRB is also subject to social desirability bias (
20), and some participants are unwilling to disclose SRB because of social stigma. As a result, complete population-based estimates of the SRB disparity by sexual orientation are lacking.
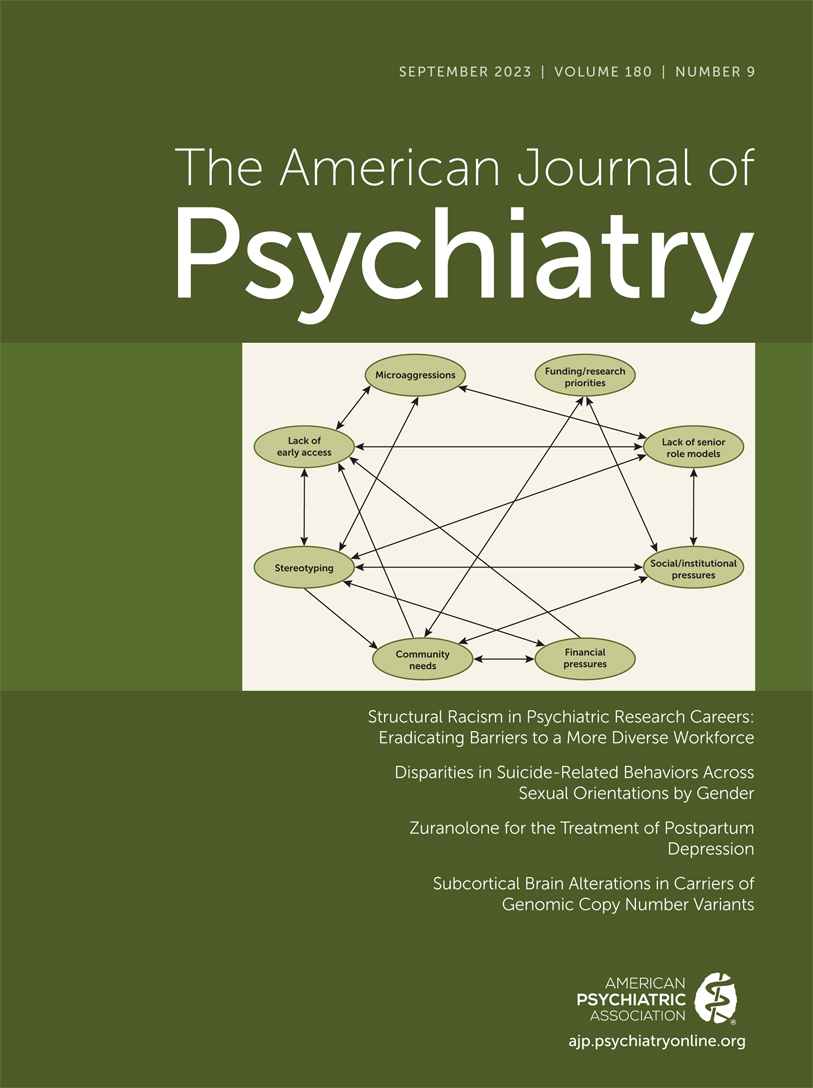
Our comprehensive search using MEDLINE and Scopus yielded only five studies (in the past 25 years) using non-self-reported events and based on randomized population-based samples that estimated SRB disparities across sexual orientations (see Figure S1 in the
online supplement for the search strategy and the PRISMA flowchart). However, the evidence from these studies is limited by several factors. Three studies from Denmark and Sweden (
21–
23) investigating suicides across sexual orientations used same-sex partnership or cohabitation status as a proxy for LGB status, which led to 1) the inability to differentiate between bisexual and gay/lesbian individuals, 2) the exclusion of nonpartnered LGB individuals, and 3) the misclassification of bisexuals with an opposite-sex partner as non–sexual minorities. In another study (
24), using linked mortality records and a U.S. nationally representative survey, only 85 sexual minority men were included, and the study was underpowered to model a regression for SRB events (i.e., insufficient number of events). Another study (
25), using U.S. Veterans Affairs linked data, found that the suicide rate among sexual minority veterans was 82.5 per 100,000 person-years (compared with 37.7 in the general veteran population). However, among the study limitations were that 1) sexual orientation was not self-reported but was extracted from medical notes, 2) gays/lesbians and bisexuals were not differentiated, and 3) the study years spanning 2000 to 2017 occurred during the “Don’t ask, don’t tell” policy era, where disclosure could lead to being dishonorably discharged. The five studies examined suicides using mortality records, but suicide attempts based on health administrative or clinical data were either not available or not examined. By treating all sexual minorities as a single group, these studies were unable to differentiate effects between gay and bisexual individuals, which may lead to an incorrect assumption that effects are homogeneous across sexual minority subgroups.
