Electrode placement is a critical ECT parameter, with both therapeutic and side-effect implications. The two most common electrode placements are bitemporal (BT) and right unilateral (RUL [or d’Elia electrode placement]
2) ECT. In 2011, the Food and Drug Administration (FDA)
3 concluded that BT ECT is the most effective electrode placement. Nevertheless, RUL ECT has been increasingly prevalent in the past few decades given its more tolerable profile.
4 Challenging common clinical assumptions, some studies
5,6 have suggested that RUL ECT is not inferior in efficacy compared with BT ECT. Altogether, it seems that our knowledge of the comparative efficacy and side-effect profiles of RUL and BT treatments could be partially revised with additional nuances, and these clinical considerations would benefit from a mechanistic understanding of the distinct biological effects of these treatment parameters.
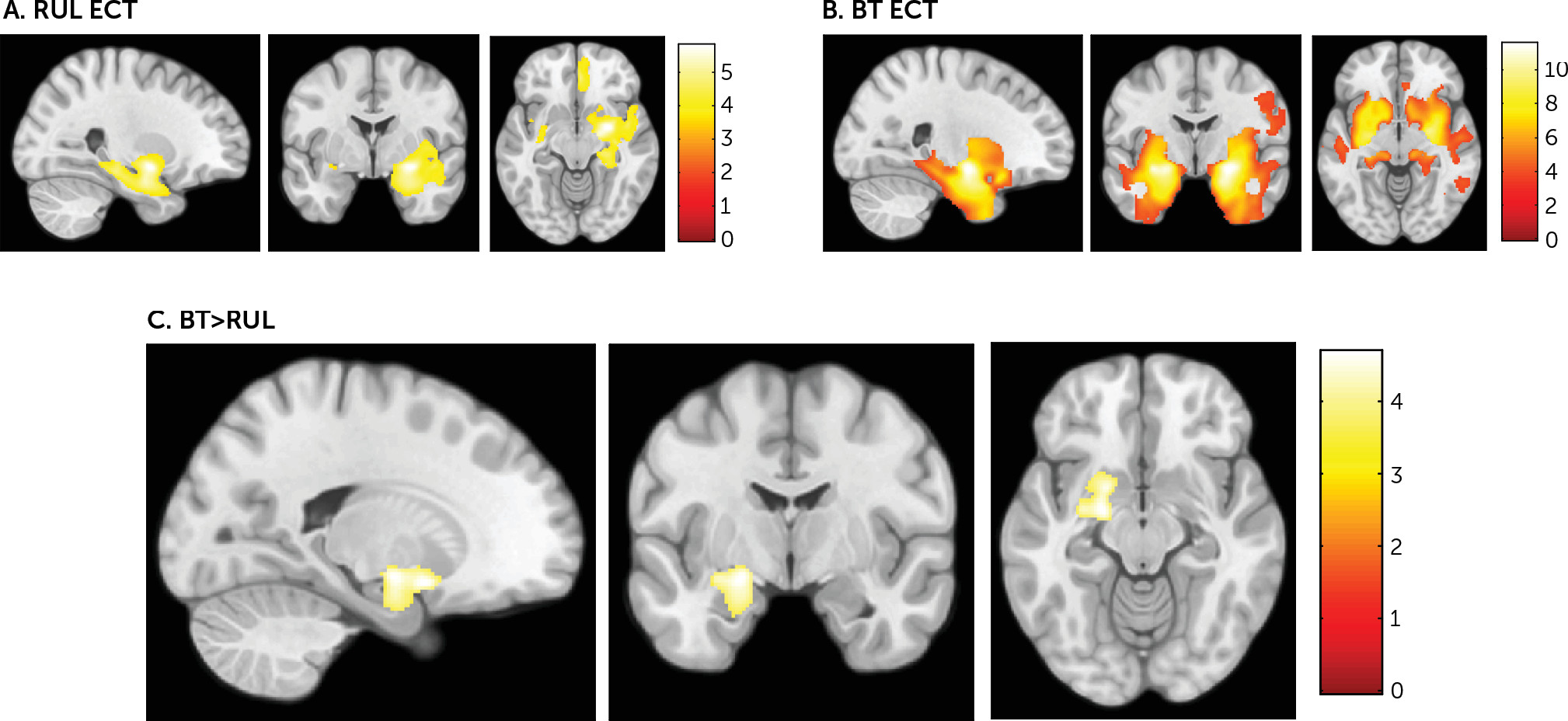
Gray matter volume increases, mainly in the limbic temporal lobe, have been observed after RUL and BT ECT.
7–19 Although most studies have not found an association between volumetric and clinical changes, some have, although not always in the same directions.
