The challenges of early identification and treatment of individuals with psychotic disorders are substantial. Among the heterogeneous groups of teens identified as being at high risk for psychosis, based on clinical manifestations established by interviews and scales, only about 1 out of 4 individuals actually converts to a chronic psychotic disorder (
1). This 75% “false positive” rate reflects both the complex interplay of neurological and psychological development during transitional ages and highlights the limits of resolution of the clinical interviews designed to identify psychosis “proneness.” The need for better prediction with actionable follow-up has driven the search for neurocognitive, neuroimaging, and neurophysiological biomarkers, among others (
2). And because even the best biomarkers add only modestly to predictive accuracy for psychosis, “conversion calculators” have been tasked with applying algorithms to draw from the predictive power across multiple different biomarkers (
3). Our field has fully embraced the notion that early identification and treatment are the keys to preventing the destructive arc of the schizophrenias, and has progressed from the sole reliance on imprecise clinical scales to the hope of applying direct and reliable brain-based biomarkers to prediction algorithms to bend this curve.
In this issue, Hou et al. (
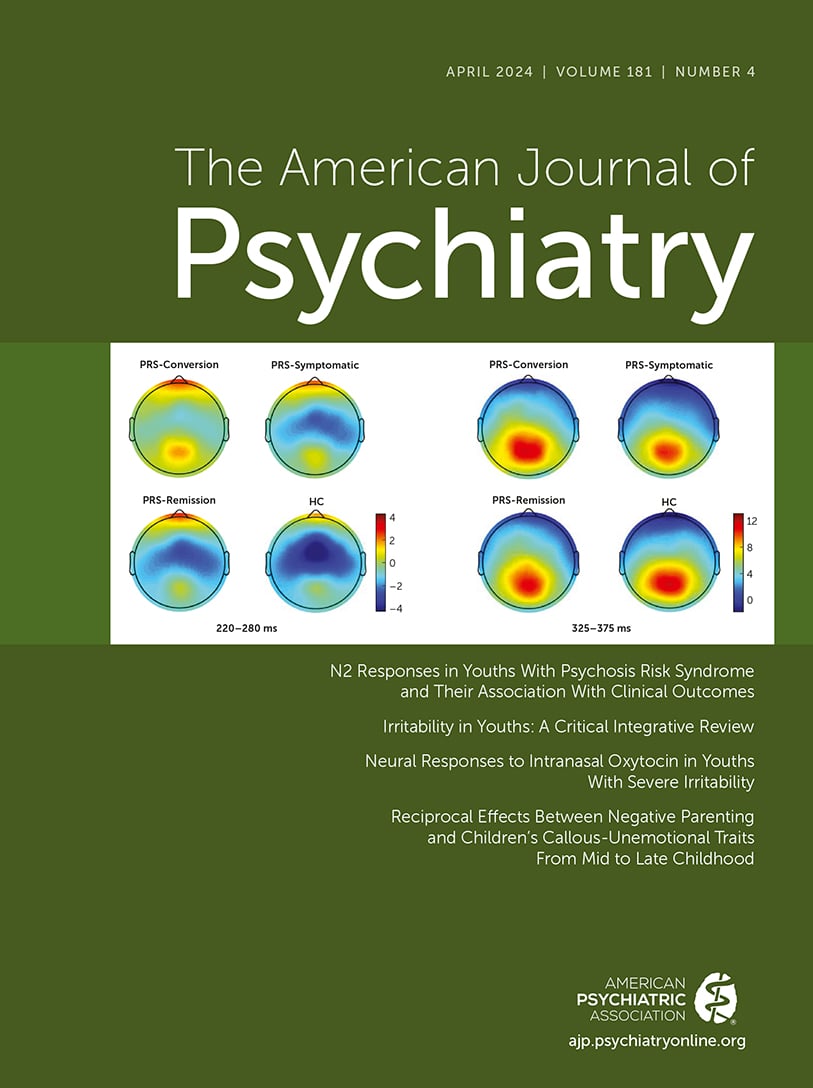
4) describe their efforts to evaluate biomarkers of brain function. They screened nearly 8,800 college freshmen to identify 122 individuals—about two-thirds of them women—whom they characterized as having a “psychosis risk syndrome,” based on the widely used Structured Interview for Psychosis-Risk Syndromes (SIPS), the Scale of Psychosis-Risk Symptoms (SOPS), and the Mini-International Neuropsychiatric Interview (MINI). These individuals completed a visual oddball task during EEG recording in order to evoke event-related potentials (ERPs) to target stimuli. The authors used a version of this oddball paradigm that is unique both because it uses visual stimuli to drive ERPs (vs. the more common auditory ERPs) and because the test session includes a third “interference” stimulus in addition to the commonly used frequent “standard” and infrequent “oddball” target stimuli. This interference stimulus is reasonably presumed to increase the attentional demands of the target detection task. While the majority of ERP studies using target detection tasks report on the extensively studied P3 ERP component, another large voltage component that precedes P3, known as the N2, is often overlooked. Like the P3, N2 is also associated with selective attention and peaks 220–280 msec following correctly identified targets.
