This review forms part of a larger project to synthesize the evidence for the pharmacological management of neurobehavioral symptoms post-TBI as a prelude to the development of a clinical guideline. This systematic review, in addition to academic and clinical expert consensus, contributes toward the development of evidence-based recommendations for the pharmacological management of complex neurobehaviors, including KBS among patients post-TBI.
Methods
Prior to commencing the review, we searched the PROSPERO Database and Joanna Briggs database to ensure the proposed work was not duplicating any work currently in progress. This systematic review is reported according to the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines.
Inclusion and Exclusion Criteria
The present review was limited to case reports and case series of human participants available as full-text articles. Case reports and series of adolescents and adults (age: ≥13 years), both male and female, who had sustained a TBI displaying partial or full KBS symptoms were considered for inclusion. TBI was defined as an alteration in brain function or other evidence of brain pathology caused by an external force. Studies were included regardless of the severity of the injury or mechanism of injury. Participants with penetrating and nonpenetrating head injury were eligible for inclusion.
The following are considered characteristic KBS symptoms:
6 placidity (loss of normal anger or fear); hyperorality (tendency to explore objects in the mouth); visual agnosia (inability to recognize objects without loss of gross visual discrimination); hypermetamorphosis (tendency to attend to and manipulate objects in the visual field); indiscriminate dietary behavior, including hyperphagia (an excessive, insatiable appetite); and hypersexuality. Diagnosis of the full form of the syndrome is based on the occurrence of all the aforementioned symptoms.
6 Diagnosis of the partial form of the syndrome requires the presence of three or more symptoms.
4,6 Studies in which diagnosis of KBS was based on fewer than three symptoms were excluded from the review.
To be included, case reports were required to show medical evidence of TBI—that is, unequivocal TBI documented in medical records or other health or medical reports cited by the research team associated with the published article. Examples of unequivocal evidence include findings from brain imaging (e.g., computed tomography scan [CT], magnetic resonance imaging [MRI]), Glasgow Coma Scale (GCS) score, posttraumatic amnesia, and loss of consciousness.
Studies in a language other than English were included if a translation service was available to the researchers. The following studies were excluded: case reports or series of children up to the age of 13 years; case reports or series in which the mechanism of injury was not clearly stated and it was therefore not possible to conclude that TBI was the focus; and case studies based on self-report of TBI from either the individual or an informant, in the absence of other medical evidence regarding the head injury, as outlined above.
A description of the syndrome post-TBI focusing on demographic and injury characteristics, brain imaging, symptoms, and pharmacotherapy is provided. The outcomes that were the focus of this review were treatment effectiveness, as measured by resolution or improvement in KBS symptoms; overall recovery; and harms, including adverse events resulting from prescribed pharmacotherapy.
Search Strategy
The search strategy was developed on the basis of the population-intervention-comparator-outcome elements of relevance to this review (population in this case was KBS secondary to TBI). It included a range of Medical Subject Headings terms and keywords linked by Boolean operators. The searches were carried out on December 20, 2016, and repeated on November 5, 2017. Terms were modified as appropriate for each database. The following databases were searched with no date, age, or language limitation: MEDLINE: OVID SP interface; EMBASE: Excerpta Medica Database, PsycINFO: OVID SP interface; and SCOPUS. The MEDLINE search terms and number of results for each database are included in the online supplement.
To ensure the search was as comprehensive as possible, we supplemented the formal search of bibliographic databases with searches of Google Scholar and ResearchGate. We also carried out electronic searching of the following online journals: Brain Injury, Neuropsychology, Journal of Neurotrauma, Neurocase, and BMJ Case Reports. We reviewed reference lists and bibliographies of retrieved articles to identify research not located through other search strategies. Finally, we asked colleagues whether they were aware of any case reports in this area.
