Introduction
In the United States in 2012 about 1.64 million cases of cancer were diagnosed, with about 577,000 deaths (1). The most common nonskin malignancies are lung, colorectal, breast, and prostate cancer. The last 40 years have seen dramatic increases in the 5-year average cancer survival rate from about 50% to now about 67% (1). This progress reflects remarkable advances in population cancer risk reduction initiatives, cancer screening programs and technology leading to earlier diagnosis, and in the active treatment modalities of oncologic surgery, radiation therapy, chemotherapy, hormonal therapy, biotherapies, and more recently targeted therapies. Advanced imaging technologies and tumor biomarker measurement now play important roles in therapy selection and tracking of response to therapeutic interventions. There remains very large variability in cancer patient response to treatment and in survival outcomes based on tumor type, tumor pathological and cytogenetic features, stage at diagnosis, race, and income level. Cancer genetic testing has become an important tool in determining personal genetic risk for some cancers (e.g., members of families with extensive breast and/or ovarian cancer history) which may result in individualized cancer risk reduction interventions (
2).
As of January 2012 there were 13.7 million U.S. cancer survivors (defined as individuals previously diagnosed with cancer) (
3). As the U.S. population ages, it is anticipated there will be significant increases in the incidence and prevalence of cancer, with the number of cancer survivors expected to grow to 18 million by 2022 (
3). This growth will significantly challenge our U.S. cancer care delivery system (
4,
5).
Historical Perspective/Current Services Delivery Landscape
The last 40 years has encompassed marked advancements in our understanding of the complexity of the human aspects of cancer care (
6).
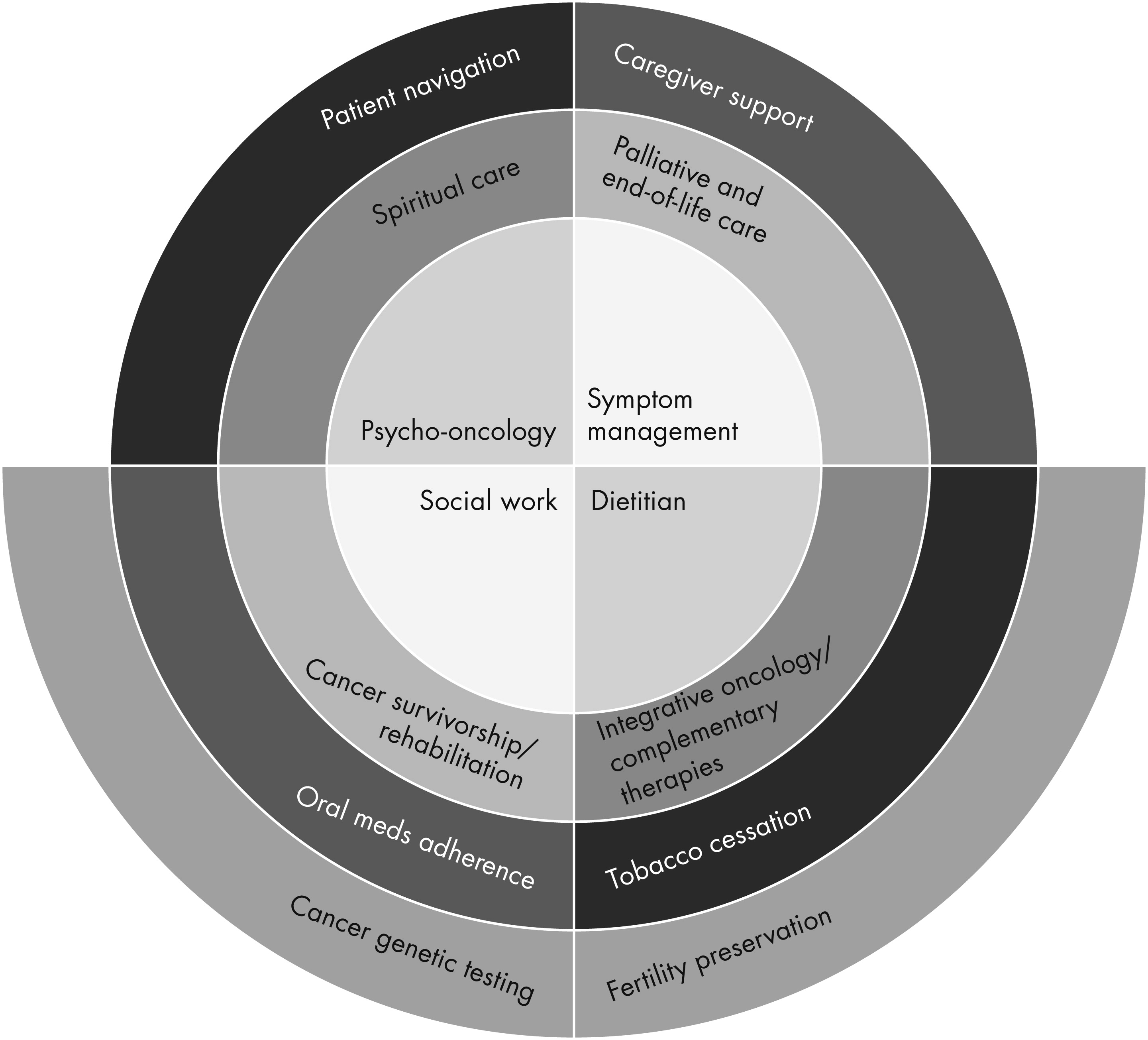
Figure 1 presents one model of the broad range of services included in supportive oncology services. For almost all of the
Figure 1 services there now exist national quality of care standards.
