To construct a natural history of the sociopathic personality, a 10‐year study was made from interviews and record information. The study of adult status of former patients of a now defunct St. Louis child guidance clinic located 90% of 524 patients 30 years after clinic referral and obtained adult records for 98% of those located. The subjects were predominantly male and American born of White protestant families of low socioeconomic status.
‐Lee Robins, PhD, Deviant Children Grown Up, 1966
A recent analysis of national trends in mental health‐related emergency department visits among youth showed a doubling of United States (US) pediatric emergency room visits over the last decade (
1). Particularly striking were the elevated rates of pediatric emergency visits for behavioral dysregulation, commonly operationalized as perceived aggression, outbursts, and tantrums leading to functional impairment. Among 10–14 year old children, emergency admissions for behavioral disorders more than tripled from 4.2 per 1000 capita between 2011 and 2012 to 12.7 per 1000 during 2019–2020 (
1). Even though the Centers for Disease Control and Preventions (CDC's) Youth Risk Behavior Survey data did not show significant increases in child and adolescent drug use through 2021 (
2), December 2023 data from the National Institutes of Health raised concern about rising rates of unintentional overdose among US youth (
3).
Against this backdrop, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry (AACAP), and the Children's Hospital Association jointly declared a National State of Emergency in Children's Mental Health in 2021. Since 2020, US Surgeon General Vivek Murthy issued two advisories to the American public describing the need for up‐to‐date surveillance data on clinical outcomes; such advisories are typically “reserved for significant public health challenges that require the nation's immediate awareness and action” (
4). Unfortunately, the youth mental health crisis does not show evidence of subsiding. A 2022 report by AACAP estimated that only half of children and adolescents in the US with diagnosable mental health problems receive the treatment they need, even though 50% of mental health disorders show their first signs before a person turns 14 years old (
5).
Conduct disorder (CD) is posited to be one of the most common conditions underlying the recent increases in acute care admissions for behavioral dysregulation in the US (
6,
7,
8). Historically, our understanding of CD's phenomenology and diagnostic criteria was influenced by Prof. Lee Robins' seminal sociological studies of an overwhelmingly White sample of children in 1960s Saint Louis, Missouri (
9). As the assessment of CD can be subjective and vary across cultures, Prof. Robins emphasized the importance of considering historical, environmental, geographical, and cultural contexts for diagnosing CD (
10). Yet, in the decades that elapsed following Prof. Robins' initial studies on CD, there are increasingly concerns for racial and ethnic disparities in the diagnosis of CD. While the 1985 Epidemiological Catchment Area study found that non‐Hispanic White people were more likely to receive CD diagnoses than Black peers (
11), newer studies found results suggestive of the contrary. For instance, in a large 2015 observational analysis of fifth graders in the Healthy Passages cohort, non‐Hispanic Black race conferred a 30% increased risk of probable CD symptoms, judged by the research staff, compared to White peers (
12). Another analysis, evaluating the fit of several measures of externalizing personality, raised concerns about the validity of CD diagnostic measures when applied to non‐White samples (
13).
Such racial and ethnic disparities in CD diagnosis are concerning for several reasons. First, the diagnosis of CD may increase the likelihood of criminal legal system involvement in the US (
14) which has one of the highest rates of youth incarceration worldwide. This is particularly problematic when considered against the backdrop of
structural racism, which can be defined as the “totality of ways in which societies foster racial discrimination through mutually reinforcing systems” that span legal, interpersonal, institutional, socioeconomic, and cultural norms (
15). In the US, mass incarceration disproportionately impacts racially and ethnically minoritized communities and is associated with a myriad of negative physical and mental health outcomes (
15). Second, externalizing behaviors may also be a reflection of disorders such as post‐traumatic stress disorder (PTSD), substance use disorders (SUDs), and attention‐deficit hyperactivity disorder (ADHD) (
16) that often co‐occur with CD diagnoses, yet are undertreated in Black children (
17,
18). For instance, a recent analysis showed that among children with major depressive disorder, rates of suicide attempts have significantly increased—particularly among racially and ethnically minoritized children with SUDs—without any corresponding change in mental health care utilization (
19), and the CDC's 2021 Youth Risk Behavior Survey Data showed that Black high school students were more likely to attempt suicide and experience serious injury during suicide attempts than White peers (
2). Additionally, studies have consistently pointed to under‐treatment of trauma in racially and ethnically minoritized young people, despite a higher incidence of trauma exposure (
20).
