A perennial challenge for psychiatric neuroimaging has been to establish its relevance to the delivery of care in the clinic. As neuroimaging researchers, we are encouraged by our growing understanding of psychiatric symptoms and their brain architectural and connectivity correlates. And yet, as clinicians, whether in the early psychosis clinic or the inpatient unit, there remains a gap from scanner to the bedside that highlights an unmet need in clinical translation of psychiatric neuroimaging.
In a study reported in this issue, Gallucci et al. (
1) use an elegant approach to take on such a challenge. The authors attempt to identify and distinguish the pathophysiology of both depressive symptoms and the negative symptoms of schizophrenia (e.g., expressive blunting, anhedonia, amotivation).
The challenge is immense both in terms of its scientific difficulty and of the urgency of unaddressed clinical need. To review briefly: there is considerable overlap between the constellation of symptoms that define a depressive episode and the negative symptoms of schizophrenia. One example is anhedonia, which can be broadly defined as the inability to derive pleasure from experiences (either current or anticipated). Despite the similarity in subjective experience, we know that anhedonia associated with these different causes has different etiologies and also differs in terms of response to pharmacological treatment (
2). The presence of negative symptoms poses a unique challenge to identifying worsening depression, which can ultimately result in untreated disability and suffering. The significant impact of this unmet need may be most acutely demonstrated in the early years after an initial psychotic episode, during which rates of suicide attempts and deaths by suicide are enormously elevated (
3).
There has been a long-standing effort to develop instruments to identify and quantify depression in the presence of negative symptoms of schizophrenia. The Calgary Depression Scale for Schizophrenia (CDSS) was developed to address this need (
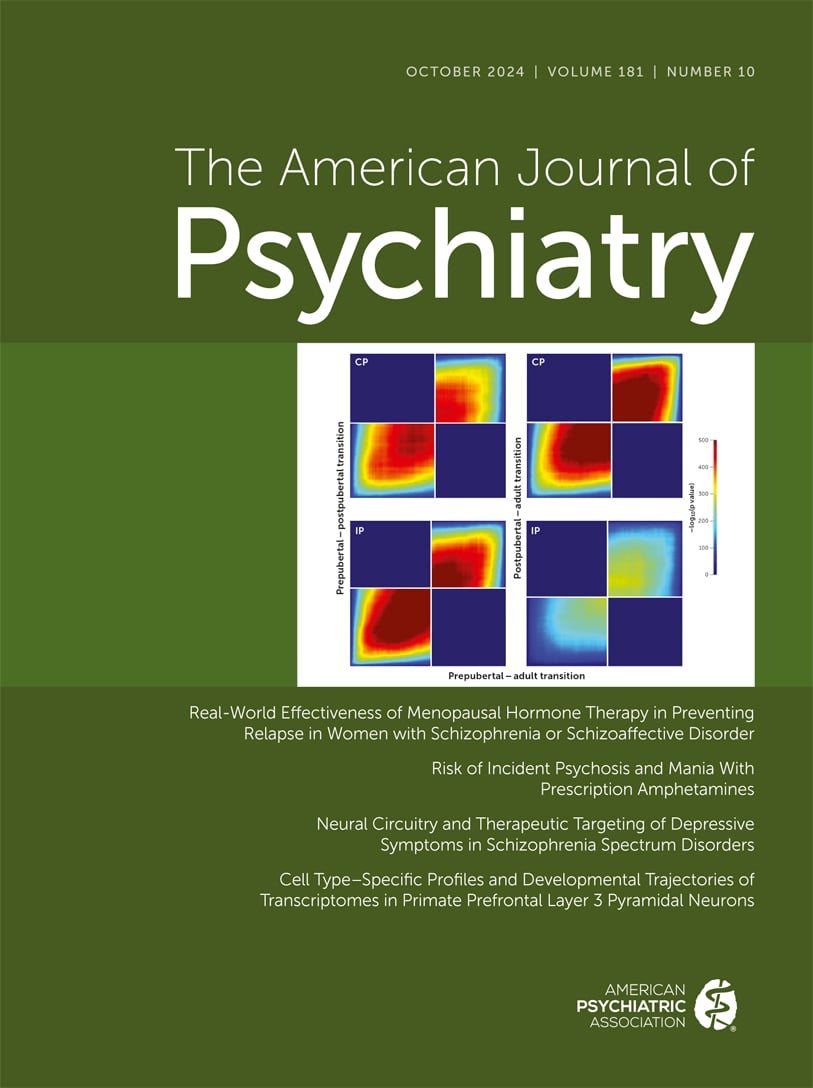
4). More recently, a small number of studies have attempted to find neuroimaging correlates of depressive symptoms in individuals with psychotic disorders. Gallucci et al. take a sophisticated and nuanced approach to this effort, employing task-free (resting-state) functional imaging to elucidate connectivity correlates with symptoms, with the overarching goal of determining whether brain network organization varies with negative symptoms and depressive symptoms in distinct or overlapping spatial patterns.
To achieve this goal, the authors work with an impressively large sample of individuals with schizophrenia spectrum disorders. Notably, the sample includes individuals at varying stages of illness, from patients in a first episode of psychosis to those with many years of lived experience with schizophrenia. These cohorts were not selected specifically for symptom severity, and almost a quarter of the participants described no depressive symptoms at all on the CDSS and were excluded from further analysis.
