Depression among individuals who have been racially and ethnically minoritized in the United States can be vastly different from that seen in White Americans (
1). For example, African American adults with depression rate their symptoms as more severe, have a longer course of illness, and experience greater disability (
2,
3). In sum, the burden of depression appears to be higher among African Americans compared with White Americans (
2).
African American adults are less likely to receive depression treatment than are their White counterparts (
4,
5). These inequities are increasingly linked to social, economic, and environmental determinants such as low income, underresourced educational opportunities, inadequate housing, and lack of access to quality mental health treatment (
6–
9). Other contributors to this treatment gap include underdetection by providers (
10), unreliable medical systems (
11), and treatment settings perceived as punitive and inaccessible (
12–
14).
Frequency of suicidal thoughts and behaviors, which are often associated with depression, is increasing among African American youths. A study with a nationally representative sample of U.S. high school students found that from 1991 to 2017 African American adolescents experienced a 73% increase in suicide attempts, while the suicide attempt rate decreased 9% among White youths during the same period (
15). Further, the suicide death rate among Black children ages 5–12 years is increasing faster than among any other racial/ethnic group in the United States (
16,
17). Similar to those among adults, factors associated with the increase in depressive sequelae among African American youths are multifactorial (
18–
21). Although researchers have described how social determinants affect depression along the life course (
22), little attention has been paid to how structural racism and its consequences may contribute to the intergenerational transmission of depression.
The purpose of this review is to conceptualize how structural racism and cumulative trauma can be fundamental drivers of the intergenerational transmission of depression. We propose that understanding risk factors for depression, particularly its intergenerational reach, requires accounting for structural racism that is routinely experienced by racially and ethnically minoritized individuals (
23). In light of the profoundly different experiences of African Americans who are depressed (i.e., more persistent course of illness and greater disability) (
2), it is critical to examine whether intergenerational transmission of depression due to structural racism is an emerging explanation for some of these differences.
Structural Racism and Depression
For this review, we adopted Alvidrez and Tabor’s (
24) recent definition of structural racism: “Macro-level societal conditions that limit opportunities, resources, and well-being of less privileged groups on the basis of race/ethnicity and/or other statuses, including but not limited to, gender identity, sexual orientation, disability status, social class or socioeconomic status (SES), religion, geographic residence, national origin, immigration status, limited English proficiency, physical characteristics, or health conditions.”
It is vital to note that structural racism as defined by Alvidrez and Tabor affects many populations (e.g., LGBTQ populations, American Indians, Latinx, women, and people with low income). A focus on structural racism lends itself to an analysis of how policies and systems affect specific groups and suggests topics on which to intervene (
9,
25). Structural racism is evidenced by limited access to opportunities through macrolevel systems, including health care, criminal justice, housing, education, employment, and income. These systems give White people an unjust amount of value, resources, rights, and power while simultaneously dehumanizing and devaluing the privileges of communities of color and other marginalized populations (
24,
26).
Our focus on structural racism does not minimize the deleterious impact of personally mediated racial discrimination (e.g., hate crimes, being followed in a store because of a suspicion that one may steal) or internalized racial inferiority (e.g., self-devaluation, hopelessness, and an embracing of “Whiteness”) (
27). Indeed, there is a robust evidence base demonstrating the negative mental and physical health impacts of racial discrimination and internalized racial inferiority (
28–
31). Rather, we aim to emphasize how cumulative trauma due to structural racism may contribute to the intergenerational transmission of depression.