At this time, within the context of the ongoing pediatric mental health crisis, it is unknown whether the literature base on CD diagnoses incorporates race and ethnicity data in their investigation of CD. Because race and ethnicity are dynamic constructs, “shaped by geographic, cultural, and sociopolitical forces” (
21,
22), guidance on their reporting in medical and scientific journals indicate that authors need to include clear and precise definitions of race and ethnicity. Specifically, a recent guideline on the reporting of race and ethnicity urged authors to not consider race and ethnicity “in isolation” but to ensure that they are “accompanied by reporting of other sociodemographic factors and social determinants of health, including concerns about racism, disparities, and inequities” (
21). In our own conceptualization of this manuscript, we defined race and ethnicity as
social constructs‐‐without a biological basis‐‐that emerged from systems of colonialism and use observable physical differences among people to create the hierarchies of power and oppression that constitute structural
racism. Because there continues to be heterogeneity in authors' definitions and conceptualizations of race and ethnicity, we examined how each manuscript on CD diagnoses collected data and operationalized race and ethnicity.
Furthermore, we were interested in comparing differences in the diagnosis of co‐occurring psychiatric disorders such as ADHD, PTSD, and SUDs between individuals with and without CD, recognizing that co‐occurring disorders are often underdiagnosed in racially and ethnically minoritized adolescents and young adults (
17,
18). Given the time‐sensitive and dynamic nature of the current pediatric mental health crisis, we addressed this gap in research by completing a rapid review (conducted with a scoping reviews framework) to evaluate the number of manuscripts on CD diagnoses that report race and ethnicity and co‐occurring psychiatric conditions such as history of PTSD, ADHD, and SUDs.
METHODS
