To the Editor: The incidence of unilateral spatial neglect (USN) has been described in up to 30%−70% after an injury to the right hemisphere. USN is one of the strongest predictors of poor functional recovery, which can lead to more prolonged hospitalization
1 and disrupt rehabilitation and recovery of functional disabilities after stroke,
2 thus limiting independence.
1 However, USN is not usually assessed in routine examinations after stroke.
1 This fact could be motivated by the clinical heterogeneity of this syndrome and by the lack of standardized assessment tools. USN is assessed through functional or behavioral tests or by observation.
1 Functional tests focus on functional impairments but do not provide information about the deficits, which makes them suitable for assessment but not for establishing customized intervention protocols. Behavioral tests are usually paper-and-pencil tasks that can be compensated, thus hiding the clinical condition of individuals with USN. Some of the behavioral tests, such as the Behavioral Inattention Test (BIT),
3 evaluate the performance on daily activities such as phone dialing, coin sorting, or map navigation, in addition to performance on conventional cancellation tasks. However, the long duration of these tests can make them tiresome for many patients, especially for those with prominent attentional problems, and time-consuming for the clinical staff. The need for a therapist during the course of the test and its psycholinguistics requirements could also prevent the widespread use of these tests.
USN has been reported to alter visual search,
4 which has been posed as a cortically mediated behavior that involves attentional processing.
5 Individuals with USN tend to compensate visual search capability and achieve balance on the neglected side with cervical rotations.
6,7 Spatial and temporal patterns of visual search during cancellation, visuomotor, and visual search tasks have been proposed to improve examination.
8 However, neutral stimuli may not be valid to assess USN, because emotional valence has been shown to affect the spatial imbalance of both performance speed and stability in USN.
9We present a novel technique based on eye-tracking technology to quantify visual search on a behavioral task that could overcome some of the limitations of the current clinical examination tools for USN.
Case Report
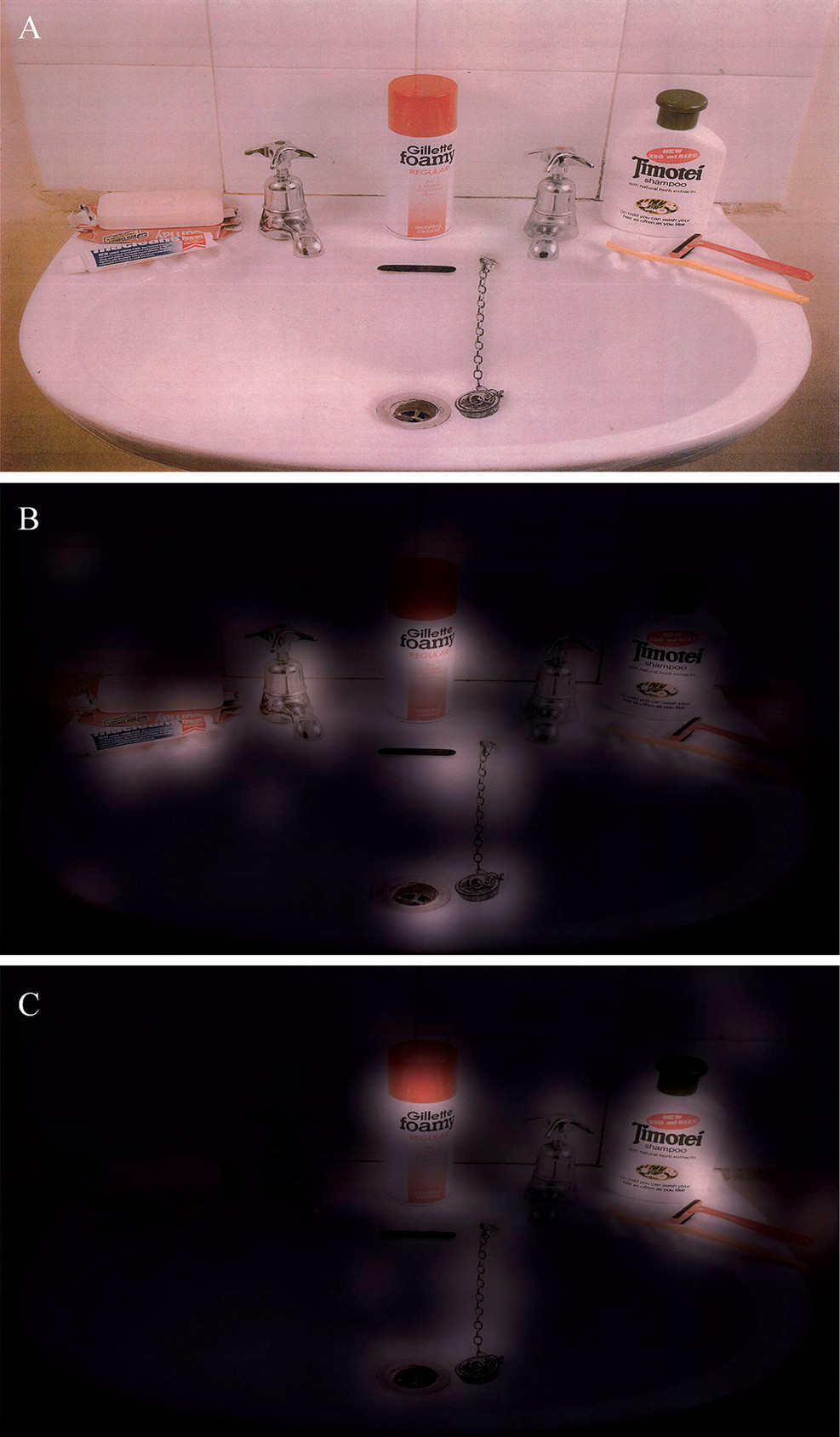
A 65-year-old woman with a right internal carotid artery occlusion that led to an ischemic focal lesion in the basal ganglia with hemorrhagic transformation of the nondominant cerebral hemisphere was admitted to our facility. The woman stayed 1 month in an acute inpatient care hospital, where she received physical therapy, and was referred to a longer-stay hospital, where she underwent a holistic neurorehabilitation program during 5 months. After that, 6 months after the onset, she was admitted to our long-term neurorehabilitation outpatient program. Results on neurological examination at admission revealed severe left hemiparesis and pronounced USN (National Institutes of Health Stroke Scale = 12). The patient manifested psychopathological disorders involving apathy and emotional lability that affected her daily living (Neuropsychiatric Inventory = 9) and self-awareness deficits of her