Research has shown that negative stereotyping and discrimination toward people with a mental disorder are experienced by their family members as well as by the individuals afflicted (
1). For example, Struening and colleagues (
2) found that 40% to 79% of 461 family members of mental health consumers with a diagnosed serious mental illness agreed that “most people” devalued family members. Research has also documented that family members tend to internalize the devaluing views of others, which is referred to as self-stigma and is reflected in feelings of guilt or self-blame in relation to the relative's illness. Studies have found that feelings of guilt or self-blame characterized up to 50% of family members (
3–
7) and that self-stigma was associated with low self-esteem (
8,
9), secrecy, or social withdrawal in response to anticipated rejection (
4,
10,
11), psychological distress (
12,
13), and subjective burden (
14). Although several interventions to reduce self-stigma among consumers have been described (
15–
20), no intervention targeting self-stigma among family members has been reported.
We present preliminary data from a novel intervention designed to reduce self-stigma among family members of individuals with serious mental illness. This intervention, In Our Own Voice-Family Companion (IOOV-FC), is a single session modeled after “In Our Own Voice” (IOOV), a widely disseminated program and manual developed by the National Alliance on Mental Illness (NAMI) to reduce public stigma toward mental health care consumers. Like IOOV, IOOV-FC features two family members who describe the process of learning to cope with mental illness through sharing their own experiences and those of other family members featured on a videotape. With this approach, IOOV-FC aims to disconfirm negative, internalized stereotypes held by family members through interaction with family peers who model challenging discriminatory behavior and stigmatizing beliefs rather than internalizing them.
This article first reports on the development of IOOV-FC. We then present our evaluation of the intervention's preliminary efficacy in reducing family self-stigma compared with a provider-delivered family education session. Second, we evaluate the efficacy of IOOV-FC in comparison with family education in altering interpersonal strategies commonly adopted to cope with the adverse impact of discrimination: secrecy and withdrawal (
21). Third, we examine potential moderators and mediators of treatment response, specifically the role of anxiety as a moderator and social comparison as a mediator of outcome. Family members of individuals with mental illness often report acute distress, anxiety, or fear (
22,
23). Because high anxiety has been associated with poorer response to psychosocial treatments for depression (
24–
29) and depression is common among caregivers of people with mental illness (
30–
32), it seems plausible that elevated pretreatment anxiety may be associated with poorer response to IOOV-FC. Anxious persons may experience social anxiety in a group setting when asked to share personal stories with strangers and withdraw, compromising their ability to benefit from an intervention designed to alter self-cognitions through exposure to, and comparison with, the viewpoints and coping strategies used by others. Festinger (
33) observed that people have a tendency to “evaluate their own opinions and abilities by comparison respectively with the opinions and abilities of others,” which he termed “social comparison.”
We hypothesized first that family members participating in a peer-led intervention focused on learning to cope with mental illness stigma (IOOV-FC) would report greater reductions in self-stigma than family members participating in clinician-led education about various aspects of mental illness. Second, we hypothesized that family members participating in IOOV-FC would report greater reductions in the use of secrecy and withdrawal than those participating in family education. Third, consistent with the results of prior studies, we hypothesized that reductions in self-stigma, secrecy, and withdrawal would be moderated by family members' preintervention anxiety level, with the advantage of IOOV-FC versus family education most evident for family members with low to moderate anxiety. Finally, on the basis of the literature on social comparison, we anticipated that hypothesized decreases in self-stigma, secrecy, and withdrawal associated with assignment to IOOV-FC would be mediated by decreases in social comparison during the intervention.