Modern hospital cancer program supportive oncology services are based on the fully integrated multidisciplinary team collaborative care model. The team may include social workers, dietitians, patient navigators, oncology nurses with educational and specialized clinical expertise (e.g., cancer pain management nurses), psychiatrists, psychologists, spiritual care providers, cancer rehabilitation medicine and survivorship services providers, integrative oncology care providers (e.g., acupuncturists, mind-body therapists), and palliative care providers. Integrated supportive oncology teams need to be fully embedded in the hospital cancer program’s cancer care delivery system at the clinical care delivery, quality improvement, and hospital organizational structure levels (such as the Cancer Committee). They need to ensure supportive oncology patient care continuity as patients move between hospital cancer program inpatient and ambulatory, community/facility, and home health and hospice care environments.
National cancer patient/family/caregiver educational and supportive care services provider and advocacy organizations form a very important component of the supportive oncology care system (
Table 1) (
7). In larger cities there are often local/regional community supportive oncology providers (e.g., Cancer Support Community, WeSpark in Los Angeles). A relatively small number of private practitioners provide psychiatric, psychological, and/or social work services to cancer patients.
For patients approaching the end of life, home health agency and hospice services providers become critically important components of their personal supportive oncology services delivery system. Given the differing hospital cancer program and hospice financing systems, maintaining supportive oncology care continuity as hospital cancer program patients transition to prehospice or hospice care is a major challenge.
Many U.S. cancer patients receive some or most of their cancer care in the physician office or free-standing cancer treatment facility environment. The provision of excellent, comprehensive, and accessible supportive oncology care to all U.S. cancer patients in all treatment environments throughout their illness is a serious challenge.
Many informational and educational/support group services to cancer patients and their family members are now available on the web, via social media, or by using telecommunications technology (
Table 1) (
8). In spite of the diversity of this supportive oncology services delivery system, many U.S. cancer patients and their family members do not have timely access to the supportive oncology services they want and need (
9).
As we look to the future impact of health care reform on models for the provision of supportive oncology to cancer patients, we can build on the cancer-specific application of current best-practice models for the role of psychiatry in collaborative care of patients with chronic medical diseases (
10).
Provision of Clinical Psychiatric and Psychological Services to Cancer Patients
Psychiatric Assessment and Care of Cancer Patients
The epidemiology of psychological distress and psychiatric disorders in cancer patients was one of the first areas of systematic research in psycho-oncology. Clinically important psychological concepts include stress/trauma and distress, individual coping strengths and resources, social and family support, the patient’s life cycle phase, medical and psychosocial illness phases, resilience and posttraumatic growth, loss and grief, existential and spiritual dimensions of the patient’s cancer care experience, and caregiver support and stresses. The financial and vocational/social role function impacts of cancer and its treatment often profoundly adversely affect the patient and his/her family members (
4,
11).