Rapid reviews are a type of a knowledge synthesis in which the components of a systematic review are streamlined to produce evidence in an expedited time frame (
23). While there is no single‐validated method for conducting rapid reviews, our method was based on the Cochran Rapid Reviews Method Group guidelines for setting the research question, determining eligibility criteria, searching databases, selecting studies, extracting data, assessing risk of bias, and synthesizing results (
23). We used a scoping review framework due to our broad aim of assessing how a heterogeneous literature base on CD diagnoses incorporated racial characteristics into methods and analyses (
24).
Under a scoping review framework, we defined study eligibility criteria based on the PCC mnemonic (Population, Concept and Context) (
24), as our study identified manuscripts containing any racial or ethnic data on children who received diagnoses of CD and peers without diagnoses of CD. The population of interest was children engaged in mental health care. The concept was the diagnosis of CD (vs. no diagnosis of CD). With regards to context, we were interested in assessing the reporting of racial and ethnic characteristics between people with and without a diagnosis of CD.
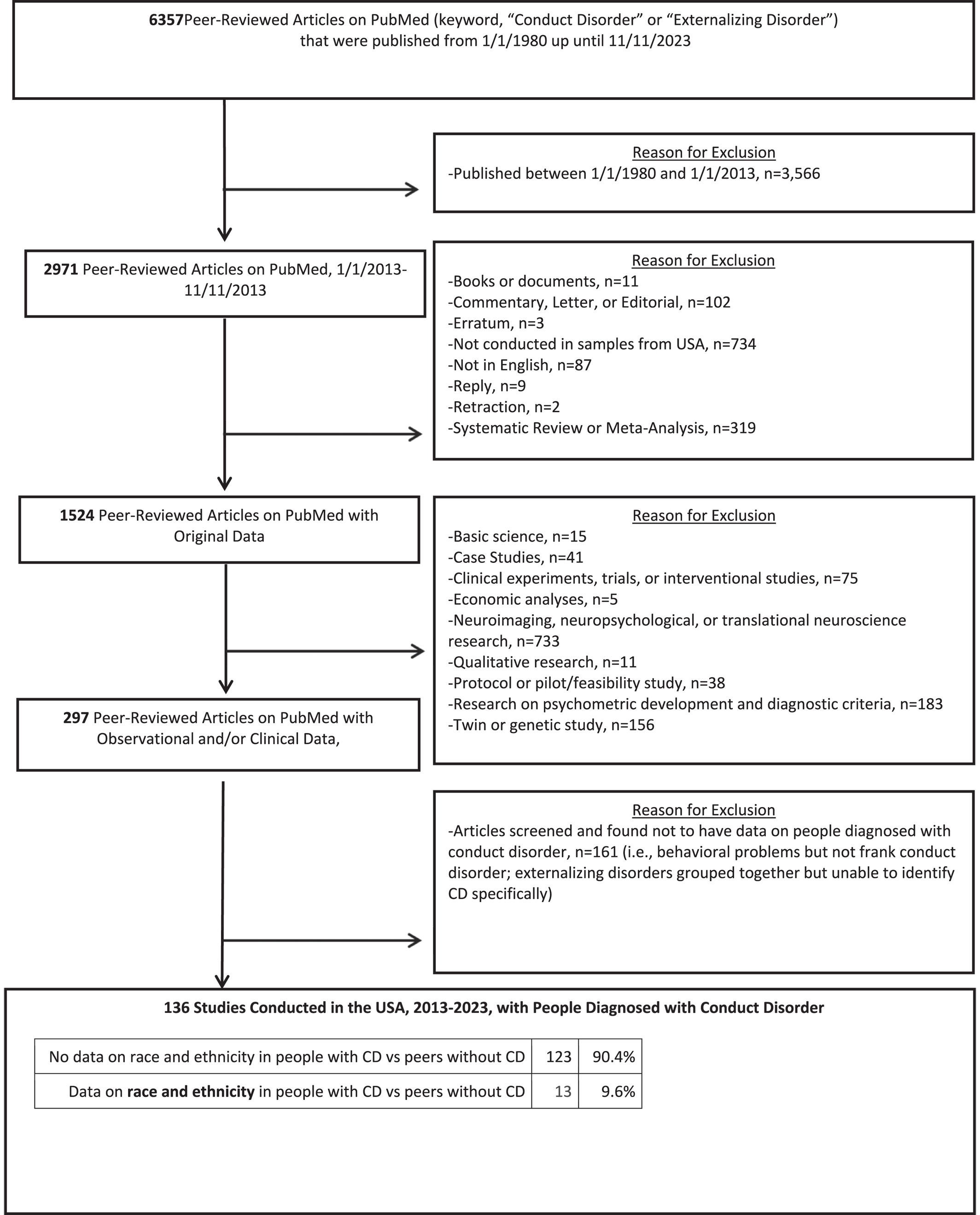
As shown in
Figure 1, we used the search term “conduct disorder” or “externalizing disorder” and screened all peer‐reviewed articles in PubMed and MedLine, including case reports and series, clinical trials, editorials and perspective articles, observational studies, meta‐analyses, and systematic reviews. We selected the time period of 2013–2023, which aligns with data showing trends in pediatric admissions for behavioral disorders in the last 10 years (
1). Because we were interested in the influence of structural racism in the US on diagnoses of CD, we limited studies to those conducted in the US, taking into account that presentations for CD may vary significantly across different cultures (
10). We excluded all studies that did not include primary data collected from patients on CD diagnoses (i.e., meta‐analyses, systematic reviews, protocols, and letters).