Methods
Participants
A total of 158 caregiver participants were recruited from the inpatient and outpatient psychiatric services of a large, metropolitan hospital center in the Northeast (N=93) and from the Connecticut chapter of the National Alliance for Mental Illness (NAMI-CT) (N=65). At the hospital, clinicians referred all consumers with diagnosed schizophrenia and an eligible caregiver to the study team. At NAMI-CT, family members were recruited via fliers or self-referral after announcements at support group meetings. To be eligible, caregivers had to be age 18 or older and the primary caregiver of a relative who met
DSM-IV criteria for a schizophrenia spectrum disorder based on chart diagnosis. We chose to focus on schizophrenia in this preliminary study to reduce heterogeneity of results from potentially differing experiences of family members whose relatives have diagnoses of other disorders. The primary caregiver met at least three of five criteria established by Pollak and Perlick (
34): being a spouse or parent, having more frequent contact than any other caregiver, helping to support the patient financially, being contacted by treatment staff for emergencies, and having been involved in the patient's treatment. In addition, caregivers had to be a first-degree relative of the patient and show evidence of perceived stigma, operationalized as scoring positive on at least two of the seven items on the Struening and colleagues (
2) Devaluation of Consumer Families Scale.
Of 221 caregivers referred, 65 (71%) of 92 caregivers referred from NAMI-CT and 93 (72%) of 129 caregivers referred from the hospital (47% of caregivers of all patients approached) agreed to participate and met inclusion criteria (N=158). All caregivers screened met inclusion criteria for perceived stigma. The study was approved by the facilities' institutional review boards; after complete description of the study to participants, written informed consent was obtained. Consenting caregivers were assessed and randomly assigned to receive one of two group interventions: a peer-led intervention (IOOV-FC) designed to stimulate group discussion, disclosure, and social comparison or a clinician-led family education session that delivered information about mental illness in a structured, didactic format. Caregivers were assessed and randomly assigned to treatment condition within the two-week period before the scheduled group meeting. We assessed 122 (77%) of consenting caregivers, who were randomly assigned to a study condition and participated in the intervention and postassessment; 23% were unable to be scheduled or contacted, and their data were thus lost to the study. Participant recruitment and data collection took place between September 2008 and April 2010.
Measures
Caregivers were assessed before randomization and immediately posttreatment on all measures described below. Posttest assessments were performed by an independent evaluator who was blind to the study's treatment condition.
To measure changes in caregiver self-stigma, we used a modified version of the seven-item Devaluation of Consumer Families Scale (
2), which measures perceptions of discrimination and devaluation directed toward families by the general public. The modified scale applies the method described by Corrigan and colleagues (
35,
36) for assessing stereotype endorsement and stereotype self-concurrence (that is, self-stigma) to each of the Struening and colleagues (
2) items. For each item, a corresponding “stereotype agreement” and “self-concurrence” item was developed. For example, for the public stigma item “Most people would rather not be friends with families that have a relative who is mentally ill living with them,” the corresponding stereotype agreement item was “People are justified in not wanting to be friends with people who have a mentally ill relative living with them,” and the corresponding self-concurrence item was “I sometimes feel that others are justified in not befriending me because I live with a family member who is mentally ill.” These items were reviewed by both Corrigan and Link and were piloted on ten family members to ensure clarity and acceptability. The seven stereotype agreement items and the seven self-concurrence items were then combined to produce a 14-item self-stigma scale, which had good internal consistency (
α=.84). Secrecy and withdrawal were assessed with Link and colleagues' (
21) scales. The secrecy scale is a five-item Likert scale assessing use of concealment of mental illness (for example, “If you have been treated for a serious mental illness, the best thing to do is to keep it a secret”) (
α=.72). The withdrawal scale consists of seven items assessing “limiting social interaction to those who know about and tend to accept one's stigmatized condition,” such as, “If I thought someone I know held negative opinions about psychiatric patients, I would try to avoid him or her” (
α=.57). Baseline self-stigma was modestly correlated with both secrecy (r=.209, p=.021) and withdrawal (r=.233, p=.010), which were significantly intercorrelated (r=.479, p<.001) as well.