Routine, early post-diagnosis patient distress screening and multidisciplinary supportive oncology team clinical assessment and triage are critical to the provision of optimal supportive oncology care. Interventions include the provision of individualized cancer and cancer treatment education, access to educational and support groups, individual supportive psychotherapy, CBT, and existential/meaning and dignity therapies. Other often personally important services include spiritual care, mind/body stress management training, and exercise/physical therapy/rehabilitation services (
12,
13)
In smaller communities that have small hospital cancer programs, the psychiatrist may often be a privative practitioner who performs inpatient consultations and sees cancer outpatients in a private practice model. In larger hospital cancer programs, the psychiatrist may receive salary support to provide direct clinical services and clinical and administrative leadership to the supportive oncology service.
Core Psychiatric Oncologist Clinical Services Role
Fundamentally based on core psychiatric and psychosomatic medicine specialty skills, the psychiatric oncologist provides psychiatric diagnostic and pharmacological management services to cancer patients with confusional states and delirium, depression, anxiety, substance abuse disorders, and insomnia. Cancer patients may also present with significant character pathology that may interfere with successful cancer treatment unless psychiatrically managed. Psychiatrist, psychologist, and social worker team members can closely collaborate in the assessment and care of these patients.in the inpatient and ambulatory cancer center settings (
14–
21).
The clinical judgment concerning the discrimination between normal (if intense) levels of situational distress and symptoms and diagnosable psychiatric disorder remains an often difficult challenge. These judgments can be aided by the use of validated scales such as the PHQ-9 and the MDFI 20.
The related clinical judgments concerning the use of psychopharmacologic agents in the management of symptoms of anxiety, depression, and insomnia are often complicated by the potential neuropsychiatric toxicity of a wide variety of oncologic active treatment medications and of radiation therapy. The potential for adverse psychopharmacologic drug interactions with oncologic agents and for adverse drug/disease interactions is an ongoing concern for psychiatrists prescribing to cancer patients (
22–
27). For example paroxetine and other antidepressant medications, which interfere with the hepatic metabolism of tamoxifen to endoxifen, may adversely impact the risk of disease recurrence in breast cancer patients (
18).
The psychiatrist also needs familiarity with a wide variety of clinically important neuropsychiatric disorders associated with cancer and its treatment. These neuropsychiatric disorders include the posterior reversible encephalopathy syndrome (PRES) and CNS paraneoplastic syndromes as well as neuropsychiatric disorders induced by oncologic agents, corticosteroids, and immunosuppressant agents. The psychiatrist also needs familiarity with side effects of medications used to treat pain or other symptoms as well as the consequences of primary or metastatic brain tumors or acute or chronic organ failure in association with advanced disease/failure to thrive/performance status decline, specifically at the end of life (16, 23, 28–31). The neuropsychiatric impacts of the newer generation of “targeted agents” and hormonal treatments are still incompletely understood. Extended Psychiatric Oncologist Role in Cancer Patient Physical Symptom Management
A host of physical symptoms may be associated with cancer and its treatment, particularly at later disease stages. Pain and fatigue are especially common and often debilitating, and unless effectively treated can greatly contribute to anxiety, depression, and insomnia. The psycho-oncologist psychiatrist would ideally develop significant expertise in the assessment and pharmacologic management of cancer pain (
32–
34), fatigue (
35), decreased appetite with weight loss/cachexia (
36), hot flashes (
37,
38), chemotherapy-induced peripheral neuropathy (
31), and the cognitive impairments associated with cancer treatment including chemotherapy (“chemobrain”) (
11,
39–
41).
While not common, there are psychiatric oncologists who have significant expertise in the clinical assessment and pharmacologic management of cancer pain and who provide cancer pain management services. The Samuel Oschin Cancer Center at the Cedars-Sinai Medical Center (CSMC) has had a psychiatrist-led cancer pain management service for about 22 years (
42). The current psychiatrist and cancer rehabilitation medicine specialist provide cancer pain management physician services to Cancer Center patients upon referral of the patient’s primary oncologist physician, including opiate and adjunctive medication management. This care is supported by dedicated service nurses who have cancer pain management expertise. The physicians have access to Cancer Center examination rooms and infusion center spaces, provide 24/7 physician coverage, and provide limited cancer pain management services to Cancer Center inpatients. The service closely collaborates with the inpatient CSMC Palliative Care Service, which provides most of the inpatient cancer pain/symptom management care. CSMC also has inpatient and outpatient anesthesiologist-led interventional and peri-operative pain management services. Thus, in close collaboration with other institutional pain and symptom management physicians and services the psychiatrist with cancer pain management expertise can play an important role in noninterventional cancer pain management care. Given the often marked clinical overlap between cancer pain, psychological distress, and psychiatric symptoms, this extended role of the psychiatrist can be very helpful in optimizing psychiatric care.