Suicides incur an economic burden to Canadian society estimated to be equivalent to $2.4 billion annually (
26), and research on high-risk groups, including LGB individuals, will help reduce this economic burden. Since LGB individuals have higher health care needs compared to the general population (e.g., higher prevalence of depression [
27] and health care utilization [
28]), accurate estimation of differential SRB risk is important for prioritizing the funding of clinical and social service programs aimed at improving the health of LGB individuals. Without high-quality evidence to quantify SRB disparity by sexual orientation, governments, policymakers, and nonprofit organizations may not be willing to redirect scarce resources and time to address the potentially greater risk among LGB individuals. The need for better evidence is also buttressed by the growing proportion of the population that identifies as non-heterosexual (
29). For instance, while 91.1% and 88.6% of Baby Boomers and Generation X, respectively, identify as heterosexual/straight, the proportion is 78.9% in Generation Z (born 1997–2002).
In this study, we investigated whether there are differences in the risk of SRB across sexual orientations by gender. Guided by the minority stress model and findings from previous research, we hypothesized that LGB individuals have a higher risk of SRB compared with their heterosexual counterparts. Previous research has found significant variation in the patterns and driving factors of suicidal behaviors between LGB men and women (
30), and a gender-stratified approach is necessary to address this heterogeneity. We used a population-based representative sample linked to medical records for people residing in Ontario, the most populated Canadian province (with 14.5 million residents in 2019), to investigate the disparity in emergency department presentation or hospitalization for SRB by sexual orientation.
Methods
Our study cohort was created using Ontario participants from multiple cross-sectional cycles of the Canadian Community Health Survey (CCHS), which is linked to longitudinal health administrative data sets, including the Discharge Abstract Database, the Ontario Mental Health Reporting System, the National Ambulatory Care Reporting System, the Ontario Health Insurance Plan, and the Office of the Registrar General–Deaths. These data sets were linked using unique encoded identifiers and analyzed at ICES (formerly the Institute for Clinical Evaluative Sciences). ICES is an independent nonprofit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. This study was approved by the Research Ethics Boards at Brock University (ethics approval number 19-150-CHUM) and at York University (ethics approval number 2022-268).
Study Sample
The study cohort was constructed from six cycles of the CCHS (2003, 2005, 2007/08, 2009/10, 2011/12, 2013/14), using a standard method to combine multiple cycles of the survey (
31). Individuals age 18 or older (at the time of survey completion) from Ontario surveyed in any one of the CCHS cycles from 2003 to 2014 were included in the study sample. The CCHS is a cross-sectional survey that uses a consistent method of multistage stratified cluster sampling to collect sociodemographic and health-related information from a representative sample of people in private dwellings, with an average response rate of 74% (unweighted N=123,995). Each person was followed, through the health care records, from their CCHS interview date until March 31, 2019, or until they died or lost eligibility for provincial universal health care (e.g., moved out of the province). In other words, our study had a staggered enrollment approach in which an individual who completed the CCHS in 2003 could be in the study for up to 17 years, but an individual who completed the CCHS in 2013/14 could have a maximum of 7 years.
Sexual orientation was ascertained by a single-item question on the CCHS: “Do you consider yourself to be…,” with the following as possible responses: “heterosexual (sexual relations with people of the opposite sex), homosexual, that is, gay or lesbian (sexual relations with people of your own sex), bisexual (sexual relations with people of both sexes).” A previous study (
32) showed that the kappa statistic for agreement between this question and a multi-question instrument was 0.89 and that it captured 99.3% of those who identified as a sexual minority on the multi-question survey and 98.4% of those with a past-year same-sex partner.