Anxiety and social comparison were assessed with the Brief Symptom Inventory (BSI) (
37) anxiety scale (
α=.85) and the 11-item, Iowa-Netherlands Comparison Orientation Measure (
38) (
α=.83), respectively. The latter scale was developed to measure social comparison, a term coined by Festinger (
33) to describe the tendency to evaluate one's opinions and abilities through comparison with others (such as “find out what others think who face similar problems as I do” or “how well I have done something”). Higher numbers reflect higher social comparison (
38).
IOOV-FC intervention
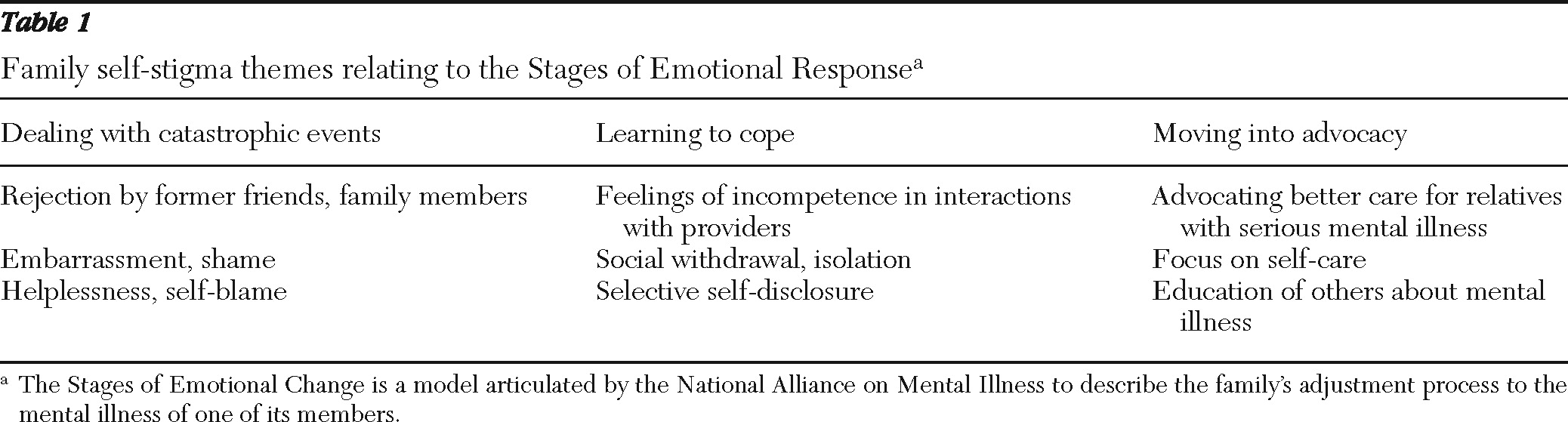
IOOV-FC consisted of a 15-minute videotape of family members describing their experiences in adjusting to having a member with mental illness, followed by a 60-minute group discussion facilitated by two family peers. The family members in the video shared their experiences coping with stigma associated with mental illness using the framework of NAMI's Stages of Emotional Response, where stage 1 is dealing with catastrophic events, when the illness symptoms first emerge; stage 2 is learning to cope, which involves understanding the illness and its management; and stage 3 is moving into advocacy through practicing self-care and confronting stigma in one's daily life and through public advocacy (
Table 1). Group discussion was elicited after the video clip on each Emotional Stage, as well as at the end of the video. Both the video and group discussions focused on self-stigma themes identified in focus groups conducted with family members and consumers.
The acceptability of the video production was evaluated by 24 family members and ten consumers using 4-point Likert scales on 17 items assessing the degree to which the production was culturally sensitive, respectful of different stakeholders, and reflective of families' stigma experiences. Higher scores reflect higher acceptability. Internal consistency of the 17 items was good (α=.92); 96% (N=23) of participants rated all items above a predetermined acceptability threshold. The mean±SD score on the total scale was 3.60±.24. Twelve family members who had facilitated or attended NAMI's signature peer education program, Family-to-Family, were chosen as facilitators for IOOV-FC and participated in a two-day, intensive training program that covered defining caregivers' experience of stigma at each of NAMI's Stages of Emotional Response, guidelines for self-disclosure, and group facilitation skills.