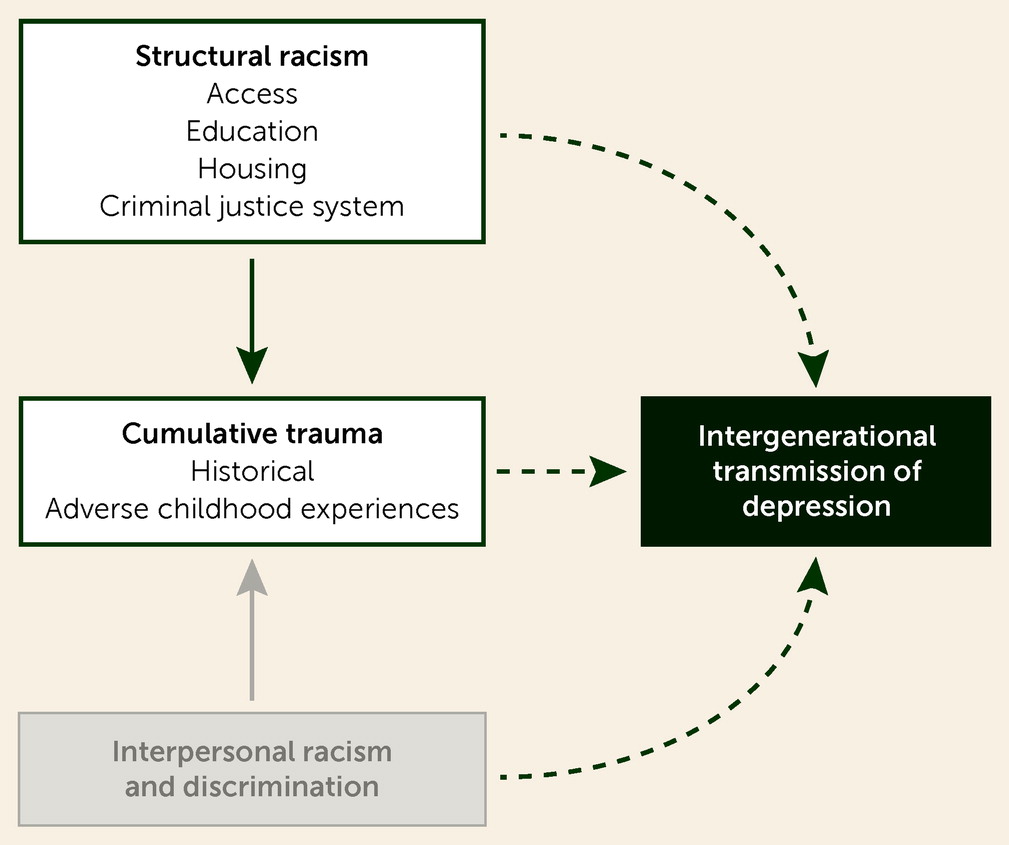
Figure 1 shows our conceptualization of the relationship among structural racism, cumulative trauma, and transmission of depression across generations.
Cumulative Trauma and Depression
Cumulative trauma is a term that is used to explain syndromes that result from repeated injury or are aggravated by repetitive insults. Examples in medicine are carpal tunnel syndrome, low back pain, or tennis elbow (
32). Similarly, cumulative psychological consequences likely result from traumatic experiences. The frequency, severity, duration, and timing of these traumatic exposures are positively correlated with severity of health outcomes, including depression. The effects of these outcomes are even more devastating when there is betrayal, when a trusted person such as a parent or close friend betrays the trust of the victim and inflicts harm (
33). Traumatic experiences stemming directly from structural racism represent the failure of a trusted entity (institutions, society, or the government) to protect one from harm.
Related to cumulative trauma is the idea of “historical trauma,” which refers to intergenerational trauma experienced by a group of individuals who have been systematically oppressed in previous generations (
34). Historical trauma theory postulates that the psychological and emotional consequences of mass traumatic experiences can be transmitted to subsequent generations through physiological, environmental, and social pathways (
25,
34). This transmission results in an intergenerational cycle of trauma response, including general medical (e.g., compromised immune system, endocrine impairment, and adrenal maladaptation), social (e.g., domestic violence, child maltreatment, substance abuse, and involvement in crime), and psychological (e.g., depression, panic or anxiety disorders, and posttraumatic stress disorder [PTSD]) (
25,
35). Other psychological mechanisms include people’s beliefs (i.e., cognitive factors) that are transmitted across generations. For example, children may be socialized within their families and schools to perceive racially minoritized groups as deficient (
36).