One reviewer (KYX) screened 2971 abstracts, culminating in 297 peer‐reviewed articles on PubMed with observational and/or clinical data, whose full‐text manuscripts were reviewed. Out of the 297 articles, potentially relevant manuscripts were reviewed with a second author (TRB). Disagreements surrounding study eligibility were resolved via discussion between the two reviewers, with the reviewers erring on the side of inclusion. We conducted the search strategy twice, first on October 13, 2023 (January 1, 2013 to October 13, 2023, averaging approximately 100 manuscripts screened per day) and again on November 11, 2023 (January 1, 2013–November 11, 2023). Because 161 of the 297 articles were excluded after they were found to not have data on people diagnosed with CD, such as studies evaluating individual behavioral problems but not frank CD. This culminated in 136 clinical studies conducted in the US from 2013 to 2023 featuring individuals diagnosed with CD. The two authors (KYX, TRB) compiled data on racial and ethnic demographics and clinical characteristics, by searching each manuscript for key words such as “conduct disorder,” “externalizing,” “externalizing disorder,” “race,” “ethnicity,” “trauma,” “substance,” “ADHD,” “attention,” “stress,” “adverse,” and “dysregulation.” We evaluated whether studies reporting race and ethnicity (a) provided justification for why race and ethnicity was collected, (b) explained how data on race and ethnicity was collected (i.e., self‐reported data; data reported by clinician; assessed and reported by administrative personnel), and (c) differentiated between race and ethnicity (i.e., defining Hispanic ethnicity and Black race as categories that are not mutually exclusive). Finally, we evaluated whether manuscripts used the term “racism” at any point in the manuscript, as guidance on the reporting of race and ethnicity data encourages authors to include the implications of historical injustices when describing potential racial and ethnic disparities, with Introduction and Discussion sections of manuscripts recommended to discuss the role of “racism” when appropriate (
21).
Further, each manuscript was screened for data on whether each study contained data on history of trauma (i.e., adverse childhood experiences; acute stress disorder; PTSD; history of abuse with or without a clinical traumatic stress disorder diagnosis), ADHD, and SUDs, as they are comorbid with CD diagnoses and undertreated in racially and ethnically minoritized children. As a Rapid Review, our protocol did not require institutional review board approval. For all studies featuring primary data on patients with CD diagnoses, we not only screened but reviewed and discussed each full‐text manuscript for data on the racial and ethnic characteristics of people with and without CD diagnoses.
RESULTS
Summary of Study Characteristics
We used the keyword “conduct disorder” and screened all peer‐reviewed articles in PubMed published from January 1, 2013 up until November 11, 2023. In total, we identified 13 papers (
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37) that differentiated between the racial characteristics of people with and without CD diagnoses, whose detailed characteristics are shown in Supporting Information
S1: eTables 1 and 2. The characteristics of included studies are shown in
Table 1. The sample sizes of included studies ranged from 225 to 442,824 individuals, with a median sample size of 1480 individuals. Included study designs and geographic regions spanned nationally representative surveys, multi‐state administrative data research, as well as single‐site clinical cohorts in individual states and cities (i.e., Chicago, Pittsburgh). There were no studies containing data collected after 2016, with five studies using data collected as early as the 2000–2010 periods.
The age ranges of study participants were largely older than 10 years of age, and only two studies provided details on heterogeneous subtypes of CD diagnoses (i.e., adolescent onset, early onset) (
26,
32). No studies provided detailed information on the heterogeneous nature of CD diagnoses, with regards to the presence of callous‐unemotional traits specifiers (
38).
Reporting of Race and Ethnicity
The majority of studies explained why racial and ethnic data were included in the manuscript, yet none reported in detail how data on race and ethnicity were collected. As shown in
Table 1, approximately one‐third of studies differentiated between race and ethnicity. Whereas some studies only differentiated between “White” and “non‐White” samples (
29,
31), others used binary characterizations of “African American” and non‐African American peers (
34) (or “African American” and “European American” peers) (
35,
37). One study focused on only Native American and non‐Native American cohorts (
30).
Despite the limitations of the evidence base, included studies consistently found that CD diagnoses were more prevalent in Black patients than White peers. For instance, an analysis of the National Inpatient Sample (one of the largest databases of discharge data in the US) found that Black children were overrepresented among people with CD diagnoses at a rate of nearly 2‐fold compared to children in other racial groups (
33). We observed similar results in an analysis of the Collaborative Psychiatric Epidemiology Studies (a series of population‐based nationally representative surveys), which illustrated an overrepresentation of Black young adults among those diagnosed with both life‐course persistent and adolescent‐limited CD diagnoses.
Only a minority of studies compared socioeconomic characteristics such as income (
27,
32,
33,
34), education (
28,
32), and criminal legal system involvement (
25,
34) between the CD diagnosis and non‐CD diagnosis cohorts, even though inequities in income, education, and incarceration often represent manifestations of structural racism. The overwhelming majority of studies did not mention the term “racism” in the manuscript.