Psycho-Oncologist Psychiatrist Role in Provision of Comprehensive Supportive Oncology Care
The psycho-oncologist psychiatrist ideally works closely with a multidisciplinary supportive oncology team including the full range of supportive oncology providers. As one example the Samuel Oschin Cancer Center at the Cedars-Sinai Medical Center treats about 10,000 patients/year with about 120,000 patient visits. For this population the Oncology Supportive Care Service has one full-time psychiatrist, one full-time cancer rehabilitation medicine specialist, six full-time oncology social workers, three full-time oncology dietitians, two full-time cancer pain management service nurses, and one full-time dedicated chaplain plus administrative support staff. The psychiatrist commonly sees new consults and patients with complex follow-up care needs with the social worker and/or nurse. This team meets briefly each workday morning for a patient review/planning “huddle” and has a weekly extended patient review and care planning meeting. Each dietitian and social worker is assigned to a specific group of oncology practices to optimize continuity of care and typically participates in specific oncology practice or service meetings. Social workers and dietitians are actively involved in a variety of patient education/support groups and wellness/cancer survivorship services. Service handoffs are routine when patients are admitted to or discharged from the inpatient setting. The Service closely follows patients with advanced disease, manages outpatient hospice referrals, and seeks to ensure optimal supportive oncology care continuity for Cancer Center patients referred to hospice. The Service leadership team meets weekly.
The organizational principles of this collaboration are more fully articulated below in the section on the City of Hope Oncology Supportive Care Medicine Service. Fann has reported a model for the collaborative mental health care of cancer patients, which may be especially important in the context of health care reform and the future “oncology accountable care organization” (
10).
Psycho-Oncologist Psychiatrist Roles in Palliative and End-of-Life Care
The recent Institute of Medicine (IOM) report on delivering high-quality cancer care has outlined five principles of cancer patient care from diagnosis onward: care planning, palliative care, psychosocial support, prevention and management of long-term and late effects, and family/caregiver support (
43). Hospice and palliative medicine physicians have long provided medical leadership to hospice services. Hospice and palliative medicine physicians are increasingly leading not only inpatient palliative care consultation services and inpatient palliative care or hospice units but also leading outpatient palliative care/supportive care medicine clinics.
There is increasing recognition of the importance of the role of psychiatry, behavioral healthcare, and spiritual care services in the care of patients at the end of life. The reader is directed to key chapters and books and multiple recent articles that articulate the scope of the clinical services needs of this population, principles of the clinical assessment and management of psychological distress and psychiatric disorders in this population, and potential roles of psychiatry in palliative care and hospice services delivery (
44–
62). Many opportunities exist for closer collaboration between psychiatric oncologists/supportive oncology services with palliative care and hospice services to enhance hospital cancer program end-of-life patient care and family/caregiver support. Hopefully future changes in the structure of hospice care and hospice reimbursement will facilitate a broader role for psychiatric oncologist/supportive oncology service in cancer patient hospice care delivery.
Two especially important therapeutic advances concerning the psychosocial care of patients at the end of life include dignity therapy and existential therapy (63–66). One recent major study found that early provision of comprehensive palliative care services to patients with advanced lung cancer resulted in extended duration of life as well as improved distress/quality of life (67, 68). Other Major Supportive Oncology Clinical Services Challenges
Many cancer patients utilize a wide variety of complementary therapies in their personal approach to fighting cancer. While mind-body therapies may bring great psychological value, there is concern that ingestion of certain natural substances (supplements, herbs) with antioxidant effects could interfere with the antitumor effectiveness of chemotherapy and/or radiotherapy treatments. The psychiatrist working in the cancer treatment setting needs to be aware of this literature (
69–
72). Several cancer quality of care standards organizations have set standards that tobacco use should be assessed in cancer patients and that those using tobacco should be offered a cessation intervention program. All hospital cancer programs should offer onsite or by referral tobacco cessation services to their cancer patients who use tobacco (
73–
75).