Family education condition
The family education condition was a 75-minute educational presentation on mental illness, its treatment, family impact, and resources and was delivered by two mental health providers in a clinical setting. Education was delivered via videotape and PowerPoint presentation, and group interaction was limited to questions from participants, with answers provided by the clinician.
Ten groups of four to eight family participants each were conducted for IOOV-FC (N=59) and for family education (N=63). A video recording was made of every third group, and four IOOV-FC tapes were rated for adherence and competence by the NAMI principal investigator and a master's-level clinician. The rating scale, which was developed for this study, included 17 items on adherence and seven items on competence. Across the four sessions rated, 94% of all items were rated at or above a preselected adherence threshold. Raters' scores differed by no more than 1 point for 91% of adherence items and 96% of competence items. The overall interrater reliability (Pearson's r) was .959 for adherence and .988 for competence.
Data analysis
All 122 participants who attended their assigned treatment group completed the posttreatment assessment. All principal analyses were conducted based on the intention-to-treat principle and used all available data for analysis. First, the treatment and control groups were compared on ten pretreatment sociodemographic and clinical characteristics by using t, chi square, or Fisher's exact tests. Next, linear regression models were used to evaluate the effect of treatment group on outcome variables. Each variable measured at posttreatment was regressed onto treatment group assignment, followed by the respective pretreatment value for that variable. In this analytic approach, the group effect was the test of the difference between the two groups posttreatment, with controls for pretreatment levels.
The model described above was computed again, with the interaction between treatment group and pretreatment anxiety level added as the final entry, in order to evaluate the hypothesis that treatment effects would be strongest for family members with low to moderate levels of baseline anxiety. Where a significant effect of group or group × anxiety level interaction was observed, we used exploratory models to evaluate social comparison as a mediator of treatment-related changes, in each case adding either the interaction between group and the pretreatment-posttreatment change in the hypothesized mediating variable as well as its pretreatment value or the pretreatment value and the pretreatment-posttreatment value alone (
39) after the group × anxiety level term had been entered.
Results
Sample characteristics
