T
o the E
ditor: While dreaming during anesthesia is common (
1), it is not known whether this phenomenon differs from normal dreaming or has post-surgical benefits. We present two cases of female patients who experienced rapid and sustained reduction of posttraumatic stress disorder (PTSD) symptoms immediately following anesthetic-based EEG-guided intraoperative dream induction. Both patients underwent surgeries and received propofol/opioid-based anesthetics. Upon finishing the surgery but before emergence, we maintained a pre-emergent anesthetic state characterized by specific frontal cortical activity for several minutes: reduced alpha power and enhanced beta power (
2). Based on previous findings showing that dreaming during anesthesia is associated with more high-frequency frontal power before emergence (
3) or as compared to connected consciousness (
1), we believe this cortical activity reflects dreaming while being sedated. Patients were interviewed immediately upon emergence, and both reported having had vivid dreams.
Both patients were identified as part of a quality-improvement program to enhance recovery after surgery, which includes informing patients of the possibility of dreaming without priming content, minimizing likelihood of emergence agitation through use of intravenous rather than inhalational anesthesia, minimal sensory input during gradual anesthetic emergence (
4), and assessment for intraoperative awareness and dreaming immediately on emergence using a modified Brice Questionnaire (
5). After identification, both patients provided informed consent for retrospective psychiatric diagnostic interviews. Patients were not identified preoperatively. Anesthetic adjustments, assessment, and diagnostic interviews adhere to established standards of care, received approval from the IRB, or fall under IRB exemption (IRB exempt protocols #54043, #59783, #65538, #67245; informed consent provided on IRB protocol #67399).
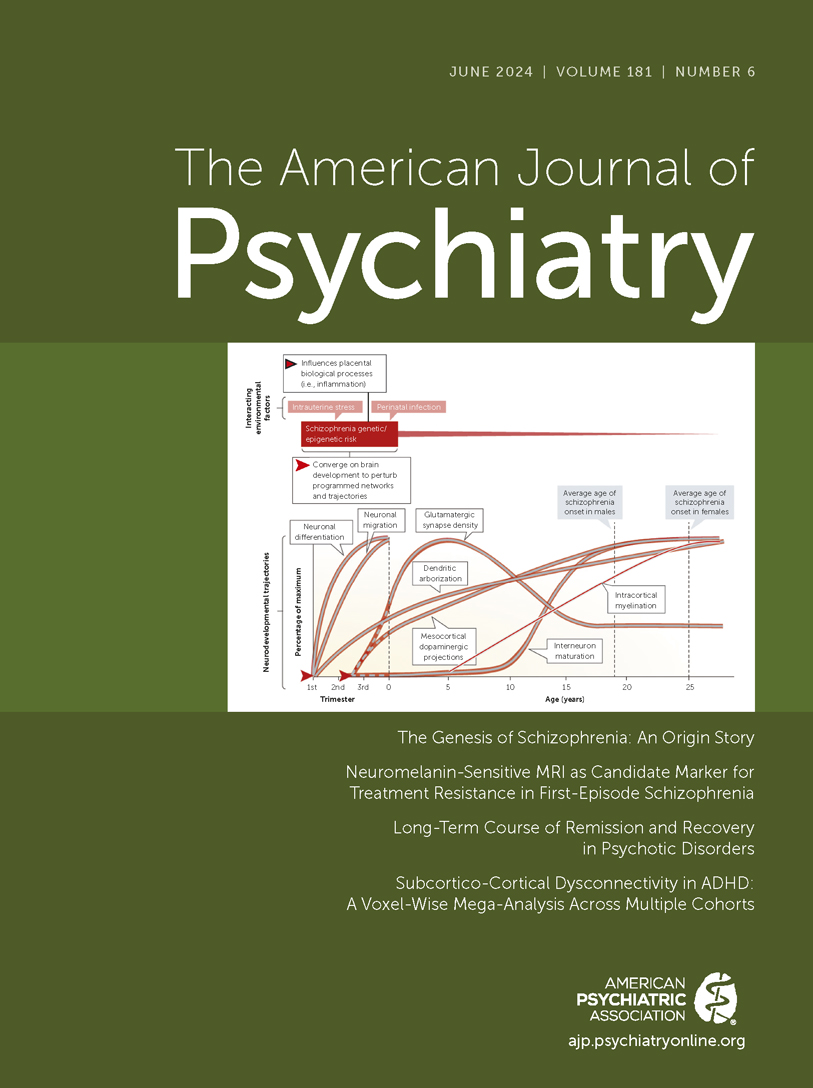
Patient 1, a 57-year-old White female with no current alcohol, tobacco, or drug use and noncontributory medical history except invasive ductal carcinoma of the right breast, presented for a right breast lumpectomy and axillary lymph node biopsy. She was not taking psychiatric medications at the time of surgery. She endorsed one nightmare per week about her son, who had died by suicide in 2017. She recalled two “euphoric” intra-operative dreams: in one, she experienced her son’s birth, originally traumatic, as deeply joyful; in a second, she spent time with her adult son and experienced cathartic relief. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) indicated a diagnosis of PTSD pre-operatively. One-month post-surgery, she no longer met criteria for PTSD, and by 1 year, she had remitted. Self-report scales indicated improvement in depression, anxiety, and sleep (
Figure 1). The patient reported that she has not had a nightmare “in over 18 months” and that her experience during surgery “saved her life.”
Patient 2, a 72-year-old White female with no reported alcohol, tobacco, or drug use and noncontributory medical history except hyperparathyroidism, presented for parathyroidectomy. She was taking fluoxetine for anxiety and depression at the time of surgery. She reported occasional nightmares about her son in the month pre-surgery, who died in 2000 from alcohol poisoning during a college fraternity hazing. Intra-operatively, she dreamed about being with her late son and other family members and described the dream as “very positive.” CAPS-5 assessment indicated that she met criteria for PTSD in the month pre-surgery but not in the month post-surgery, and self-report scales for anxiety and depression showed improvement (
Figure 1). She denied nightmares in the month post-surgery.
Anesthetic-induced prolonged dream states may serve as an emotion regulation function. Patients experiencing fear memory elements (i.e., dreaming about their sons) on a background of anesthetic-induced low arousal may have contributed to fear extinction (
6). We recently presented a case of resolution of acute stress disorder (
2) after anesthetic-induced intra-operative dreaming. These collected cases suggest that anesthetic-induced intra-operative dreaming may be therapeutic in both recent onset and long-standing trauma disorders and have a rapid and durable effect. This preliminary evidence justifies an open-label study of deliberate induction of dreaming with anesthesia in PTSD.