Of the potential neurophysiological biomarkers assessed by this group in response to the different stimuli presented, the lesser-studied N2 response was the one most associated with both psychosis risk syndrome phenotype and conversion to psychosis. Specifically, individuals with psychosis risk syndrome exhibited reduced (“less negative”) N2 amplitude compared with age-matched healthy comparison subjects; depressed and/or anxious individuals (those in an “emotional disorders” comparison group) exhibited intermediate N2 amplitudes. A skeptic might point to the unfortunate circularity of validating a precise neurophysiological assay of brain function (low N2 amplitude) based on its association with a fuzzy clinical phenotype (psychosis risk syndrome) established by imprecise clinical interviews (SIPS, SOPS, and MINI). Nonetheless, 12 months later, roughly 20% of the individuals with psychosis risk syndrome had converted to psychosis (the conversion subgroup), while 46% remained symptomatic but not psychotic (the symptomatic subgroup) and 34% had remitted (the remission subgroup). Importantly, the critical outcome—conversion to psychosis—was predicted by reduced N2 amplitudes 12 months earlier: N2 amplitudes were significantly lower among individuals in the conversion subgroup than among both those in the symptomatic subgroup (d=0.58) and those in the remission subgroup (d=0.5). And while there are other interesting findings with task-related reaction time (not predictive of conversion) and the correlation of N2 with SOPS positive symptoms (counterintuitively, more severe symptoms were associated with more “normal” N2 amplitude), the most exciting new finding in this report is the potential ability of N2 amplitude in individuals with psychosis risk syndrome tested in a three-stimulus oddball visual ERP paradigm to predict conversion to psychosis 12 months later. The authors do not speculate how much this N2 effect would contribute to a predictive model, but with an effect size between 0.5–0.58, it’s very likely that this measure would need to be bundled with other potential predictors to contribute to a scalable and actionable multivariate conversion algorithm. This is a notable and important story of a biomarker, graduating from laboratory development into potential utility in the real world, and which now will need to withstand rigorous testing with large samples, likely within international consortia.
There is a long history and rich literature connecting deficits in ERP-based measures of deviance detection to chronic psychosis; from this perspective, the present findings linking N2 deficits with psychosis are not unexpected. But the ability of these N2 deficits to predict conversion to psychosis 12 months later is a new and important extension of this literature. This is a timely finding given the significant effort being directed toward validating such biomarkers for psychosis. For example, the Accelerating Medicines Partnership for Schizophrenia is an international multisite consortium that is evaluating multiple biomarkers across domains, including EEG, to develop a reliable platform for testing novel therapeutics in clinical high-risk cohorts tested and retested after 2 months (
5).
There is another story here, “beyond the biomarker,” about the heroic efforts taken to identify a single biomarker with, at best, modest discriminative power, which now must be moved—at much greater cost and effort—to the real testing grounds of large multisite inquiry. Given the failures to develop substantially better outcomes for youths at high clinical risk based on clinical information alone, substantial resources have been directed toward this quest of earlier biomarker-based identification and treatment. This would seem to be a rational strategy given improved outcomes resulting from early intervention for heart disease, cancer, and other serious medical illnesses. But these other forms of illness have a pipeline of viable treatment options awaiting them after they’ve been “caught early,” and this is not the case for the schizophrenias. Even intensive multidimensional interventions provided early to high-risk cohorts yield mixed results (
6). Moreover, for “converted” schizophrenia patients, the newest antipsychotics impart only modest functional gains (
7), yet carry significant risks, including metabolic syndrome, anticholinergic burden, and a long list of morbidities. Indeed, given state-of-the-art treatment, schizophrenia patients on average will have a lifespan shortened by 14.5 years (
8). Since we are making such a major investment in the thus far unsubstantiated hope that early identification of “converters” can bend the curve on the schizophrenias, we should do everything within our power to make sure that we’ve got effective, scalable, shovel-ready treatment paradigms for those who convert. So far, we don’t.
Certainly, there is an appeal to working with a patient population that is early in their illness, before the clinical course is dominated by stigmata of complex medications, comorbidities, and functional decline. By contrast, there may be a form of “learned helplessness” among those developing treatments for chronic psychosis, based on the marginal gains in functional outcome after more than six decades of reliance on antipsychotic medications, and the apparent lack of efficacious alternatives. We’ve suggested that there is an urgent need for alternative treatment strategies for the schizophrenias, including the use of medications to enhance gains from cognitive interventions for psychosis, rather than to suppress psychosis per se (
9,
10). Other “outside the antipsychotic box” strategies are now being used to manipulate cholinergic systems, either with procholinergic interventions against a primary target of psychosis (
11) or by reducing anticholinergic burden to maximize cognitive resources and minimize risk of cognitive decline (
12). There will be a need for laboratory biomarkers that predict sensitivity to each of these novel interventional strategies, and it seems likely that these biomarkers will differ from those that predict conversion to psychosis. Testing novel therapeutic strategies for schizophrenia is painstaking work, but it’s the heavy lift we need to make.
Hou et al. have moved the field a large step forward, by using an ERP paradigm to demonstrate that visual N2 amplitude is associated both with psychosis risk syndrome and with the psychosis risk syndrome subgroup that converts to psychosis within 1 year. This type of tool will require substantial validation as part of a large effort to enhance our ability to predict psychosis conversion through the use of laboratory-based biomarkers and related algorithms. We note that, in this effort, it will be important to maintain a clear focus on what new we will have to offer these converters “beyond the biomarkers.” Novel strategies for efficacious, function-sparing therapeutics are needed to address the challenges that those who convert to psychosis will face across their lifetime.