Outcome Measures
Our primary outcomes were nonfatal self-harm and fatal suicide events that are associated with an emergency department presentation or hospitalization. Nonfatal self-harm events with ICD-10 diagnostic codes in the range of X60–X84 (intentional self-harm) were captured using the National Ambulatory Care Reporting System, the Discharge Abstract Database, and the Ontario Mental Health Reporting System. In a study that compared ICD-10 codes to clinical assessment using the Columbia Classification Algorithm of Suicide Assessment (
33), the inclusion of undetermined injuries and deaths (Y10–Y34) improved sensitivity of detecting SRB from 36.9% (95% CI=32.4–41.4) to 41.0% (95% CI=36.4–45.6), while its impact on specificity was negligible, from 98.8% (95% CI=98.3–99.2) to 97.9% (95% CI=97.4–98.4). A systematic review has shown that undetermined deaths and injuries should be included when identifying suicide and self-harm-related injuries and deaths (
34,
35). Fatal suicide events included those in which individuals were dead at discharge from the hospital or emergency department for the above-listed events, and fatal SRB events at home, in the community, or in nonclinical institutions were identified using the Office of the Registrar General–Deaths, using the same diagnostic codes.
Covariates
The following sociodemographic information was included in our models: year of birth, gender, ethnic minority status, level of education attained (postsecondary graduate vs. not), marital status (married vs. unmarried), rurality (rural vs. nonrural, based on Canada Post rural postal codes [
36]), and comorbidity indicator. Information on gender was obtained from the Registered Person Database, which reflects sex assigned at birth for anyone who is eligible for universal health care services in Ontario. Since 2017, the Ontario government has allowed for sex designation to change to conform with gender identity, but a letter from a physician is required and may still be a barrier for some trans individuals (
37). However, only binary gender is indicated in the database (M or F), and no indicator is available for transgender status. For the comorbidity indicator, we used the Aggregated Diagnosis Groups produced by the Johns Hopkins Adjusted Clinical Group System (version 10), which is based on 32 diagnosis clusters and indicates the burden of morbidity (
38,
39).
Analysis
We first calculated both the crude rates of SRB events and the number of individuals with at least one SRB event across gender and sexual orientations at a 5% significance level. Next, we performed unadjusted and adjusted Cox regression analyses to examine the relationship between sexual orientation and time to first SRB event, accounting for the effects of the aforementioned covariates in adjusted analyses. We assessed the proportional hazards assumption by plotting the log of negative log estimates over the log survival time for each sexual orientation to determine their degree of parallelism (
40). Hazard ratios were calculated from the models. For each model, gender-stratified analyses were conducted, given the gender difference in suicidal behavior identified in previous research (
12). Given that SRB as a concept includes fatal and nonfatal events, we also conducted a sensitivity test to assess whether the results were similar for only nonfatal events. Statistical analyses were performed using SAS, version 9.4 (SAS Institute, Cary, N.C.), and 95% confidence intervals were used. To account for the complex sampling strategy of the CCHS and to ensure representativeness, survey weights were applied and bootstrapping methods were used to estimate the 95% confidence intervals for all analyses.
Missing Data
Since population-wide health administrative data were used, loss to follow-up was generally not a concern, both because our data capture all acute care visits in Ontario and because those who started the study period with health care eligibility and subsequently lost their eligibility (e.g., died or relocated to another province/country) were appropriately censored at the point of ineligibility. The levels of missingness for covariates are summarized in the footnote to
Table 1. We included individuals who elected not to state their sexual orientation as a separate category (“not stated”) in our models. Missingness in other covariates led to listwise deletion, so we corrected for potential bias in the standard errors using nonparametric bootstrapping with 500 replicates (with bootstrap weights provided by Statistics Canada [
41]), which has been shown to be sufficient when only a standard error is required (
42).
Results
Descriptive Statistics
Our sample included 123,995 individuals, with a total of 2,098,559 person-years in the unweighted data set. The average follow-up time was 11.4 years. A total of 164 people died from suicide, and 3,192 people had at least one nonfatal SRB event. All of the following results were weighted to ensure representativeness of the sample (
31).
Table 1 presents key covariates across sexual orientations, and
Table 2 presents the weighted number of persons, person-years, and incidence rates of SRB events per 100,000 person-years. The crude incidence rate of SRB events per 100,000 person-years was 224.7 among heterosexual individuals, 664.7 among gay/lesbian individuals, and 5,911.9 among bisexual individuals. Bisexual individuals were younger on average than the rest of the sample (mean age, 33.9 years compared with 42.3 years), and fewer had completed postsecondary education (42.8% compared with 52.6%). See Table S1 in the
online supplement for age-adjusted rates of SRB events per 100,000 across sexual orientations.