Study Selection
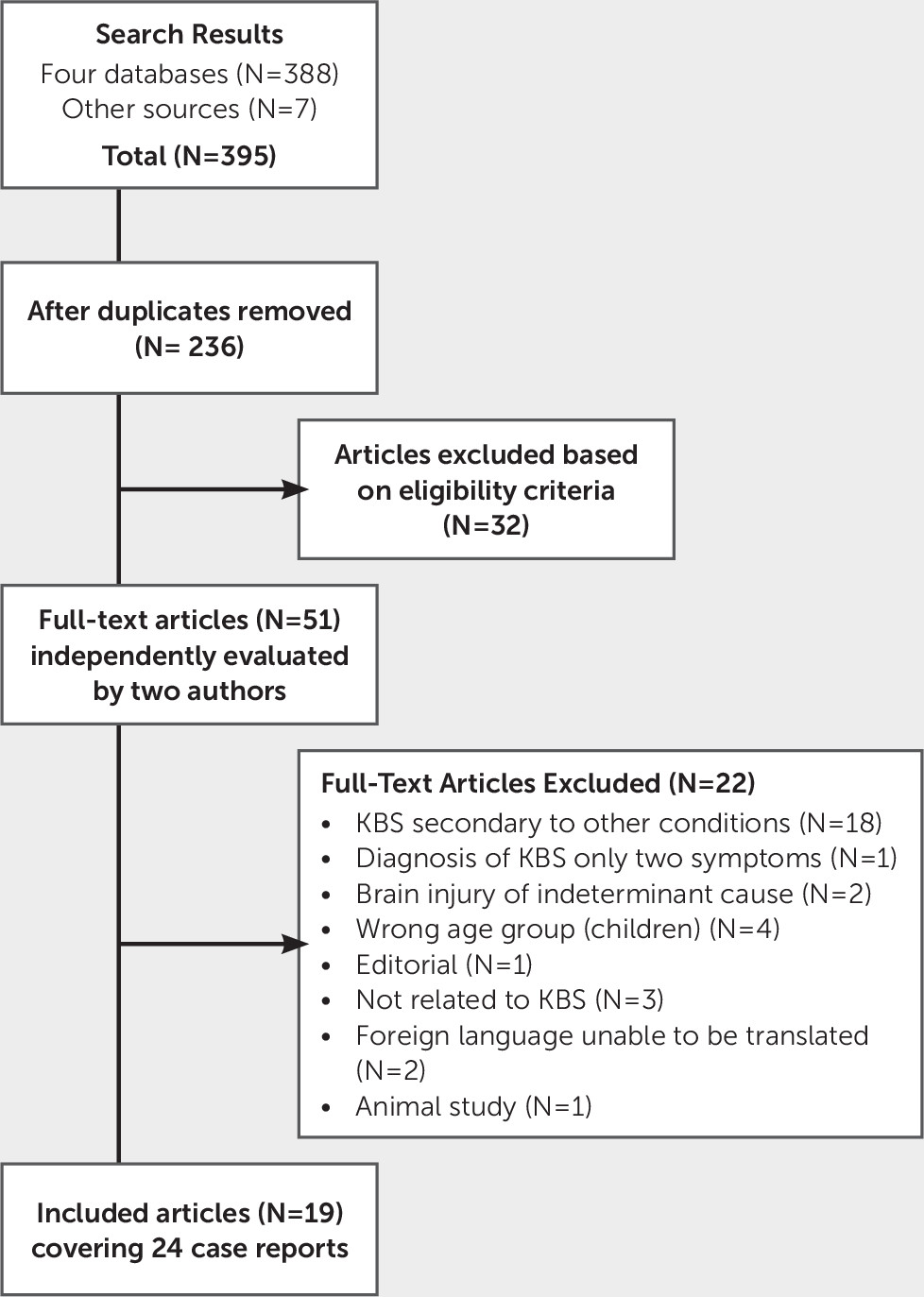
Results from the four database searches were downloaded into Endnote×7 and deduplicated. Titles and abstracts were screened by two independent reviewers (FC, AK) against the inclusion and exclusion criteria for the review. Studies that potentially met the inclusion criteria at the title and abstract stage were retrieved in full and independently assessed against the inclusion criteria by two members of the review team (FC, AK). An article could be included in the review if it contained at least one relevant case. Articles that included both relevant cases and cases that did not meet the inclusion criteria (e.g., because of patient age or KBS not being secondary to TBI) were still eligible. Discussion between reviewers was used to achieve agreement over the eligibility of two studies. Full-text studies that did not meet the inclusion criteria were excluded, and reasons for exclusion are provided in
Figure 1.
Assessment of Methodological Quality
Quality was assessed by three reviewers (FC, AK, EA) using the Joanna Briggs Institute critical appraisal eight-question checklist for case reports. (This checklist is included in the online supplement.) In brief, the questions assess the quality of reporting of the patient’s demographic characteristics, current clinical condition, diagnostic tests or assessment methods, interventions or treatment, postintervention clinical condition, harms and unexpected consequences, and take-home lessons.
Data Extraction
Where available, the following data were extracted from the included case reports with a customized data-extraction tool pilot tested on two case reports of KBS secondary to herpes simplex virus (FC, AK). Minor modifications to the data-extraction tool were made following the pilot. To aid interpretation of data, we sought to ensure that one of the reviewers involved in data extraction had a medical degree (AK). The specific data items extracted, where available, are as follows.
