Wellness Recovery Action Planning (WRAP) is an illness self-management intervention with an educational component that promotes healthy living and a psychological component that involves peer support. It is widely used by people with diverse mental health diagnoses and other disabilities, economic circumstances, and cultural backgrounds (
1). WRAP helps participants identify personal wellness resources and how to use them in daily living, as well as deal with symptom triggers, early warning signs of illness exacerbation, and crisis periods (
2). People typically develop WRAP plans while attending a WRAP group facilitated by trained, certified educators. Certification requires attendance at five-day training sessions sponsored by the Copeland Center for Wellness and Recovery along with mentoring from advanced-level WRAP facilitators who observe and provide feedback (
3).
WRAP has been widely disseminated and is offered in every U.S. state and territory, as well as in Canada, England, Scotland, Ireland, Japan, Hong Kong, New Zealand, and Australia (
4). Although its growth has been rapid, a comprehensive review of the literature identified only four published studies of WRAP outcomes (
5). A one-group pretest-posttest study in New Zealand examined outcomes reported by 187 health professionals and service users who attended a one- to two-day WRAP workshop (
6). Statistically significant improvement was found in recovery attitudes (regarding the possibility of recovery and the importance of shared decision making, for example) and knowledge (concerning the nature of advance directives and elements of peer support, for example), with no significant differences between consumers and professionals in the extent to which scores improved. A one-group pre-post study of 30 participants in a 12-week WRAP program at three mental health centers in Iowa found significant increases in hope and recovery but did not find a decreased level of symptoms (
7). A quasi-experimental study from the same authors contrasted outcomes of 58 Iowa mental health center clients who attended at least 75% of their WRAP sessions with outcomes of a matched comparison group from the same centers (
8). Results revealed significant intervention effects for reduction of psychiatric symptoms and increased hopefulness but no significant changes in self-perceived recovery. Finally, a one-group pre-post evaluation of two statewide WRAP initiatives involving 147 participants in Vermont and 234 in Minnesota (
9) found statistically significant improvement on three dimensions of self-management: positive attitudes, such as feeling hopeful about recovery and the ability to assume responsibility for one's own wellness; knowledge regarding early warning signs of decompensation and symptom triggers; and wellness skills, such as using one's social support network and following a daily plan for healthy living.
This study tested two hypotheses. The first was that intervention group participants would experience greater reduction of symptoms of depression and anxiety than participants in the control group and that this effect would be maintained over time. The second hypothesis was that intervention participants would report greater increases in self-perceived recovery than those in the control group, a change also maintained longitudinally.
Methods
Using a wait-list control design, this randomized controlled trial compared WRAP with services as usual. Participants were recruited from six Ohio communities: Canton, Cleveland, Columbus, Dayton, Lorain, and Toledo. Sites were chosen on the basis of availability of certified WRAP educators as well as minimal prior WRAP instruction in the local area. Written informed consent was obtained via procedures approved by the University of Illinois at Chicago (UIC) Institutional Review Board.
Participants
Participants were individuals with serious mental illness as defined by Public Law 102–321 specifying diagnosis, duration, and level of disability (
10). They had a
DSM-IV-TR (
11) disorder (other than substance use) of at least 12 months' duration that was characterized by “serious impairment,” defined by Ohio statute as “functional limitations on a continuing or intermittent basis in major life activities that would be appropriate for the individual's developmental stage” (
12). Screening confirmed that individuals either were enrolled in publicly funded mental health programs for clients with serious impairment or scored 13 or higher on the K-6 Screening Scale for serious mental illness (
13), or both. Other inclusion criteria were age (18 years or older), ability to provide informed consent, comprehension of spoken English, and no prior WRAP education.
Information about the study was disseminated by the Ohio Department of Mental Health, statewide consumer organizations (Ohio Advocates for Mental Health, Depression and Bipolar Support Alliance Ohio), newspaper advertisements, and notices on county mental health board Web sites. Enrollment commenced October 2006 and ended April 2008. Recruitment occurred in traditional psychiatric outpatient settings, residential programs, consumer-operated programs, and self-help groups. The study's local coordinators met with potential participants to describe WRAP and research procedures, answer questions, and help interested individuals contact UIC via a toll-free telephone number for screening and enrollment by research staff.