In
Figure 1, the log-log plot of survival functions curve shows the estimated survival function (log-log survival curve plotted against survival time). The figure demonstrates that a constant hazard ratio over time is observed for individuals with different sexual orientations, which is an assumption for Cox regression models.
The hazard ratios from models 1 and 2 (
Table 3) show that sexual minorities were more likely to experience SRB events than heterosexuals. In an age- and gender-adjusted model for the overall sample (model 1), the likelihood of an SRB event was 3.64 times greater among bisexual individuals (hazard ratio=3.64, 95% CI=2.53–5.24) and 2.43 times greater among gay/lesbian individuals (hazard ratio=2.43, 95% CI=1.37–4.31) compared with heterosexual individuals. Similar results were obtained in the fully adjusted model (model 2), where bisexual individuals were 2.98 times (95% CI=2.04–4.27) more likely to have an SRB event and gay/lesbian individuals 2.10 times (95% CI=1.18–3.71) more likely compared with heterosexual individuals.
Gender-stratified models (
Table 3, models 3–6) showed a higher likelihood of SRB events in sexual minority groups among both men and women. In model 3 (age-adjusted), gay men (hazard ratio=2.36, 95% CI=0.92–6.03) and bisexual men (hazard ratio=2.41, 95% CI=1.20–4.86) were more than two times more likely to have an SRB event. In model 4 (fully adjusted), the hazard ratio for bisexual men was 2.04 (95% CI=1.01–4.11), and the hazard ratio for gay men was 2.10 (95% CI=0.83–5.32). In both models 3 and 4, while gay men had a higher estimated risk of SRB events, the estimates did not reach statistical significance. In model 5 (age-adjusted), lesbian and bisexual women were 2.54 (95% CI=1.33–4.87) and 4.23 (95% CI=2.73–6.53) times more likely, respectively, than heterosexual women to have an SRB event. These elevated risks persisted in the fully adjusted model (model 6). In the fully adjusted model in the sensitivity analysis (full sample), where suicide deaths were excluded, bisexual individuals were 3.09 times (95% CI=2.15–4.44) more likely to have an SRB event, and gay/lesbian individuals were 2.11 times (95% CI=1.16–3.85) more likely, relative to heterosexual individuals (see Table S2 in the
online supplement) (
17). We conducted further analyses based on models 4 and 6 to investigate the SRB disparity between gay/lesbian and bisexual individuals, and we found that the hazard ratio for bisexual men compared with gay men was 0.97 (95% CI=0.77–1.22), and the hazard ratio for bisexual women compared with lesbians was 1.56 (95% CI=1.26–1.93).
Discussion
Our study provides high-quality evidence for the disparity in SRB across sexual orientations, using health administrative data and a population-based randomized sample. We found that sexual minority individuals were 2.10 to 4.23 times more likely to have SRB events compared with their heterosexual counterparts. Bisexual individuals had the highest risk, followed by gay/lesbian individuals; disparity relative to heterosexuals was greatest for women. In a previous review and meta-analysis based on self-reported suicidal behavior (
8), the lifetime prevalence of suicide attempts was 4% among heterosexual individuals and 11%–20% among sexual minority individuals. In contrast, using health administrative data and a follow-up period of 11.4 years, our study found the prevalence of one or more SRB events to be 2.2% among heterosexual individuals, 5.2% among gay/lesbian individuals, and 8.0% among bisexual individuals. While the meta-analysis found that LGB respondents had 2.75 to 5 times the likelihood of lifetime self-reported SRB risk compared with heterosexuals, our findings indicate a range 2.04 to 3.37 times the risk across LGB individuals. By focusing only on the most serious behaviors (i.e., SRB events that require emergency department visits or hospitalization or lead to death), our findings seem to be more consistent with previous studies of self-reported SRB events that report a smaller disparity.