10,16,19,20 The nature of these changes may shed light on the mechanism of action of ECT, but recent studies do not allow a clear disambiguation between the mechanisms of BT versus RUL ECT. Indeed, only one recent structural neuroimaging study assessed the effect of RUL versus bilateral (that is, bitemporal and bifrontal) ECT. However, as opposed to our whole-brain approach, the authors limited their focus to volumetric changes in the hippocampus.
20 Results from this study indicated that electrode placement determines the extent of volume change in the right and left hemispheres, with bilateral electrode placement being associated with bilateral hippocampal changes, whereas RUL electrode placement was preferentially associated with right hippocampal changes. In addition to these volumetric differences, previous neurophysiological studies have shown that slow-wave activity after RUL ECT was observed in the right hemisphere, whereas slow-wave activity was more prominent over the left hemisphere with BT ECT.
21In the present study, we aimed to assess the effects of ECT electrode placement, and specifically the differential impact of RUL versus bifrontotemporal ECT, on whole-brain volumetric changes in study subjects with treatment-resistant depression. We hypothesized that despite the common causal association with the ECT-induced generalized seizure, RUL and BT electrode placements would lead to different topographic distributions of the volumetric changes observed after ECT: specifically, study subjects treated with BT ECT, in comparison with subjects receiving RUL treatment, would show greater gray matter volume increases in the left hemisphere.
Methods
Participants
We recruited 24 study subjects with treatment-resistant depression from two research centers: the Mood Disorders Inpatient Unit of Bellvitge University Hospital, Barcelona, Spain (N=12), and the Department of Psychiatry at Massachusetts General Hospital (MGH), Boston (N=12). The mean age of study subjects from Bellvitge University Hospital was 59.17 years (SD=8.02), and the mean age of the study subjects from MGH was 42.25 years (SD=15.78).
Fifty percent of subjects from each cohort were men (Bellvitge, N=6; MGH, N=6).
Age and gender were used as covariates for statistical analyses. All study subjects met criteria for a major depressive episode according to DSM-IV-TR
22 criteria as well as the following structural clinical interviews: the Structured Clinical Interview for DSM-IV Axis I Disorders–Clinician Version (SCID)
23, for the Bellvitge University Hospital cohort, and the Mini-International Neuropsychiatric Interview 6.0 (MINI)
24, for the MGH cohort. Exclusion criteria included 1) the presence or past history of a severe medical illness or neurological disorder, 2) contraindication to MRI scanning or abnormal MRI on visual inspection, and 3) a history of ECT during the past 12 months. Pharmacotherapy remained unchanged throughout the ECT protocol, with close monitoring for unwanted adverse effects (
Table 1; see also Table S1 in the
online supplement). Moreover, subjects in the Bellvitge University Hospital cohort underwent longitudinal clinical assessment using the 21-item Hamilton Depression Rating Scale (HAM-D),
25 and subjects in the MGH cohort were assessed with the Quick Inventory of Depressive Symptomatology (QIDS).
26 The study was approved by the local ethical review board of each center and was performed in accordance with the Declaration of Helsinki. All participants provided written, informed consent after a detailed description of the study was given.
ECT
The 12 subjects in the Bellvitge University Hospital cohort were treated with bifrontotemporal brief-pulse (0.5–1 ms) ECT using a Thymatron System IV device (Somatics, Lake Bluff, Ill.). Anesthesia was induced with intravenous thiopental (2–2.5 mg kg
−1), and succinylcholine (0.5 mg kg
−1) was used for muscle paralysis. Initial stimulus dose was determined by using the half-age method,
27 and subsequent dosing was determined according to seizure morphology adequacy. The 12 subjects in the MGH cohort were treated with ultra-brief pulse and brief pulse (0.3–0.5 ms) RUL ECT (d’Elia electrode placement
2) using a MECTA spECTrum 5000Q machine (Portland, Ore.). Anesthesia for the procedure was provided using methohexital (0.8–1.2 mg kg
−1) for induction and succinylcholine for muscle relaxation (0.5–1 mg kg
−1). Initial stimulus dose was determined by titrating the seizure threshold, starting with 19 millicoulombs for women and 38 millicoulombs for men. Subsequent treatments were performed at six times the estimated seizure threshold. During an acute course of ECT, treatments were administered three times per week every other day at both centers.