The concept of intergenerational trauma was introduced into the psychiatric literature through descriptions of behavioral and clinical problems in offspring of Holocaust survivors (
37). Subsequently, discussions have ensued about the impact of historical events such as colonization, slavery, and displacement trauma in many cultures, including First Nations and Native American communities (
38), African Americans (
39,
40), Australian Aboriginal people (
41), and Maori people of New Zealand (
42). Intergenerational trauma has also been studied in societies exposed to genocide, ethnic cleansing, or war, such as people of Cambodian (
43), Armenian (
44), Rwandan (
45), and Palestinian (
46) descent. The data are even scarcer among those experiencing both, yet distinct, well-documented cumulative and historical traumata—sexual minority groups among racial/ethnic minority populations (
47).
Adverse childhood experiences (ACEs) refer to adverse events experienced by children younger than 18 years (
48). Early studies defined ACEs as emotional, physical, or sexual abuse; emotional and physical neglect; witnessing violence against the mother; parental separation or divorce; and living with household members who were ever incarcerated, had mental illness or were suicidal, or misused substances (
48,
49). Expanded ACEs studies also include experiences of racism, bullying, low neighborhood safety, community violence, and living in foster care as additional forms of childhood trauma (
50). Numerous ACEs studies have documented a strong, graded dose-response relationship among the number of ACEs; individuals with four or more ACEs have been found to be at highest risk for or have experienced negative health, social, or behavioral outcomes in adulthood (
51). Furthermore, a longstanding body of evidence indicates that childhood exposure to intimate partner violence and other forms of abuse is positively correlated with perpetration of various forms of violence during the life course (
52).
Numerous studies have shown the long-term negative impact of childhood adversity and maltreatment on increased risk for depression across the lifespan (
53–
55). The rates of childhood adversity, poor parental bonding, and family instability are clustered among parents with depression (
56). The literature is replete with studies documenting the adverse and cumulative effects of interpersonal trauma on a person’s psychological well-being (
57–
59). Left untreated, the outcomes of these traumatic stressors and violent episodes include enduring cognitive and physiological consequences, including depression (
60).
Intergenerational Transmission of Depression
Results from numerous studies from the United States and other countries indicate that the offspring of depressed parents are at increased risk for developing depression and other adverse clinical outcomes (
61–
67). Transmission of depression from parent to child may begin early, even in utero. New studies of the offspring of depressed mothers are increasingly focused on the pregnancy itself and on the effects of maternal depression on the offspring during pregnancy, delivery, and postpartum (
68,
69). These studies show that a mother’s experience of depressive episodes is associated with premature delivery, low birth weight, and atypical adjustment, which can lead to a greater risk for adjustment problems as the child matures (
70,
71).
Of great relevance to African Americans and other marginalized groups is the notion that depression risk among those directly affected by structural racism and cumulative trauma may extend to their descendants. The following vignette is based on a real patient named “Barbara.” Some details have been modified with the patient’s consent to protect patient confidentiality. The case describes how structural racism and cumulative trauma affected the intergenerational transmission and illness course of depression in an African American family.
Clinical Case History
Barbara is a 64-year-old African American woman who is an adjunct professor and lives in a large urban city in the northeastern United States. She has a psychiatric history of depression and PTSD. Her family history has significant prevalence of both depression and trauma. Barbara’s mother was diagnosed as having depression and had multiple depressive episodes during Barbara’s childhood. She remembers that her mother developed certain patterns and behaviors when she was depressed, the most prominent of which were social isolation (e.g., not wanting to go out or see friends), sleep problems, missing many days from work, and filing for disability at an early age. Despite acknowledging that she was depressed, Barbara’s mother never sought treatment for her illness stating, “The only thing psychiatrists do for us [African Americans] is lock us up in the hospital. I’ll handle this by myself.”
