Several types of imaging evidence support the participation of both cortical and subcortical regions in performance of the clock-drawing task. An fMRI study in normal, healthy individuals performing a task that required drawing clock hands to indicate time found activations in both frontal and parietal regions (
Figure 2).
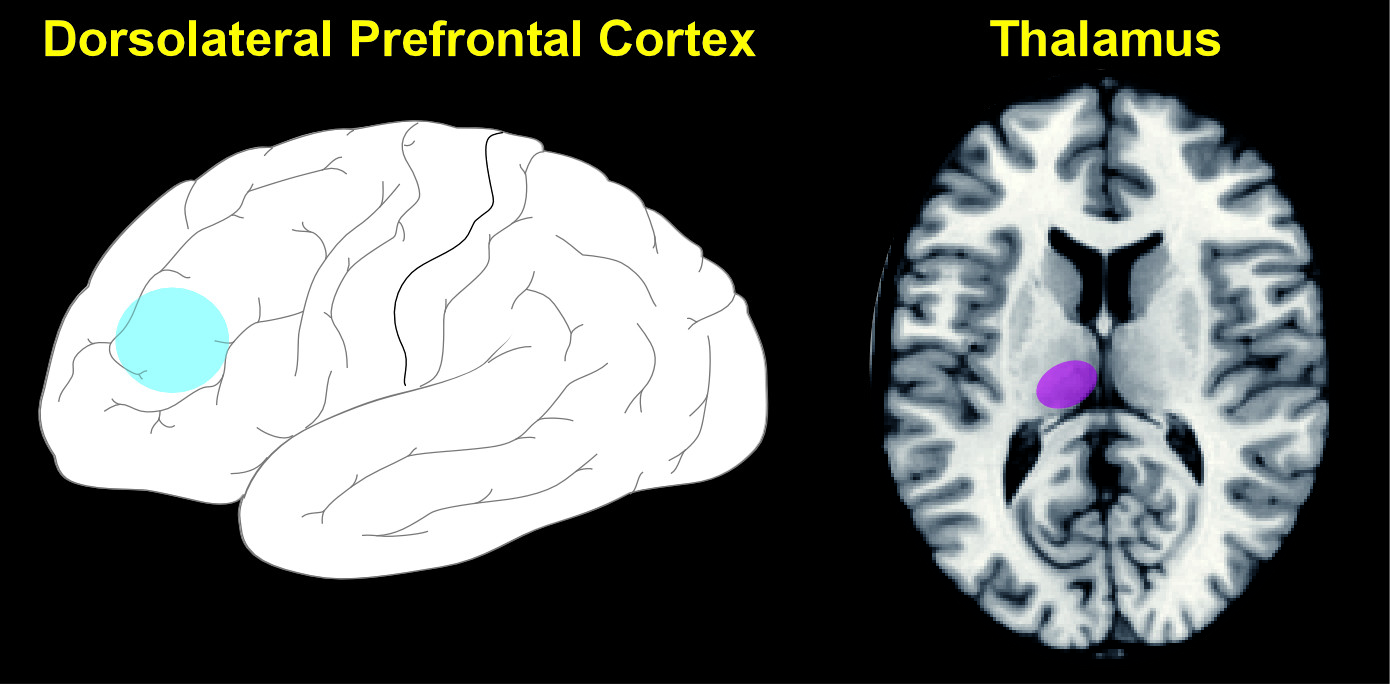
2 A study in patients with MCI, using resting-state fMRI to assess functional connectivity of dorsolateral prefrontal cortex (DLPFC), reported that connectivity to multiple brain regions (e.g., inferior parietal lobule, superior frontal gyrus, medial frontal gyrus, putamen) was reduced, but only the reduction in connectivity between left DLPFC and left thalamus correlated with performance impairment on the clock-drawing task (
Figure 3).
3 A study using voxel-based relaxometry to identify structural injury found that the clock-drawing task was more sensitive than several other commonly-used tests (e.g., MMSE, Trailmaking test Part A, Trailmaking test Part B) to the presence of small areas of brain injury, but that the injuries were to a wide variety of cortical (insula, temporal, frontal, posterior parietal) and subcortical (corpus callosum, caudate) locations.
26 Another study found that white-matter abnormalities in the periventricular region were more strongly associated with impaired performance than were white-matter abnormalities in other areas, implicating fronto-subcortical connections.
27 Several studies have utilized positron emission tomography (PET) and single photon emission computed tomography (SPECT) to examine the relationship between localized reductions in cerebral blood flow or cerebral metabolic rate and impaired performance on the clock-drawing task in various disorders. The most commonly-associated areas in patients with AD or MCI have been parietal and posterior cingulate cortices and the hippocampal region.
28–30 Areas implicated in patients with DLB dementia include both cortical (frontal, temporoparietal) and subcortical (putamen, thalamus) regions.
31,32 Studies utilizing voxel-based morphometry in patients with AD or MCI to assess the relationship between local gray-matter density and clock-drawing performance have reported associations with numerous cortical (temporal, frontal, parietal, cerebellum) and subcortical (thalamus, caudate) areas.
33–35 Of note, a study comparing several scoring systems found that all correlated with regional gray-matter volume in the right parietal lobe, but they differed for other areas, indicating that choice of scoring system will influence results.