Of the 122 participants randomly assigned to receive the IOOV-FC intervention or the control treatment, all were available for postassessment.
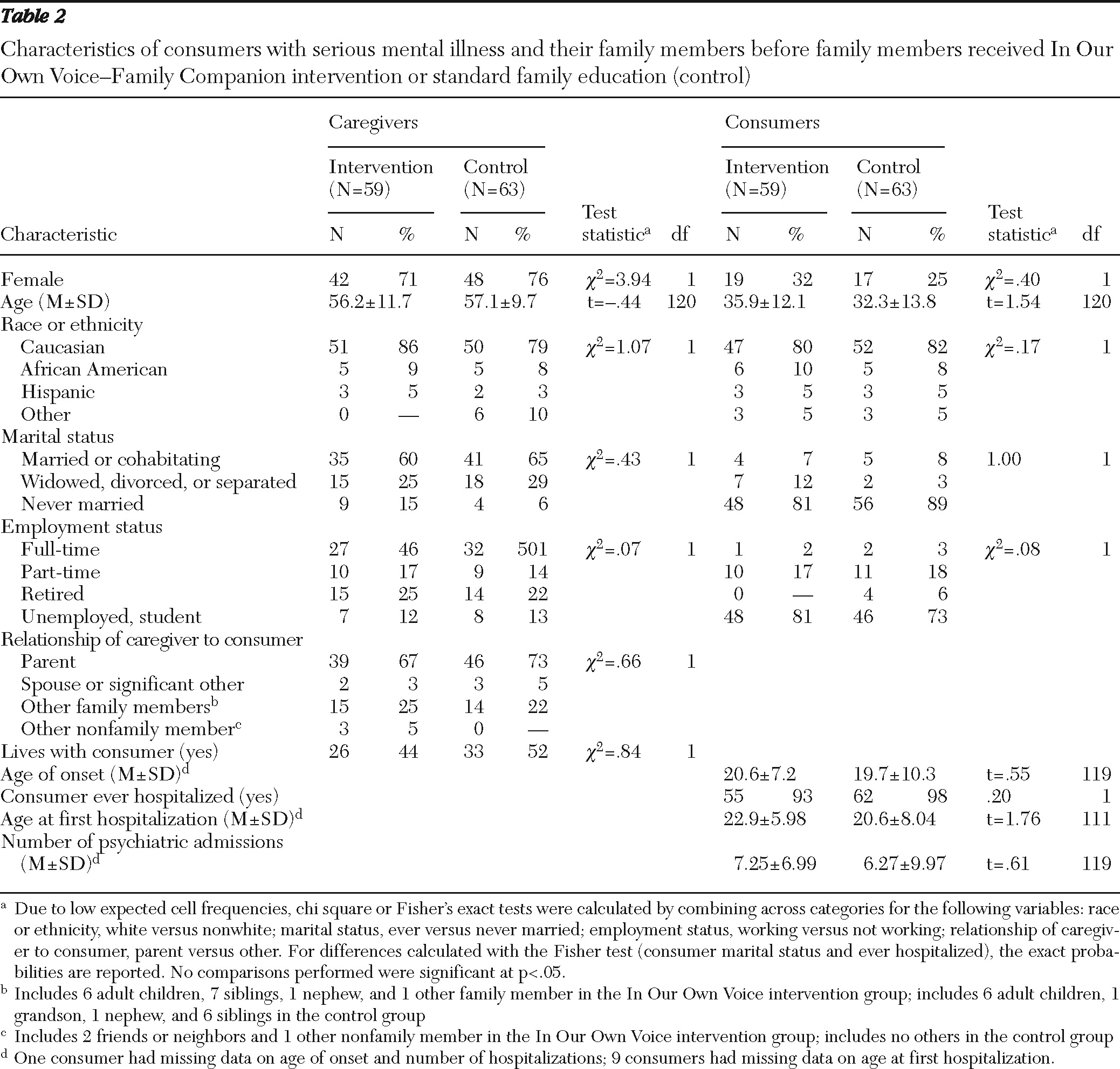
Table 2 displays the pretreatment sociodemographic and clinical characteristics of the study sample. No significant differences between treatment groups were observed before the onset of treatment on any of ten caregiver and patient sociodemographic variables.
Patient and caregiver treatment outcomes
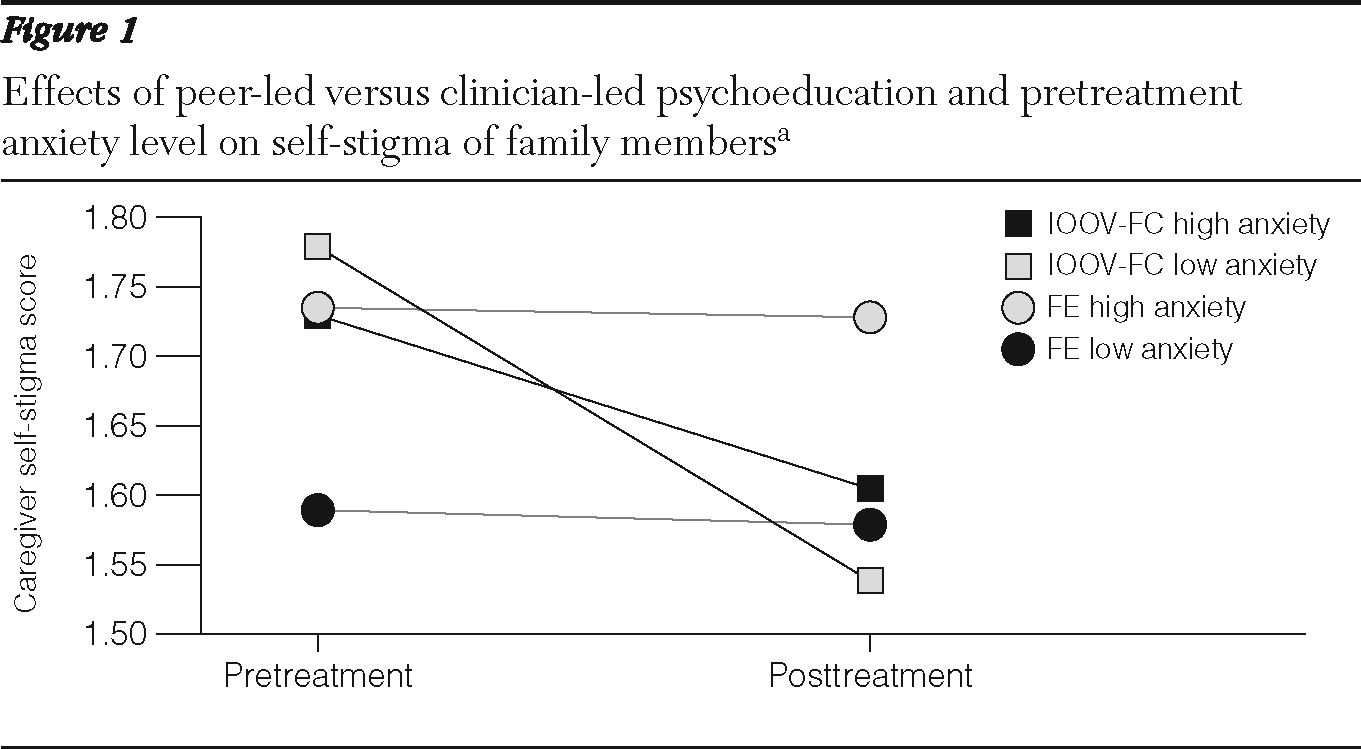
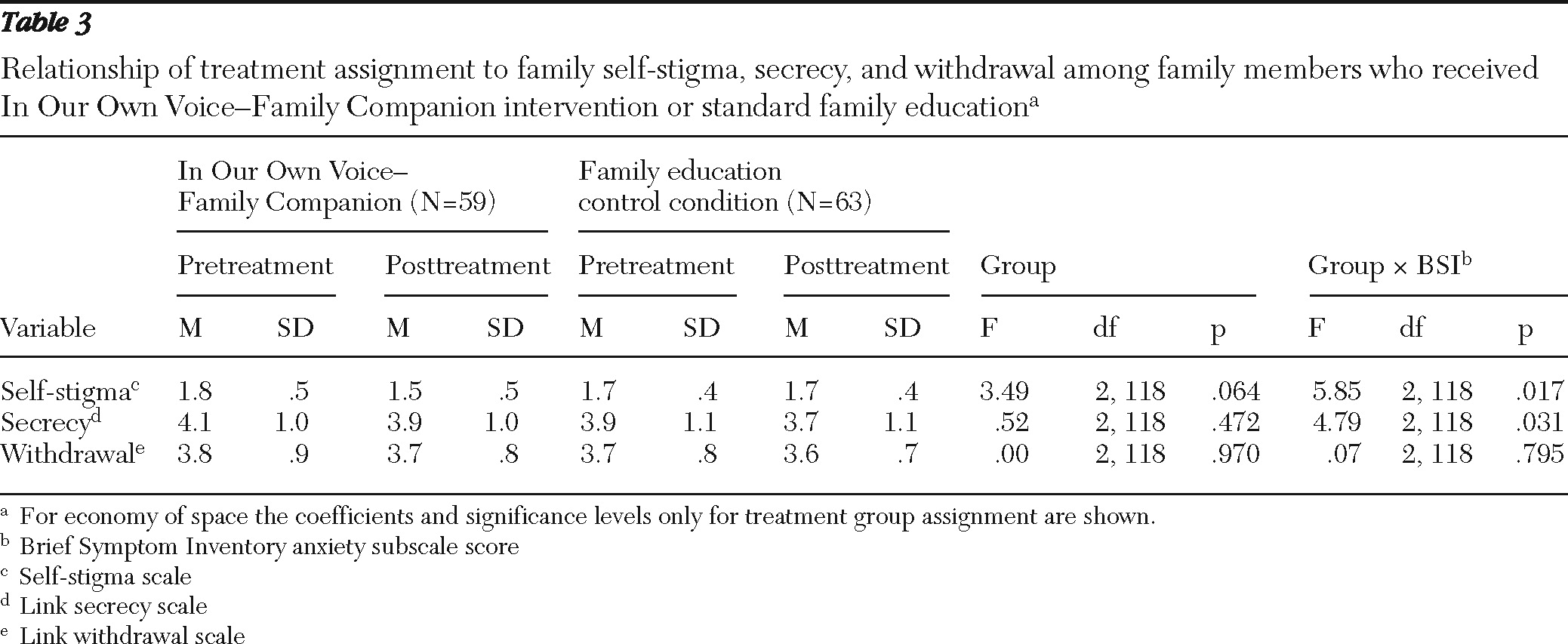
Table 3 summarizes the results of the regression analyses of family outcome variables by treatment group assignment. In addition to the group effect, the group × anxiety level interaction effect is reported. Although the group effect for self-stigma approached significance (p=.064), none of the models found a significant effect for treatment group alone. However, significant interactions between group and pretreatment anxiety level were observed for two outcomes. For self-stigma, a significant interaction was observed in which the IOOV-FC group overall showed some reduction in reports of self-stigma (F=5.85, df=2 and 122, p=.017), but the reduction was greatest for those with low to moderate versus high levels of pretreatment anxiety (
Figure 1). By contrast, for the family education group, reports of self-stigma postintervention were virtually identical to those reported preintervention (
Figure 1) and were not influenced by level of anxiety (pretreatment BSI score × pre-post self-stigma Pearson r=.038). The effect size observed for participants with low to moderate anxiety was in the medium range (Cohen's d=.50), whereas the effect was considered small for participants with high anxiety (d=.21). A significant group × pretreatment anxiety interaction was also observed for secrecy (F=4.79, df=2 and 122, p=.031). In the IOOV-FC group participants with low to moderate levels of anxiety reported a modest decrease in secrecy (d=.20), whereas participants with high anxiety reported a comparable increase in secrecy (d=.19). Pretreatment-posttreatment changes in stigma were not significantly associated with changes in secrecy (r=−.310, p=.738) or withdrawal (r=−.162, p=.076), although changes in secrecy and withdrawal were significantly correlated (r=.276, p=.002).
The term for changes in social comparison observed during the intervention (pretreatment-posttreatment social comparison) was significant when examined in the exploratory model evaluating the role of social comparison as a mediator of changes in self-stigma (F=6.15, df=1 and 115, p=.015 ). Lower levels of self-stigma posttreatment were associated with greater reductions in social comparison. The associated increase in explanatory power (from an adjusted R2 of .332 to .366) was also significant (Fchange=6.11, df=1 and 115, p=.015).