A previous meta-analysis (
43) found that bisexual individuals had 1.25 times the risk of lifetime SRB events compared with gays/lesbians. Further analyses using sex-stratified models show that the elevated risk among bisexual individuals is more pronounced among bisexual women (an odds ratio of 1.48 relative to lesbians) compared with bisexual men (an odds ratio of 1.00 relative to gay men). An interaction between gender and sexuality was also reflected in our study; additional calculation based on the hazard ratios obtained showed that bisexual women have 1.56 times the risk of SRB events relative to lesbians, while bisexual men did not appear to have more risk compared with gay men. The differential SRB risk between bisexual men and bisexual women may be attributable to 1) lower levels of LGBT+ community support experienced by bisexual women (
43,
44); 2) the mental health benefits associated with heterosexual partnership for bisexual men (if they have an opposite-sex partner), while women’s role as caregiver may reduce the mental health benefits from similar partnerships (
43); or 3) bisexual women’s higher risk of trauma, particularly through intimate partner violence, relative to lesbian women (while the difference is negligible between bisexual and gay men) (
43). Further research is needed to test whether these pathways may explain gay/lesbian–bisexual disparity in SRB risks.
There are some limitations to this study. First, there may be unmeasured confounders, such as employment status. However, socioeconomic indicators (e.g., employment, housing, income, etc.) may work as a mediator between LGB status and SRB, which may bias estimates of the direct effect of LGB status on SRB. Second, ICES collects health administrative data of Ontario residents, and those who moved out of the province are censored, which could bias the estimates in an unknown direction if there was differential attrition across sexual orientations. Third, the sample was not large enough to examine SRB fatal events alone; therefore, our results are mostly driven by nonfatal SRB events. Fourth, our sample did not include individuals with nonbinary gender, and we could not estimate its effects in our models. Fifth, sexual orientation in our study included only heterosexual, gay/lesbian, and bisexual, but did not include other orientations (e.g., asexual and queer). Sixth, while we stratified our analysis by gender and adjusted for age, there may be effect modifications by birth cohort confounding the relationship between sexual orientation and SRB. The study sample was not sufficiently large to carry out both gender- and cohort-stratified analyses. Seventh, sexual orientation was treated as a time-invariant characteristic, but it may change over time. Our use of sexual orientation as a time-invariant variable is validated by previous findings in which 96% of individuals were not observed to change how they identify within a 7- to 8-year period (
45). Furthermore, the typical shift is from heterosexual to LGB, or bisexual to gay/lesbian, aligning with the coming out process. Hence, some LGB individuals may be misclassified as heterosexual, which in turn possibly biases the results toward null. Finally, sexual orientation was determined using a single-item inquiry administered by a trained interviewer. It is possible that the number of LGB individuals was undercounted as a result of the lack of inquiry about sexual behaviors and attraction, as well as respondents’ discomfort with disclosing their sexual orientation to the interviewer.
This is, to our knowledge, the first study using a representative sample and medical diagnoses to quantify SRB events across heterosexual, gay/lesbian, and bisexual individuals, which improves the generalizability of our study compared to many prior studies that relied on convenience samples. Most importantly, while previous research provided evidence of SRB disparities by sexual orientation using self-report data, we show that the disparity is consistently observed even when limited to the most serious SRB events—those leading to medical interventions or deaths. In addition, our use of health administrative data (as opposed to self-report data) may help reduce survivorship bias and social desirability bias. While many previous studies combined LGB into a single category (i.e., sexual minority), our sample included disaggregated estimates for gays/lesbians and bisexuals, by gender, to produce separate estimates for each subgroup. Our study highlights the need for health care practitioners to assess suicide risk and suicidal ideation in sexual minority patients.
Further research is needed to identify mitigating factors that can protect sexual minorities from an elevated risk of suicidal behavior. LGB individuals experience greater interpersonal and structural discrimination, which creates roadblocks to receiving necessary care (
46). Further training and education of clinicians and psychiatrists to improve awareness and sensitivity toward SRB risk among LGB patients is needed to reduce SRB in this population. For example, LGB individuals may experience minority stress as a result of trauma from family rejection or bullying at school for being gay or lesbian. Clinicians can be educated on these common sources of minority stressors relevant to the LGB community so that they are better able to understand and help mitigate risks associated with them. Furthermore, psychiatrists and health care professionals should regularly screen bisexual women for psychiatric mental health symptoms, paying particular attention to those suffering from lower social supports, given the underutilization of necessary mental health services in this population (
42,
47). In addition, the collection of sexual orientation data has a high level of acceptability (
42), and given the higher risk of SRB among sexual minorities, it is important to consider sexual orientation as a part of routinely collected data to improve patient care.
Acknowledgments
Parts of this material are based on data on deaths compiled and provided by the Ministry of Health, the Canadian Institute of Health Information, the Canadian Community Health Survey, and the Ontario Registrar General, the original source of which is ServiceOntario.