Certain chemotherapy agents and many of the newer targeted agents are oral, self-administered medications. Studies have indicated that adherence rates for women with breast cancer on chronic oral hormonal treatments (tamoxifen, aromatase inhibitors) decline quite significantly over the first 3–4 years of treatment (
76–
78). This finding will likely apply to other chronic oral therapies (
79). One of the major challenges for supportive oncology is developing effective mechanisms for determining patients’ risk for nonadherence to oral regimens, and implementing effective educational and adherence support programs to optimize patient adherence to these regimens.
There exist many challenges in implementing sustainable financing/business models for the provision of psychiatric oncology/supportive oncology services in the hospital cancer program environment. Given the current reimbursement environment, these services are not financially self-sustaining and require hospital financial support. The senior author for many years led the corporate development of comprehensive hospital ambulatory cancer center supportive oncology services at multiple hospital sites throughout the United States. In general, the total net costs of providing supportive oncology services ranged between 1.5%−2.5% of net Cancer Center operating revenues. The current business rationale for hospital financial support for these services includes contribution to patient care quality and patient service satisfaction, meeting national supportive oncology care quality standards, contributing to optimal patient treatment adherence, contributing to oncologist physician/nurse/patient visit productivity, and the ability to attract private philanthropy to support certain elements of supportive oncology services.
Particularly in collaboration with inpatient and outpatient palliative care services, supportive oncology services can contribute to optimizing patient end-of-life care, decreasing avoidable utilization of hospital emergency department and inpatient/ICU resources for cancer patients at the end of life, and supporting earlier referrals of patients with advanced disease to hospice from the ambulatory cancer center setting.
In the future, as we move toward the potential “oncology accountable care organization” (away from the current fee-for-service model to the bundled care reimbursement model), and as cost minimization becomes a more important component of hospital cancer program financial sustainability, it is likely that the role of supportive oncology services will become more highly valued.
Cancer Survivorship and Rehabilitation Services
The creation of cancer active treatment summaries and cancer survivorship care plans for cancer patients completing initial active cancer treatment is a standard for hospital cancer programs established by the American College of Surgeons Commission on Cancer (ACoS CoC) as of January 2015. Cancer survivors face many ongoing cancer recurrence prevention, physical/rehabilitation, financial/vocational function, symptom management, psychosocial, and physical and mental health quality of life challenges. Providing effective, timely, accessible, affordable, and sustainable supportive oncology services to cancer survivors is another major challenge to the U.S. cancer care delivery system (
4,
5,
80,
81).
Some cancer patients develop personally significant deterioration in often higher executive cognitive functions due to the neuropsychiatric toxicity of cancer medications and possibly radiation therapy. The concept of “chemo brain” has definitely entered the consciousness and vocabulary of many cancer patients. Clinical experience suggests that neurocognitive rehabilitation programs and in some cases psychopharmacologic treatments can be therapeutically helpful (
5,
39–
41).
Cancer rehabilitation medicine services provide great value to hospital cancer programs whether as an organizationally separate service or as an integrated component of a supportive oncology service. Clinically safe, oncologist physician-sanctioned physical exercise programs/physical therapy programs provide important rehabilitation and fatigue management value to many cancer patients at varying disease stages.
Major Informational/Educational Resources Available to the Psychiatrist or Psychologist Working with Cancer Patients
This section presents some of the important professional organization, textbook, and journal resources valuable to the clinical psychiatrist or psychologist working with cancer patients. The major organizations and resources include the American Psychosocial Oncology Society, Association of Oncology Social Workers, and the Center to Advance Palliative Care. A second textbook on psycho-oncology has recently been published (
82). The major journals include
Psycho-Oncology,
Journal of Psychosocial Oncology,
Palliative and Supportive Care,
Journal of Cancer Survivorship: Research and Practice,
Journal of Pain and Symptom Management, and the
Journal of Palliative Medicine.Organizational Structure of Supportive Oncology
For a comprehensive discussion of creating oncology supportive care programs please see the work of Loscalzo and colleagues (
83,
84). The Department of Supportive Care Medicine at the City of Hope is a nationally leading model of a fully integrated multidisciplinary department with the capability of sharing a specific departmental vision/mission, supporting a high level of internal care delivery integration, and supporting comprehensive patient-centered care provided by a large, NCI-designated comprehensive cancer center. This single departmental model can also support optimal health care professional education and productive collaborative research activities. While other successful models exist for the organizational structure of supportive oncology in large academic cancer centers, the fully integrated single departmental model for supportive oncology services appears to hold the most promise for providing high-value supportive oncology care.