Barbara’s father was born in a town in the Deep South. On two separate occasions, he woke up to see a cross burning on his front yard. His family migrated to a large northern, urban city shortly after Emmett Till was murdered because his mother was terrified that her son’s life would be in danger as he got older. Several years after graduating from high school, Barbara’s father and mother got married. The father sought full-time jobs but was denied multiple vocational opportunities because of a “lack of experience.” After he found work and saved enough money to move to his desired neighborhood, the family was denied an apartment because the neighborhood did not rent to African Americans. Barbara’s father mentioned on multiple occasions that the family tried to rent an apartment but was never given a reason why their application was denied. In 1974, he was arrested when Barbara was an adolescent and sentenced to 15 years in prison for possession of marijuana. Although this was his first criminal offense, he was incarcerated for 8 years of his 15-year sentence.
Barbara experienced a range of ACEs before having her first depressive episode as a young adult: her mother had depression, her father was incarcerated when she was 17 years old, and she was a survivor of physical and sexual abuse from a close male relative. Barbara was also bullied by White students at school when they discovered that her father had been incarcerated.
To this day, Barbara experiences recurrent depressive episodes and PTSD symptoms, most notably hypervigilance. Her symptoms are exacerbated by present-day events, such as the murder of George Floyd in 2020, that remind her of the historical traumatic events to which her family was exposed. Furthermore, she has attributed persistence of her depressive symptoms to challenges navigating the health care system, mistreatment by mental health care providers, and lack of access to affordable, high-quality treatment. Protective factors she cites include spirituality, a strong social network of friends, and engagement with a trauma-informed psychiatrist and therapist. Breaking the familial cycle of depression illustrated in Barbara’s case must involve directly addressing the structural barriers she and her father and mother experienced.
Recommendations to Disrupt Structural Racism
Advocate for Antiracist Policies
Morsy and Rothstein (
72) note that social class, income, and race can contribute to toxic stress, which can lead to behavioral problems and depression. The authors recommend improving support (i.e., home visits or therapy services by community health workers or other specialists) to promote protective parenting, improving training of school staff to support children, addressing racially disparate policies and practices in schools (i.e., inequitable discipline policies that can induce stress), and training health care professionals in screening and treatment for stressful experiences such as trauma (
73). Public policies that address inequities in social determinants of health (e.g., education, housing, employment, and food insecurity) that are rooted in structural racism are also needed.
Similarly, the mass incarceration of African American men has been well documented (
74). Barbara’s father was a victim of excessively harsh drug laws in the 1970s that gave a minimum of 15 years to life in prison to people charged with possession of illicit substances (
75,
76). Policies that promote criminal justice reform hold great promise for disrupting the cycle of intergenerational trauma (
77). Any one of these policies may have improved Barbara’s quality of life and the trajectory of her depression.
Address Societal Attitudes and Biases
It is critical that we adequately address conscious and unconscious biases throughout society. Providing inclusive and complete histories about minoritized groups within our educational system—beginning in children’s formative years—is a meaningful first step to disrupting the cross-generational transmission of deficit-based beliefs about minoritized groups. Meaningful change must be comprehensive, coordinated, and multitiered. Rigorously testing the impact of these strategies will be crucial to assess the utility of their widespread dissemination.
Conduct Longitudinal Studies With Racially Diverse Samples
Intergenerational questions require intergenerational study designs. Until intergenerational cohorts of groups exposed to structural racism become more readily accessible, questions about the intergenerational ramifications of racism and trauma will remain unanswered. To date, most longitudinal studies have been conducted with mostly White subjects.