Reporting of Co‐Occurring Psychiatric Problems
We reviewed each study for detailed clinical information on history of trauma, substance use, and developmental disorders (i.e., ADHD) that are prevalent in people with CD diagnoses yet diagnosed inequitably between White and Black children. Only three papers compared CD diagnosis and non‐CD diagnosis cohorts with regards to potential history of trauma, assessed as adverse childhood experiences (
25), Childhood Trauma Questionnaire scores (
34), and potentially traumatic events and interpersonal trauma (
27). In an analysis of the National Comorbidity Survey Replication‐Adolescent Supplement, multivariable models (adjusting for demographics and parental psychopathology) showed that interpersonal trauma and potentially traumatic events were strongly associated with increased risk for receiving CD diagnoses (
27). Similarly, in an analysis of young adults with prenatal cocaine exposure, higher scores in childhood trauma questionnaires correlated with increased likelihood of conduct disorder diagnoses (
34).
Overall, seven papers compared the CD diagnosis and non‐CD diagnosis cohorts with regards to substance use‐related data, with relatively few papers analyzing the prevalence of specific substance‐related exposures such as marijuana (
28,
29,
34), cocaine (
29,
34), and alcohol (
28,
34,
35) across the CD diagnosis and non‐CD diagnosis group. Only one study assessed opioid and amphetamine use (
29). Included studies consistently showed a strong correlation between SUD and CD diagnoses. For instance, CD diagnoses were strongly associated with onset of alcohol use disorder (as well as time to first intoxication and regular drinking) (
35), cannabis consumption and positive attitudes towards drug use (
31), and problematic stimulant use (
29). While racial differences in the diagnosis and treatment of SUDs were outside the scope of included studies, a study by Sartor and colleagues emphasized the need for research that consider sociocultural factors that “disproportionately impact racial and ethnic minorities, including poverty and discrimination,” and may influence substance use‐related outcomes (
35).
With regards to developmental disabilities, one study collected data on rates of learning disability (
32), but comparison of the CD diagnosis and non‐CD diagnosis samples was likely limited by low statistical power. Separately, an analysis of Florida juvenile justice data by Baglivio and colleagues (a dataset encompassing over 10,000 detainees) did not compare ADHD diagnosis rates between the CD diagnosis and non‐CD diagnosis samples, but the authors noted that White male detainees were more likely to receive ADHD diagnoses than Black peers (
25). While we posited that an examination of whether racial inequities in ADHD diagnosis was a determinant of racially inequitable CD diagnoses was outside the scope of Baglivio et al.’s analysis, the study noted that Black male detainees were 32% less likely to receive psychiatric treatment than White detainees (
25).
DISCUSSION
Overall, this analysis illustrates an underreporting of race and ethnicity data in the CD diagnosis literature, with included studies raising concern for racial inequities in the diagnosis of CD between Black and White children and adolescents in the US. While the problem of underreporting race and ethnicity is not unique to child and adolescent psychiatry (
39), data on racial characteristics have unique relevance to CD diagnoses given CD's correlation with criminal legal system involvement among minoritized children. The present article also underscores the need for up‐to‐date epidemiologic data collection on the burden of psychiatric comorbidities in children and young adults with CD diagnoses. Our included manuscripts illustrate that CD diagnoses is consistently associated with a past history of trauma and SUDs. However, no studies, based on our review, thoroughly assess how minoritized stress and racialized trauma (
20,
40) may influence CD diagnoses, even as studies show that prenatal, familial, and early life exposure to socioeconomic deprivation have negative consequences for child development (
41,
42,
43). This is an important research gap, as it is difficult to develop interventions to improve mental health outcomes among minoritized children diagnosed with CD if we do not have up‐to‐date data on potential unmet treatment needs. Specifically, the reporting of race and ethnicity in future studies of CD diagnoses is necessary to ensure that research on CD addresses rather than perpetuates health inequities. After all, if racial and ethnic disparities in pediatric and adolescent mental health outcomes are to be eliminated, it is important to find ways to identify and study these disparities.