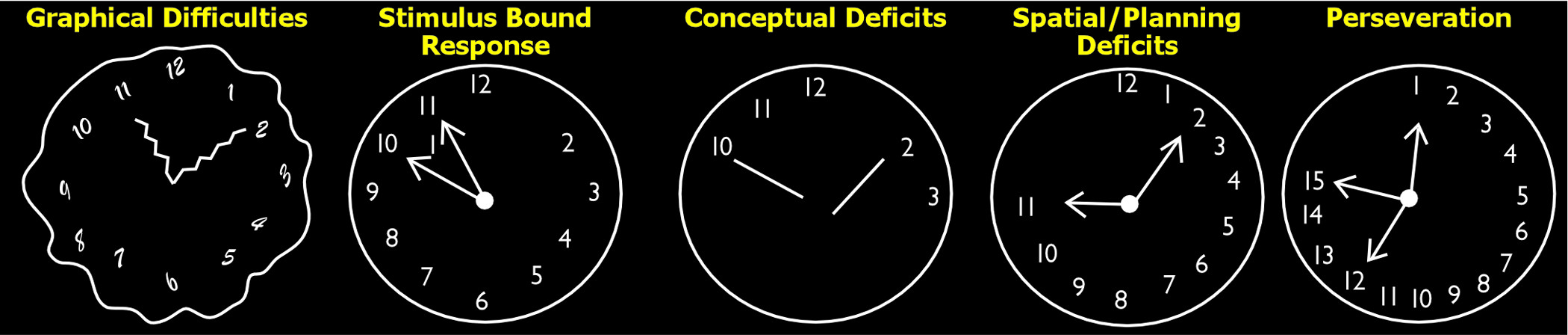
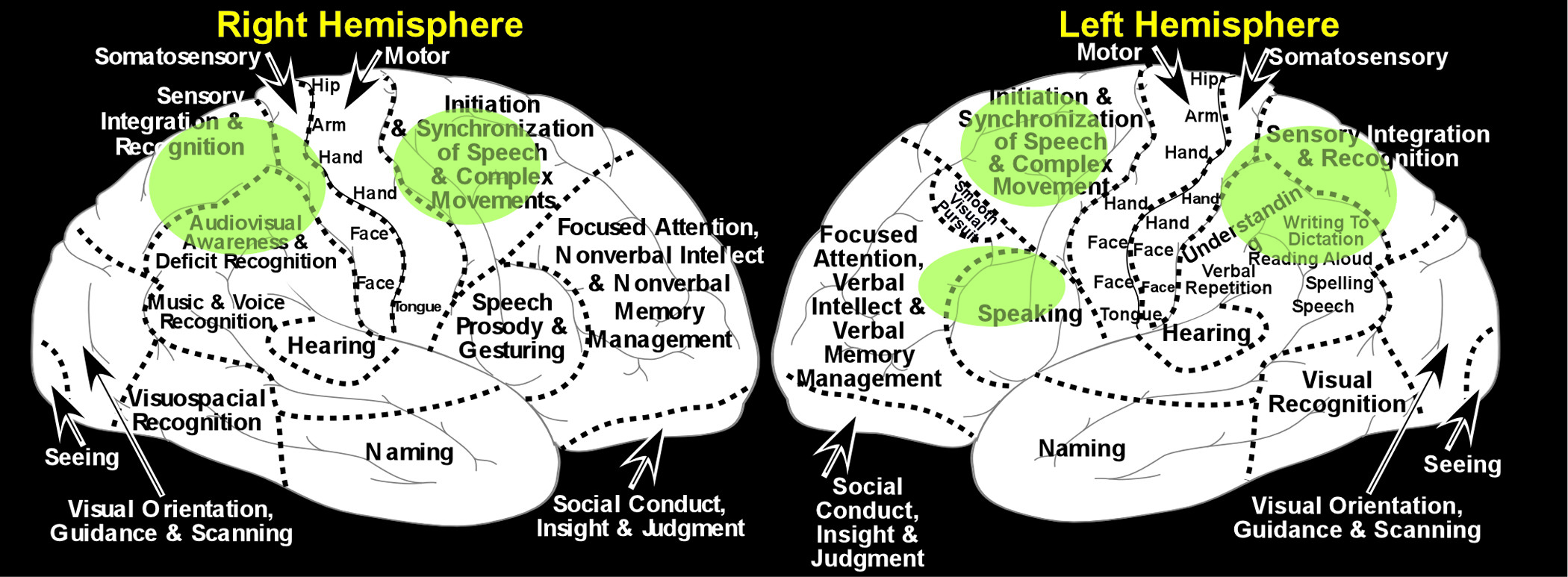
34Only a handful of studies have examined the anatomic correlates of specific types of errors. A lesion/deficit study in patients with focal brain injury identified two predominant patterns of errors on the clock-drawing task.
22 Problems with spatial organization and proper placement of numbers was more common in patients with right-hemisphere lesions, whereas problems with proper placement of clock hands (time-setting) were more common in patients with left-hemisphere lesions. The authors of this study noted that these findings are consistent with impaired visuospatial processing in the first group, and impaired language processing in the second. A study assessing the impact of high versus low load of periventricular white-matter abnormalities (WMA) on performance of clock-drawing in patients with dementia compared patients with either AD or vascular dementia to those with PD on total score and score by functional domain (gross motor, time, perseveration/pull, spatial layout).
36 The Low WMA group had better performance than the other two groups (PD; High WMA), which did not differ on either total score or domain scores. The Low WMA group performed better than high-WMA on the gross motor domain and better than PD on time and spatial layout domains. As noted by the authors, these results support the participation of both cortical and subcortical areas in the performance of this task.