A notable exception is the Boricua Youth Study (BYS)—a longitudinal, population-based sample of Puerto Rican children and adolescents in two separate locations: the South Bronx, New York, and the San Juan–Caguas metropolitan area, Puerto Rico. Importantly, the BYS is the only study to date to examine developmental psychopathology among children of the same ethnic group living in two highly disadvantaged contexts in the United States. Although in both contexts children are disproportionately exposed to structural racism, Puerto Rican children residing in the South Bronx have the additional experience of being an ethnically minoritized group. For the past 20 years, it therefore has been possible to examine how the experience of being part of an ethnically minoritized group—which putatively results in increased exposure to racism, discrimination, acculturation, and cultural stress (
78,
79)—shapes risk for psychopathology differently for Puerto Rican children residing outside of the archipelago.
The BYS has consistently documented higher prevalence of several psychiatric disorders among children residing in the South Bronx. Notably, although the risk and resiliency factors to developing psychopathology have been similar across both contexts, risk factors (including cultural stress and discrimination) were more frequently present in the South Bronx. In fact, the results of our studies have shown that even when controlling for sociodemographic factors and stressful life events, cultural stress (
79,
80) still strongly predicts psychopathology among children. Further, findings from the most recent wave of data collection (
78) suggest that the intersecting contexts of minoritized participants might be particularly important for understanding risk for depression.
“Coproduce” Clinical Interventions and Research
A growing body of evidence has shown that policy makers, clinicians, and researchers need to coproduce research and interventions (e.g., programs, services, and policies) in collaboration with people of color instead of coming up with “top down” solutions (
81). Community-Partnered Participatory Research (CPPR) is one of many community engagement strategies that fosters collaborations among community members, researchers, and clinicians (
82). CPPR emphasizes two-way sharing of knowledge, respect for diversity, and equity (
83). Community-partnered approaches enable shared power among stakeholders, increase trust within marginalized communities (previously subjected to unethical institution-led research such as the Tuskegee Syphilis Study), and reduce mental health disparities (
82,
84).
Culturally Tailor Depression Interventions for Males of Color
The aforementioned BYS documented unusually high rates of depression among males at both study sites, so much so that the expected sex differences in depression rates were not observed. It may be that a lack of opportunities, high poverty, and lack of social mobility present in both contexts may have interacted with cultural gender norms and may have generated frustration among young men who may have felt that they were inadequate providers for their families. Because racial and ethnic minority groups are more likely to reside in underserved communities, our findings highlight how multiple intersecting factors, including manifestations of structural racism and poverty, shape depression risk across the life course.
Intersectionality theory, rooted in feminist approaches and Critical Race Theory, posits that social identities involve complex intersections of individuals’ lived experiences nested within systems of oppression (
85,
86). We propose the use of intersectionality to adapt depression interventions for men of color, whose socially constructed identity categorizations (i.e., race), experiences (e.g., depression or criminal justice involvement), and impact of their gender lead to perceived racial discrimination and utilization of mental health services (
87). Given the rising rates of suicidality among Black boys, culturally tailoring of depression interventions to this group is a pressing clinical and public health need. Conversely, we should be wary about overdeveloping culturally based solutions. Such approaches may suggest inherent defects within marginalized or stigmatized populations and could inadvertently support the notion that Whiteness equates to perfection. Intersectionality may also guide the development of a more diverse workforce to deliver mental health interventions to and in marginalized communities.
Conclusions
We assert that structural racism and cumulative trauma are fundamental drivers of the intergenerational transmission of depression. The clinical vignette used in this review highlights the ways in which structural racism (e.g., familial housing discrimination and lack of access to mental health treatment) and cumulative trauma (e.g., exposure to hate crimes via cross burnings, parental incarceration, and ACEs) interact to influence the intergenerational transmission of depression. Action should be directed toward policies that dismantle structurally racist institutions and practices; improve protective systems, including a mental health care system that is equitable, of high quality, and accessible; and generate knowledge to understand the intergenerational course of depression among historically racially and ethnically minoritized families.
Acknowledgments
The authors acknowledge the work of Drs. Chester Pierce, Camara Jones, and David Williams, among others, whose conceptualization of racism led to groundbreaking empirical studies that have highlighted the deleterious impact of racism on mental health.