Recognizing that CD's diagnostic criteria experienced minor modifications from DSM‐IV to DSM‐V (i.e., the addition of specifiers such as limited prosocial emotions, lack of remorse or guilt and callous traits), older data do not necessarily disqualify the internal validity of a study. However, our scoping review illustrates that the majority of studies published on CD diagnoses in the last decade use data from the early 2000s and 2010s. The age of the CD evidence base raises concern about generalizability of existing studies to the current treatment landscape in the US. Especially since our included studies showed a correlation between CD diagnoses and substance‐related problems, the ongoing surge of problematic substance use in young adults in the US underscores the need for up‐to‐date data on the mental health outcomes of children with CD diagnoses in the US.
Finally, the reporting the racial and ethnic characteristics of patients with and without CD diagnoses in research studies is an important first step towards addressing the unmet mental health needs of children diagnosed with CD. CD remains a diagnosis that is made by evaluating the violation of age‐appropriate societal rules, norms, and laws in children, a process that can be fraught with value judgments and subjectivity. Unfortunately, there remains concern for interpersonal and structural racism impacting the subjective process of evaluating conduct problems in children. For instance, a recent study showed that predominantly White teachers endorsed greater burden of conduct problems in Black children with ADHD compared to White peers even though Black caregivers endorsed fewer or similar number of symptoms as White caregivers (
44), despite studies showing that cardinal ADHD symptom profiles are similar for Black and White children (
45). Other analyses suggested that while many Black children may have a higher symptom burden for ADHD, based on questionnaires than White patients, they were less likely to have been clinically diagnosed (
17). Against this backdrop, the present study's findings are consistent with literature raising concern about how existing models for psychiatric disorders may benefit from more rigorous integration of historical and social context. For instance, in the child psychiatry realm, important efforts have been made to revise diagnostic criteria for oppositional defiant disorder (
46), recognizing that diagnoses of externalizing behavior may incorrectly pathologize trauma responses in minoritized people while drawing attention away from important structural contexts. Before we can take similar steps for CD, more comprehensive racial and ethnic and clinical data from patients with CD diagnoses first needs to be collected.
There are several important limitations to consider. First, we only identified 13 manuscripts on CD diagnoses that contained data on the racial and ethnic characteristics of patients diagnosed with CD. While we ideally sought to pool the findings of each manuscript together and assess racial and ethnic differences in the rates of CD diagnoses, we found that the 13 identified manuscripts on CD diagnoses had such heterogeneous research questions, study designs, and methods that a meta‐analysis is not feasible. Second, there are inherent limitations to conducting rapid reviews. While they are well suited for time‐sensitive and dynamic topics, such as the crises of structural racism in the US and the co‐occurring pediatric mental health crisis, our rapid reviews was limited by the use of a streamlined review method focusing on only studies conducted in samples in the US. We did not register our review on PROSPERO or assess every paper's study quality using a formal instrument.
Clinical Implications
Amid the youth mental health crisis, a growing number of children and adolescents present to acute care facilities where they carry diagnoses of CD. However, data on the racial and ethnic characteristics of children with CD is sparse, even though there is growing concern for racial and ethnic disparities in CD diagnoses. Because diagnoses of CD may increase the likelihood of criminal legal system involvement, clinicians should be cautious to not perpetuate diagnostic bias and contribute to the criminalization of externalizing behaviors when children with diagnoses of CD present for care. Particularly in fast‐paced acute care settings, where clinical teams rely heavily on the electronic health record for diagnostic history and context, it is important to verify previous mental health diagnoses rather than assuming them to be true, particularly for minoritized children. Overall, our analysis suggests that clinicians, policymakers, and public health practitioners have an opportunity to address structural racism by incorporating a more intentional approach to collecting race, ethnicity, and socioeconomic data and interpreting its findings.
CONCLUSION
In summary, this rapid review, conducted with a scoping reviews framework, illustrates that there is no shortage of manuscripts on CD diagnoses in the last 10 years. Yet, the vast majority of manuscripts on CD diagnoses lacked demographic data on patients' racial and ethnic characteristics. Most manuscripts lacked information on prior history of co‐occurring psychiatric disorders like PTSD, ADHD, and SUDs that can manifest as externalizing disorders and are undertreated in racially and ethnically minoritized children. The lack of reporting on race and ethnicity in children with CD diagnoses represents a cross‐cutting priority for future research in the US, especially amid surging volumes of children presenting to acute care settings for behavioral disorders and overrepresentation of minoritized youth in juvenile justice settings.