We extracted data on country of the case; age, gender, and mechanism of injury of the case; and report of loss of consciousness (on the basis of GCS score and presence or absence of coma). We also gathered information on the study population: TBIs (injuries other than to the head, time postinjury), KBS syndrome symptoms, whether KBS was full or partial, time at KBS onset, and duration of KBS. We extracted data on the imaging used (CT, MRI) and on the pharmacotherapy intervention if one was used, including type of pharmacological compound, dose, frequency and duration, and cointerventions and their details. We tracked outcomes and when they were measured as well as treatment response and treatment adverse events.
Discussion
To the best of our knowledge, this is the first systematic review to identify and synthesize the evidence for KBS secondary to TBI from case reports. Using a defined search strategy applied to four bibliographic library databases, we identified 24 case reports that met the inclusion criteria and form the focus of this review. Notwithstanding the methodological limitations associated with case reports, given the rarity of KBS and the lack of studies with higher quality methodologies, the use of case reports offers opportunities to better understand KBS post-TBI.
In the current review, hypersexuality, hyperorality, and aggressive behavior were the most common presenting KBS symptoms. Visual agnosia was the least common symptom. Gerstenbrand et al.
37 summarized their experiences with posttraumatic cases of KBS, reporting clinical data on 40 case subjects diagnosed between 1978 and 1981. Although no individual case data were presented, the frequency of KBS symptoms was reported. Symptoms of bulimia, memory disturbances, hyperorality, and visual agnosia occurred in 30 cases. Hypersexuality occurred in 18 cases, and aggressiveness occurred in 11 cases. Persistence of hypersexuality at 1 year was noted in 12 cases, bulimia in eight cases, and aggressiveness in 10 cases. Although the sources of the cases are not described, the majority were male (77.5%), and the age range indicates the cohort was younger, because children were included (aged 7–33 years [mean=17.2 years]). The differences may reflect the heterogeneous nature of TBI. It is unclear whether the patients in the study by Gerstenbrand et al.
37 had TBI or other acquired brain injury. Six case subjects died within 10 weeks of their accident, and thus it is possible that the cases described in the current review were less serious.
Although the natural history of KBS post-TBI is not known,
23 it appears as a chronic, persistent state for some patients and a transient, resolving state for others.
6 Of the case reports described in the current review, the majority of cases showed partial or full recovery. For the majority of cases, the course of KBS ranged from 5 days to 1 year. For other cases (N=8), the syndrome was ongoing 1–25 years following onset, depending on when the patient was evaluated. Although it cannot be ruled out that this reflects a positive-outcome publication bias, the extent of recovery is consistent with the study by Formisano et al.,
38 who examined the global outcome of 19 patients with KBS secondary to severe brain injury following a traffic accident. To be included in Formisano et al.’s study, cases were counted as KBS if they had two of the KBS symptoms.
38 This is at odds with the definition of partial KBS, which requires three symptoms.
6 Although no individual case data were presented, of the 19 included KBS patients, four did not regain independence, six achieved family integration, and nine achieved work integration. In keeping with Formisano et al.’s
38 findings, lesions in the temporal lobes were common in the case reports included in the current synthesis.
The nature and anatomic location of the lesions necessary to produce human KBS post-TBI have not been definitively determined, in part because of the limits of current routine structural imaging. Investigators have proposed a number of hypotheses. Góscínski et al.
19,20 proposed a bilateral injury of the mediobasal temporal lobe as a result of swelling or edema of the brain and compression of the arteries. Yoneoka et al.
25 hypothesized that KBS symptomatology may reflect edema-induced transient dysfunction of the right temporal and basal frontal lobes. Slaughter et al.
29 proposed combinations of posterior frontal and anterior temporal lobe defects, and Deginal and Changty
23 postulated disruptions of pathways connecting the dorsomedial thalmi with prefrontal cortices and other limbic areas. It is notable that the extent of neurological deficits did not correlate with the level of personality disturbances.
27 More recently, Caro and Jimenez
7 proposed that KBS results from mesiotemporal lesions or other changes (possibly transient) leading to hypofunctioning in the amygdala or its projections, regardless of etiology. In the case of transient KBS, they proposed that the disappearance of KBS symptoms follows improvement in the localized neuronal dysfunction.
A secondary objective of the current review was to compare and contrast the individual case reports that described pharmacological management of KBS-related symptoms. The French SOFMER guidelines on drugs for behavioral disorders following TBI reported level 4 grade C evidence for the use of carbamazepine.
18 This was based on a single case series of four patients treated with carbamazepine.
19,20 No data on duration of treatment or time point at which treatment was initiated were provided. Dose of carbamazepine was not reported for case 1.
The authors reported that the patients showed improvement, as measured by the Glasgow Outcome Scale (GOS), at hospital discharge, 3 months, and 6 months after trauma when given carbamazepine during hospitalization and after discharge.