For smaller hospital cancer programs with smaller supportive oncology services, the principle of close psychiatrist collaboration with oncology social workers, dietitians, and psychologists can be highly effective. Close collaboration with local regional supportive oncology community service provider organizations, and helping guide patients to national educational and supportive oncology services providers (
Table 1) is especially important in the small hospital cancer program environment.
Biopsychosocial Screening: Distress is Never Enough
It is evident from the amount of professional publications that distress screening is of great interest. The influential 2008 IOM Report and subsequent key articles have demonstrated benefits, shared effective implementation strategies, and have been well described elsewhere (
83–
86). The focus of this section will be to extend the original implications of distress screening (which is now seen as too limited) within the realities of cancer care (
84,
85). The Distress Thermometer has been widely influential and is the instrument of choice wherever an automated tool is not available. Because it is paper based, it does not naturally link to specific professionals or to electronic health records, which is increasingly the standard for clinical care.
The more comprehensive automated biopsychosocial screening that is in place in a number of settings automates a series of processes that bring obvious increased institutional value (quality+cost): identification (physical symptoms, psychological problems, social concerns, spiritual challenges, practical barriers), requests (tailored education, resources, clinical trials), criteria driven triage to multispecialists, data storage (program development, research), and tailored reports. Biopsychosocial screening processes are achieved in real-time before or during the clinical encounter and are integrated with electronic medical records and tailored to specific populations (
85–
93). We can now turn to why biopsychosocial screening is strategically relevant to supportive care programs.
Comprehensive biopsychosocial screening supports the provision of timely comprehensive integrated biopsychosocial care, which thereby supports the ability of patients and their families to fully benefit from medical care, to cope effectively, and to make positive meaning of their experience. Comprehensive biopsychosocial screening also provides the opportunity for psychiatric leadership in the creation and implementation of institutional multidisciplinary psychosocial care triage and care algorithms. When done correctly, this process is much more than a set of mechanistic or operational processes to organize clinical care but rather enables open and honest communication about which professional is licensed and qualified to provide specific services. All too often these essential ongoing conversations do not happen because they are emotionally charged, and in general health care professionals are conflict aversive with each other. This is ironic given that the same health care professionals (including psychiatrists, psychologists, and social workers)—who may be highly skilled in end-of-life and other difficult communications—seldom create environments where these conversations can occur.
Ultimately, even highly trained professionals do not realize that conflict itself is not the problem–not managing the inherent conflicts that are endemic to team work is a serious problem that undermines quality of medical care, teamwork and patient safety (
84). Because effective biopsychosocial screening is dependent on coordination and communication among team members there is an opportunity and an acute need for leadership by psychiatrists.
Leveraging the System
Data are always necessary for successful programs but is never enough. Leadership and teamwork is always essential. Supportive care programs, even when integrated within standard cancer care, are frequently seen as both having value and competing for resources. In the present cost-cutting environment, supportive care is increasingly seen as a way to reduce costs, but administrators still struggle to understand the benefits of cost savings in a model that has traditionally focused solely on revenue.
Ultimately supportive care services have never had such a high profile and awareness of potential benefits that go well beyond the finances of a health care system in extremis. NCI Guidelines, NCCN Distress Management Guidelines, the recent IOM report (
43), increased emphasis on patient and family centered care, and consumer advocacy groups are all creating a more sustainable base of support for the importance for mental health interventions in cancer settings. Private philanthropy can also support innovative supportive care programs (the American Psychosocial Oncology Society’s website includes a robust video program on fund raising:
http://www.apos-society.org/professionals/meetings-ed/webcasts.aspx#2011).
In addition to the biopsychosocial screening and related service benefits for cancer settings, two additional ways that supportive care programs can leverage their influence is by partnering with patients, families, and local communities and pushing all professionals to the top of their licenses. When professionals practice at the top of their license (i.e., oncologists focusing on disease-directed care and not psychosocial problems for which they do not have the time or the training, or psychiatrists seeing patients who are depressed and not simply sad) there are resource efficiencies seen and potentially higher levels of provider and patient satisfaction.
Biopsychosocial screening instruments overall are able to rule-out depression in cancer patients (
87). There are major shortages of psychiatric oncologists in hospital cancer program settings. There are also shortages of community psychiatrists willing to see cancer patients, skilled in working with patients and their families affected by cancer, and able to take on people with poor health insurance and few financial resources. These realities make it essential that psychiatrists are used wisely in cancer patient care.