Image Acquisition and Preprocessing
All study subjects were scanned two times: before the first ECT session (MRI 1) and after completion of the ECT course (MRI 2). A 3.0-T structural T1-weighted MRI high-resolution structural scan was locally acquired for each participant. Study subjects in the Bellvitge University Hospital cohort were scanned with a Philips Achieva 3.0-Tesla magnet scanner (Amsterdam) equipped with an eight-channel phased-array head coil (160 slices, repetition time=8.1 ms, echo time=3.7 ms, flip angle=8°, field of view=240×240 mm, matrix size=256×256 pixels, in-plane resolution=0.94×0.94 mm2, slice thickness=1 mm). Study subjects in the MGH cohort were scanned at the Martinos Center for Biomedical Imaging with a Siemens Skyra 3.0-Tesla magnet scanner (Munich, Germany) equipped with a 32-channel head coil (156 slices, repetition time=2,530 ms, multi-echo time=1.69, 3.55, 5.41, and 7.27 ms, flip angle=7°, field of view=256×256 mm, matrix size=256×256 pixels, in-plane resolution=1×1 mm2, slice thickness=1 mm).
All structural MRI data were processed on a Microsoft Windows platform using technical computing software (MATLAB, 7.14, MathWorks, Natick, Mass.) and Statistical Parametric Mapping (SPM12, Welcome Department of Imaging Neuroscience, London). The preprocessing consisted of an initial rigid-body within-subject coregistration to the first scan to ensure good starting estimates. This was followed by a pairwise longitudinal registration between the scans of each participant to obtain an average image and a Jacobian difference map. The average image was segmented, and the gray matter voxels were multiplied by the Jacobian difference map to obtain a gray matter volume change map for each participant. Next, we generated one specific template of both study samples (in Montreal Neurological Institute space) using Diffeomorphic Anatomical Registration Through Exponentiated Lie Algebra algorithm,
28,29 which was used to spatially normalize the gray matter volume change maps. Finally, images were smoothed with a 6-mm full-width at half maximum isotropic Gaussian kernel.
Statistical Analyses
Sociodemographic and clinical data were analyzed with SPSS version 21 (SPSS, Chicago) using nonparametric tests.
We used an independent two-sample model to derive a t statistic map comparing the gray matter volume change maps between participants with treatment-resistant depression treated with bifrontotemporal ECT (BT group) and participants with treatment-resistant depression treated with right unilateral ECT (RUL group). We initially estimated within-group volumetric changes (using two one-sample t tests at a p value <0.05, two-tailed, family-wise-error corrected for multiple comparisons across the whole brain) and created a combined mask (adding significant changes from both groups) in which we investigated between-group differences. This approach has been used as a strategy to increase the sensitivity directed toward our main objective (i.e., BT versus RUL ECT comparison). Age and gender were included as confounding covariates. Statistical significance was set at a p value <0.05 (two-tailed), family-wise-error corrected for multiple comparisons across all in-mask voxels (i.e., using small-volume correction procedures across all voxels showing volumetric changes in the RUL and BT groups). This mask contained 20,592 voxels.
Discussion
This is the first study, to our knowledge, comparing the whole-brain volumetric correlates of BT and RUL ECT in study subjects with treatment-resistant depression. Consistent with previous research,
7–19 we observed that ECT is associated with gray matter volume increases in limbic structures, including the ventral striatum, the amygdala, and the hippocampus. Indeed, neuroimaging, neuropathological, and lesion analysis studies have highlighted the importance of cortico-limbic circuit disruption in depression.
30 However, our study provides novel insight regarding the gray matter volume increases associated with ECT electrode placement, because we described that limbic gray matter volume increases are specifically observed ipsilateral to the hemispheres stimulated: the pattern of gray matter change after BT treatment includes both hemispheres, compared with the unilateral right hemisphere changes observed after RUL ECT. In this sense, our results concur with the recent study by Oltedal et al.,
20 who observed that while bilateral ECT accounted for similar volume changes in right and left hippocampi, RUL ECT led to more focal effects in the right hippocampus. It is noteworthy that although this study also demonstrated a dose-dependent effect of the number of ECT sessions on hippocampal volume, such ECT parameter did not significantly differ between our study groups, and regressing it out did not change our results. Therefore, our whole-brain analyses showed that these changes are not limited to the hippocampus but extend to other limbic structures critical for negative and positive affective processing and the pathophysiology of depression, such as the amygdala and the ventral striatum.
31The literature on BT ECT versus RUL ECT has shown that the seizure evoked by BT ECT is better generalized throughout the brain.
32 Indeed, current density in unilateral ECT placements is substantially larger in the ipsilateral hemisphere than in the contralateral hemisphere.
33,34 Accordingly, our brain volumetric findings appear to be related to the specific placement of the electrodes and, therefore, likely to be associated with the underlying current density distribution. Additionally, although some neuroimaging studies that mixed RUL ECT and BT ECT have reported that gray matter volume increases were not clearly lateralized to the stimulation side,
7,11,14,16,35 when the brain volumetric effects of RUL ECT
10,36 or BT ECT were specifically assessed,
8,13,17,19 gray matter volume increases were consistently observed underneath the stimulation side (except in the study by Depping et al.,
36 which limited the analysis to cerebellar volume changes). Overall, our findings, along with results from previous studies, clearly support the notion of a direct relationship between electrode placement and lateralization of ECT-induced volumetric increases. However, contrary to this line of argument, it is noteworthy that we also observed volumetric increases in the pregenual anterior cingulate cortex that were limited to the right hemisphere both in the BT group and the RUL group. Further research is warranted to ascertain the possible mechanisms underlying this finding, which may putatively involve interactions between current density and the specific structural plasticity features of the different brain regions.