Discussion
This article reports on the development and preliminary findings of IOOV-FC, a novel intervention designed to reduce family self-stigma. Developed in collaboration with NAMI-CT, IOOV-FC was structured to promote interaction with family peers who had successfully negotiated many of the difficulties and emotional strains confronting study participants. IOOV-FC was hypothesized to reduce self-stigma, secrecy, and withdrawal through stimulating social comparison processes that would inspire participants to reappraise their ability to cope with discrimination and rejection experienced in interactions with others. Our findings indicate that the intervention was acceptable and feasible. Family members with low to moderate levels of preintervention anxiety who were assigned to IOOV-FC reported significant reductions in self-stigma and secrecy relative to those assigned to the family education control group, and reductions in self-stigma were partially mediated by reductions in social comparison.
Although our findings are consistent with the literature, it is of concern that caregivers with high levels of anxiety showed only a small reduction in self-stigma in contrast to the more robust reduction observed for caregivers with low to moderate anxiety. Future trials should modify the intervention to address the stigma concerns of these caregivers as well. Caregivers with high anxiety may refrain from full group participation for fear of being judged or embarrassed. Consistent with this speculation is the slight increase in secrecy observed among these caregivers. In studies of evidence-based psychosocial interventions, consumers with co-occurring anxiety symptoms took longer to achieve a therapeutic response (
24–
27), suggesting that caregivers with high anxiety might respond more favorably to IOOV-FC with additional sessions, allowing sufficient exposure to disconfirm anticipated threats (such as fear of shaming or embarrassment) and to increase receptivity to cognitive-informational and affective-supportive aspects of IOOV-FC. It is also possible that they would benefit from inclusion of stress reduction tools or strategies from evidence-based interventions for anxiety. Qualitative methods might be used to determine specific needs of caregivers with high anxiety that are not addressed by the current intervention.
The finding that changes in self-stigma were not associated with changes in secrecy or withdrawal despite significant intercorrelations pretreatment and in prior work (
29) may be attributable to differences in sampling (that is, mental health or support group versus a community setting) or to the use of specific intervention strategies. For example, group leaders supported use of both secrecy and selective disclosure, depending on the situation.
The finding that reductions in self-stigma in IOOV-FC were partially mediated by reductions in social comparison suggests that learning more effective strategies for coping with public stigma and the tendency to internalize negative stereotypes decreased participants' need to seek information from, or evaluate their abilities in relation to, the perceived successes of other family members, resulting in reductions in both self-stigma and social comparison from pretreatment to posttreatment relative to reductions observed for the control group.
The availability of a very brief intervention that can help reverse the internalization of mental illness stigma for families is important for several reasons. First, as noted above, self-stigma adversely affects the self-esteem, social lives, and psychological health and well-being of family members of persons with mental illness (
8–
12). Second, in practice, family members who feel ashamed, to blame, incompetent, or who make other internal attributions for their relative's illness may be less likely to take constructive actions on his or her behalf. Family members play a critical role in promoting their relative's entry into and adherence to mental health treatments (
40–
45) but are often deterred by fear of exposure to stigma and blame from providers, friends, or other family members (
6,
46).
Although these initial results are promising, it will be critical to see whether they are sustained over time. A limitation of the study is the relatively low proportion of caregivers from diverse ethnic and racial backgrounds, which limits generalizability. Only 18% of caregivers and 19% of consumers were from racial or ethnic minority groups. Because stigma may serve as an especially profound barrier to care for individuals from these groups (
47,
48), it will be critical to build in measures to increase diversity in future studies.
Conclusions
The results of this study suggest that peer-delivered interventions may represent a more effective way to reduce self-stigma than provider-delivered education. Future studies should address the needs of caregivers with high anxiety levels and from racial and ethnic minority groups.
Acknowledgments and disclosures
This study was supported by grants R01 MH077168 and R01MH077169 from the National Institute of Mental Health. The authors gratefully acknowledge the support and guidance of and offer a special thanks to the peer facilitators from the Connecticut chapter of the National Alliance on Mental Illness and family members and mental health consumers who participated in this study. Finally, the authors thank Christina DeFranco of Danolas Productions for her inspired video representation of the personal accounts of family members learning to cope with having a relative with mental illness.
The authors report no competing interests.