19,20 Case 2 did not show a change in GOS score. The nature of the improvement was not described. Given the complexity of the syndrome, the fact that only two cases can be definitively considered as TBI, the lack of pharmacological information, and the lack of reporting on which symptoms improved, guideline recommendations based on this article should at best be circumspect.
Ten case reports that described treatment with carbamazepine were included in this review, and they provide some additional evidence on the use of carbamazepine in relation to KBS. Improvement of symptoms was seen within 3 weeks of commencing carbamazepine,
22 and in one case, complete resolution of symptoms was reported,
34 but no time frame was specified. Other cases reported general improvements in symptoms for patients taking carbamazepine, but, again, no time frame was mentioned when improvements occurred.
23,27,34,35Carbamazepine is a carboxamide-derivate antiepileptic drug with a chemical structure similar to tricyclic antidepressants and is used in the management of seizure disorders, neuropathic pain, and psychiatric disorders.
39 The efficacy of carbamazepine as an anticonvulsant drug has been demonstrated among patients with temporal lobe epilepsy
40 with additional symptoms similar in nature to KBS, which could be one of the reasons behind its use. Moreover, both full and partial remission of symptoms following carbamazepine treatment have been noted in KBS associated with a range of etiologies other than TBI. Unfortunately, the case reports in the current study did not report in detail which of the diagnostic KBS symptoms improved. Improvements in behavioral, hyperorality, and cognitive symptoms were documented.
Of the 24 cases described in this systematic review, 10 were treated with carbamazepine. Overall, the cases suggest that carbamazepine may be an effective treatment for certain symptoms of KBS. Of the cases treated with carbamazepine, a serum carbamazepine trough level of >6 µL/mL was reported for three patients (optimal therapeutic range: 4–12 µL/mL). Because of its potentially severe toxic effects (e.g., ataxia, seizures, dystonic reaction, and even coma), it is crucial to avoid carbamazepine overdosing.
39 Although a serum trough level of 6 µL/ml is still within the recommended range, the lack of effect with carbamazepine in Slaughter et al.’s
29 case 1 maybe associated with a subtherapeutic trough level.
The antipsychotic drug chlorpromazine usually shows a high sedative effect and increased potential for extrapyramidal symptoms. In the case presented by Hooshmand,
41 chlorpromazine might have been given as a treatment for psychotic symptoms, and the treatment then could have been switched to carbamazepine for long-term seizure management.
34 In terms of effectiveness, the early introduction of carbamazepine seems to be important, as stated by Góscínski et al.
19,20The prescription of multiple medications was described in four cases. In Slaughter et al.’s
29 case 2, both lorazepam and valproic acid were prescribed. Lorazepam is usually prescribed for its anxiolytic effects, and its reported pharmacokinetic interaction with valproic acid might lead to further aggravated sedative effects.
42 In Slaughter et al.’s
29 case 1, the patient received several antidepressants, including sertraline and trazodone. Sertraline was later substituted with fluoxetine; both drugs are SSRIs. Some KBS symptoms have obsessive-compulsive disorder (OCD) features, and sertraline at higher doses has been shown to be effective with OCD.
43 However, sertraline and fluoxetine are both metabolized on common cytochrome P
450 pathways, including CYP2D6, and pharmacokinetic interactions might be expected in the present case given the rapid succession.
44 The antidepressant trazodone, a potent serotonin and α1-adrenergic receptor antagonist and weak serotonin reuptake inhibitor, was administered together with carbamazepine.
45 With carbamazepine being a known inducer of CYP3A4, potential interactions might be clinically relevant and exacerbate symptom remission.
46,47It is important to acknowledge that this systematic review is subject to limitations that are a feature of case reports. Because case reports are retrospective observational studies, causal inference cannot be made. There is a risk of positive-outcome bias, and one might overinterpret features of the case because of the different emphasis given by authors to cases. For the current review, data were missing for some of the collected attributes. Underreporting of when KBS patients were assessed during their hospital stay, during rehabilitation, and following hospital discharge limits the interpretation of the duration of KBS symptoms.
Because it is a natural experiment, the case cannot be repeated, and the care of patients with KBS might have changed over the years. Because peer-reviewed articles on KBS are not very common, the search strategy did not include a large range of terms, and it is possible that relevant cases were missed. We think the likelihood of this is small given the range of databases searched, the number of reference lists consulted, and the search of Google Scholar.
Notwithstanding these limitations, the strengths of the review include the systematic identification of cases through a specified search strategy and a critical appraisal of the reports’ quality. Moreover, no date or language restrictions were applied, and we were able to get three studies translated. The review brings together 24 cases of KBS post-TBI, of which half were treated with pharmacotherapy. This review will help clinicians to understand the clinical spectrum of KBS post-TBI and may offer guidance in the personalization of treatments in clinical practice.