The analytic approach referred to as partial least squares correlation (PLSC) was chosen to identify latent relationships between different items on two instruments that quantify the severity of depressive symptoms (the CDSS) and negative symptoms (the Scale for the Assessment of Negative Symptoms) and whole brain functional connectivity in every participant. This approach prioritizes orthogonality, that is, the identification of latent variables (LVs) that are distinct from each other, but when combined account for maximal variance in relationships between symptom severity and brain connectivity.
The resulting latent variables of symptoms are consistent with previous studies (
5,
6): The CDSS can be described as at least two factors (here described as LV1 for “general depressive” symptoms and LV3 for “guilt and early waking” symptoms), both of which are uncorrelated with negative symptom severity (here described as LV2). Variance in each of these symptom clusters was associated with variance in a heterogeneous array of functional connectivity edges, or pairwise relationships between brain regions. In other words, the correlated activity in widely distributed anatomical regions was associated with these three different symptom clusters. The patterns of functional connectivity linked to each symptom cluster defy easy categorization and represent a highly diverse set of within-network, between-network, and both positive and negative correlations between symptom severity and functional connectivity. One notable feature might be the lack of overlap between functional connectivity edges in each of the different latent variables. This could represent true biologically distinct processes or could alternatively be the product of the symptom scales used as well as an analytic approach that identifies orthogonal factors to maximally account for variance.
With latent symptom-brain relationships now identified, the investigators then performed a rigorous (and rarely attempted) effort to validate the dissociation between symptom clusters and neuroanatomy. Specifically, if symptoms are associated almost entirely with nonoverlapping neuroanatomy, a highly spatially localized intervention could have distinct effects on one symptom cluster and not others. The investigators reanalyzed data from a previously published sham-controlled clinical trial in which individuals with schizophrenia spectrum disorders received repetitive transcranial magnetic stimulation (rTMS) targeting the dorsolateral prefrontal cortex (DLFPC) bilaterally daily for 4 weeks. Although these rTMS stimulation targets overlapped with cerebral territory linked to all three latent variable symptom clusters, there was a highly specific reduction in the “general depressive” symptoms of latent variable LV1 in the active rTMS group but not the sham rTMS group.
In a final exploratory analysis, the authors asked whether rTMS’s effects on “general depressive” symptoms were mediated by rTMS effects on the distributed network of connectivity linked to these symptoms in the first analysis. These results were tantalizing but complex. The “brain score” derived from connectivity in this LV1 network varies considerably within individuals over time under sham conditions, and it is unclear whether active rTMS affected these natural fluctuations. This fluctuation over time was not linked to symptom change in the sham rTMS group. In the active rTMS group, change in brain score was linked to antidepressant effect in a complex manner: Increase in brain score in this network was linked to a weak antidepressant effect, stable brain score was associated with a moderate antidepressant effect, and reduction in brain score was linked to higher antidepressant effect. Although these findings do not lend themselves to easy interpretation, it is worth noting that rTMS in this trial was not targeting the brain network specifically linked to the “general depressive” symptoms of LV1. Future trials designed to specifically engage this network may reveal clearer brain–symptom relationships.
The results of this study support the authors’ argument for a larger trial of rTMS for depression in schizophrenia. It is worth noting that the individuals in the trial presented here were not selected for depression severity. The potential of rTMS to alleviate depressive symptoms in schizophrenia may be even more impressive than the already compelling data presented here. Ideally, a larger trial would include individuals selected for significant depression at the start of the trial, so that we could understand the full potential of rTMS as an intervention in this population.
As clinicians, this would be a welcome development. The observation of an antidepressant effect for rTMS focused on the DLPFC is very encouraging given the concern that antidepressant medication interventions may be of limited use in this population (
2). The need for novel interventions is made glaringly clear as the range of antidepressant options available to individuals without psychotic disorders (e.g., ketamine [
7] and psilocybin [
8]) grows rapidly.
More broadly, the Gallucci et al. study is a model effort in the ongoing quest to use neuroscience to guide therapeutic development for unmet clinical needs. Our enthusiasm is driven by two main factors, which we will briefly highlight here—the analytic approach used in the neuroimaging–symptom correlation and the evaluation of these relationships using neuromodulation techniques such as rTMS.
First, the analytic approach used here (PSLC) is well positioned to bridge the gap between two relatively isolated approaches: 1) pen-and-paper instruments with decades of refinement and validation in the clinic, and 2) neuroimaging that is rapidly developing the tools needed at the personalized scale needed in the clinic (
9). It seems certain that constructs such as a CDSS scale and resting-state connectivity will not map onto each other easily, and so approaches such as PSLC represent a promising path forward.
The second notable aspect is the attempted validation of imaging–symptom correlations identified by PSLC. The testing of the causality of these symptom–network relationships using neuromodulation, in this case rTMS, is critical for translation (
10). Even as the range of pharmacological and neuromodulation tools available continues to grow, the need for well-designed investigator-initiated controlled clinical trials will be a daunting challenge. The Gallucci et al. study is an elegant demonstration of how this can be accomplished when all of the intellectual, clinical, and structural resources required are marshaled for this purpose.