Regarding clinical effects, we observed an 89.26% clinical response (as measured by the percentage of change in HAM-D score) among study subjects with treatment-resistant depression who received BT ECT, whereas study subjects who received RUL ECT showed a 33.41% clinical response (as measured by the percentage of change in QIDS score). These results are consistent with the 2011 conclusions presented by the FDA,
3 indicating that RUL ECT is less effective than BT ECT. Although the greater generalization of the evoked seizure in BT ECT
32 has been thought to predict greater clinical response,
37,38 biophysical differences across the two electrode placements, such as induced electric field distribution or intensity in the brain, may be causally linked to the clinical differences between electrode placements. In this sense, the greater capability of BT ECT to induce comparable electric field strength in both hemispheres may explain the clinical superiority of this electrode placement.
34 However, despite the characteristically low clinical response in the RUL ECT group, we also observed neuroanatomical changes associated with RUL ECT. In this sense, it is important that recent research suggests that volumetric changes should not be necessarily linked to treatment response.
20On the other hand, Abrams et al. suggested that slow-wave activity after BT ECT is accentuated in the left hemisphere
21 and that left unilateral (LUL) electrode placement may be as effective as BT ECT,
39 findings that dovetail with the positive association between volume increases in the left hemisphere and clinical improvement observed in our previous study.
19 Therefore, another plausible interpretation of the clinical superiority of BT ECT may be, specifically, the modulation of the left hemisphere. Indeed, other effective brain stimulation treatments for treatment-resistant depression, such as transcranial magnetic stimulation, primarily target the left hemisphere.
40 Moreover, despite the traditional association between left hemisphere stimulation and verbal memory disruptions, some reports suggest that patients who receive LUL may avoid specific side effects, such as disruption in nonverbal functions.
41 Therefore, LUL may be a reasonable treatment alternative for specific subgroups of patients.
The present study has several limitations. Most importantly, there was a perfect collinear association between ECT electrode placement and scanner type, because these analyses were conducted independently (i.e., without possibility for a priori randomization) and our results stem from a post hoc analysis of the merged data sets. Although these confounders might have introduced nuisance between-group variance, the longitudinal processing applied to our data allowed us to minimize such putative interscan confounding effects: study subjects from the different scanners were never directly compared, and, instead, we exclusively compared the gray matter volume change maps that were obtained from each individual patient. Moreover, the anatomical correspondence between the stimulation side and structural changes would be difficult to explain by differences in scanner-specific artifacts and suggests that our findings are the consequence of ECT treatment. Nevertheless, a prospective study with a priori randomization would be needed to fully confirm our results. Second, we cannot determine what effect, if any, concurrent pharmacological treatment had on our results, although in an attempt to minimize this confounding effect, pharmacological treatment was not modified throughout the entire ECT course. Third, the putative differences between the standardized scales used at each study site (i.e., HAM-D and QIDS) in ascertaining remission from depression could have compromised our clinical findings. Finally, other ECT parameters in addition to electrode placement differed between the study groups (i.e., dosing method and pulse width). Therefore, our results should plausibly be better understood as depicting the neurobiological correlates of two different treatment approaches differing in various associated factors, of which electrode placement was the primary driver of other differences (e.g., BT ECT would be associated with lower stimulation intensity and greater therapeutic response). Nevertheless, despite being unable to specifically control for these other factors, due to their collinear association with electrode placement, our findings provide a framework to interpret previous results and stimulate further research on the relationships between ECT parameters with changes in brain biology and clinical efficacy in a prospective controlled manner.
In conclusion, our findings indicate that brain volumetric changes associated with ECT may be ipsilateral to the stimulation side (i.e., RUL ECT triggered gray matter volume increases limited to the right hemisphere, whereas BT ECT unleashed bilateral gray matter volume increases). Despite its diffuse biophysical properties, the biological effects of ECT are more specific than previously considered, and this specificity is parameter-dependent. Because the lateralization of gray matter volume changes may be associated with the clinical effects of ECT (i.e., efficacy and side effects), our results highlight the importance of carefully considering electrode placement in clinical settings in order to develop tailored treatment protocols, which may include RUL, BT, or even LUL approaches. Moreover, clinical research should carefully consider electrode placement in order to properly interpret the results from studies aimed toward unraveling the mechanisms of action of ECT.