Supportive Oncology Clinical Quality Standards of Care
Efforts to promote greater awareness of the need for supportive care of cancer patients and its benefits received a major boost in 2008 with the publication of an IOM report titled, “Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs” (
94). The report summarized the considerable evidence about the deleterious effects of unmet psychosocial needs as well as the beneficial effects of providing psychosocial services. Among the report’s major conclusions was that, despite evidence of the effectiveness of supportive care services, many patients do not receive help for problems that would benefit from this type of care. To address this problem, the report included a list of recommended actions. The first and foremost recommendation is that all entities establishing or using standards for the quality of cancer care adopt a standard that calls for the provision of appropriate supportive care services.
To date, standards for supportive care have been put forward mostly by organizations and committees consisting of members of the supportive care community. Accordingly, there are concerns about the extent to which the wider community of oncology professionals is cognizant of these initiatives. Recent actions undertaken by the American College of Surgeons Commission on Cancer (ACoS CoC) bode well for the wider awareness and acceptance of standards for supportive care. The ACoS CoC is a consortium of 47 professional organizations that establishes cancer care standards and monitors quality of care at the more than 1,500 hospitals it accredits. In 2012, the ACoS CoC released several new standards for patient-centered care that will phase in for the 2015 accreditations (
95). Among the new standards is one which specifies that a local oversight committee develop and implement a process for psychosocial distress screening and referral for the provision of psychosocial care. The release of this guideline has generated considerable attention, including recommendations for how it should be met (
96,
97).
Clinical practice guidelines are more specific than standards and are meant to provide information that can be of assistance to health care providers in making evaluation, management, and treatment decisions. Numerous organizations have issued clinical practice guidelines that include recommendations for the supportive care of people with cancer. The National Comprehensive Cancer Network (NCCN) has been particularly active in this regard. Among other topics, NCCN has issued guidelines for the management of pain, emesis, anemia, fatigue, distress, and venous thromboembolic disease (
98).
Details about NCCN Guidelines for Distress Management are provided to illustrate the format and content. This NCCN guideline, updated annually since 1999 (
99,
100), consists primarily of recommendations that represent a uniform consensus among experts from NCCN member institutions; in general, they are based on lower-level evidence, such as clinical experience, as opposed to higher-level evidence, such as randomized controlled trials (RCTs). The guideline includes specific recommendations for psychosocial screening, evaluation, treatment and follow-up presented primarily in the form of clinical pathways. For example, recommendations for management of mood disorders (e.g. depression) specify that all patients should undergo brief psychosocial screening, with patients found to have moderate to severe distress referred to psychosocial care professionals. If patients are displaying signs and symptoms of a mood disorder, the initial recommendation is further evaluation, diagnostic studies, and modification of factors potentially contributing to the symptoms, such as concurrent medications and pain. Based on findings, subsequent recommendations may include initiation of psychotherapy and antidepressant medication, possibly in combination with anxiolytic medication. Consideration of referral to social work or chaplaincy services is also recommended before follow-up and reevaluation. A notable strength of these guidelines is the clear guidance they provide for the organization and delivery of psychosocial services given their clinical pathway format. A notable weakness is the limited use made of higher-level evidence to provide care recommendations. For example, the pathways regarding management of mood disorders do not include recommendations for use of specific forms of psychotherapy or pharmacotherapy even though there is a body of evidence on this topic for people with cancer (
101).
Moving forward, two considerations should guide future development of guidelines in this area. First, it is important to insure that procedures used to formulate and present guideline recommendations are consistent with recommended methods (
102). To address this issue, the quality of existing guidelines addressing supportive care should be evaluated using accepted methods such as the AGREE (Appraisal of Guidelines for Research & Evaluation) instrument (
103). The results are likely to suggest ways that existing guideline efforts in this area could be improved or could lead to the formation of new guideline efforts if improvements are not forthcoming. Second, greater effort needs to be devoted to embedding guidelines for supportive care into broader sets of cancer treatment guidelines. The Children’s Oncology Group Long-term Follow-up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers (
104) are a notable example of how consideration of the psychosocial dimension of care was melded into a comprehensive set of guidelines addressing late-effects of cancer treatment. Similar approaches should be considered in developing guidelines for adult-onset cancers, especially those for which supportive care issues are frequently encountered.