impairments, limitations, and future planning (Self-Awareness Deficit Interview = 2+3+3). In regard to the neuropsychological domain, she was oriented to time and place, obtained a Mini-Mental State Examination score of 25/30, and showed attentional (Conners' Continuous Performance Test II–Hit Reaction Time = 1064.7 ms, Corsi block-tapping task total score = 4), memory (California Verbal Learning Test–Total Learning = 30; Immediate Free Recall = 5; Delayed Free Recall = 5), and a discrepancy between the performance on the paper-and-pencil test to assess USN (BIT–Conventional subtest = 133/146; BIT–Behavioral subtest = 68/81) and the functional difficulties that this syndrome caused in her everyday functioning (Catherine Bergego Scale = 23). The patient was enrolled in an experimental eye-tracking study where she and a healthy matched woman were required to look for 60 seconds at an image of the BIT depicting a washbasin (Behavioral subtest: picture 2, version B) and name the items present in it (
Figure 1A). Gaze parameters of both women were recorded using a low-cost eye-tracking device (the Eye Tribe Aps, Copenhagen, Denmark), and heat maps were estimated as superimposed distributions of eye fixations using the Open Gaze and Mouse Analyzer 4.5.
10 In contrast to the healthy participant, who revealed distributed fixations in all of the image (
Figure 1B), the patient presented an absence of fixations in the left side of the image (
Figure 1C), thus confirming the diagnosis and illustrating the behavioral complications that affected her everyday functioning.
Discussion
Although USN is a frequent and disabling consequence after stroke and standardized tools are available for therapists to identify this syndrome, use of these tools in the clinical practice is dramatically low. We presented a novel method to examine USN using an image of the BIT and eye-tracking technology to determine the gaze patterns of a poststroke patient with USN. Benefits of this protocol could be threefold: first, it provides qualitative (visual) but also quantitative (fixation times, gaze patterns, etc.) information; second, it is easy to administer and is not time consuming; and third, no specific cognitive or psycholinguistic condition is required to patients. In addition, the system allows repeated assessments, which are important to adjust interventions during the rehabilitation process. Recent advances have given rise to low-cost eye-tracking devices that are available for $100 and free software for data processing, which could promote the clinical integration on this technology. Although this protocol focuses on the visual input and the peripersonal space, it could be a potential tool to provide relevant information about the deficits and their functional consequences.
In our particular case, conventional measures of USN, such as the BIT, were not sufficient to reflect the severity of the impairment, which was evidenced by the gaze parameters. Objective information as, but not limited to, superimposed distributions of eye fixations provided by eye-tracking technology could be useful as complementary data for the assessment of USN.
Acknowledgments
The authors thank the staff and patients of the Servicio de Neurorrehabilitación y Daño Cerebral de los Hospitales NISA for their participation in this study.