Of 850 individuals contacted, 295 were not randomly assigned because they declined participation, were determined to be ineligible, or did not complete enrollment procedures. The remaining 555 were randomly assigned to the control (N=279) or intervention (N=276) condition. Eleven control participants and 25 intervention participants were lost to follow-up for reasons including death or ill health, moving away from the area, or formal withdrawal from the study. Data from all other participants were included in the analysis given the desire to limit postrandomization exclusion (
14). Thus the final sample included 268 in the control group and 251 in the intervention group. Statistical power was .80 to detect a between-groups, unadjusted effect size of d=.22 for the Brief Symptom Inventory (BSI) anxiety and depression subscales. For all analyses, p<.05 was considered significant.
Procedures
UIC Survey Research Laboratory personnel who were blinded to study condition administered one-hour structured telephone interviews at baseline (time 1), two months (time 2), and eight months (time 3). Participants received a research stipend of $20 for the first interview, $25 for the second, and $30 for the third, with a $10 bonus for completing all three. Interviews were conducted via computer-assisted personal interviewing (CAPI) software.
At the end of the baseline interview, we randomly assigned respondents at the site level using a random allocation sequence programmed in the CAPI software. This method allowed for complete allocation concealment up to the point of assignment (
15) so that interviewers and respondents were unaware of the study condition until after assignment. Follow-up interviewers were blinded to study condition. To monitor the fidelity of the blind, the interviewers recorded at the conclusion of each two- and eight-month interview whether participants had revealed their actual study condition. This was found to have occurred in only 4% of all interviews.
Of the 519 participants who completed baseline assessments, 458 participants (88%) completed time 2 interviews, and 448 (86%) completed time 3 interviews. There were no statistically significant differences in follow-up rates between intervention and control conditions at either time point. Finally, there were no significant differences in completion of follow-up interviews by study site.
Measures
The primary outcome was reduction in symptoms of depression and anxiety as measured with the BSI depression and general anxiety subscales. The BSI is a patient self-report instrument showing high concordance with clinician symptom assessment and strong test-retest and internal consistency reliabilities (
16). Factor-analytic studies of the scale's internal structure have demonstrated its construct validity with a six-item depression subscale (item content included “feeling lonely,” “thoughts of ending your life,” and “worthlessness”) and a six-item anxiety subscale (items included “suddenly scared for no reason,” “feeling fearful,” and “spells of terror or panic”). All items are rated on a 5-point scale from 0, symptom not present, to 4, extremely severe. Following published BSI scoring algorithms (
17), we converted values to area t scores with a mean of 50 and a standard deviation of 10. Internal consistency reliability for the BSI in this study was good, with Cronbach's
α=.90 for the anxiety subscale and
α=.82 for the depression subscale.
The second outcome was self-perceived recovery from mental illness as measured by the Recovery Assessment Scale (RAS), which consists of 41 items rated on a 5-point scale from 1, “strongly disagree,” to 5, “strongly agree” (
18). The scale conceptualizes recovery as a status with components of empowerment, quality of life, hope, meaning of life, and tolerable symptom levels. In addition to a total score, subscales measure personal confidence, willingness to ask for help, goal orientation, reliance on others, and not feeling dominated by symptoms (
19). In prior studies, the RAS was positively related to other measures of recovery, self-esteem, empowerment, and quality of life and negatively related to psychiatric symptoms (
20). Internal consistency reliability for the RAS was good, with Cronbach's
α=.91 for the total scale and ranging from .69 to .85 for the subscales.
Intervention
The intervention was delivered simultaneously across study sites, with five waves of classes taught over a three-year period. WRAP was delivered in eight weekly sessions lasting 2.5 hours each and cofacilitated by two peers who were mental health consumers, with a third serving as backup for emergencies. Classes ranged in size from five to 12 participants and were taught in accessible community settings, free of charge. Content included lectures, individual and group exercises, discussions, and personal examples from the lives of participants and educators. Session 1 conveyed key concepts of WRAP and intervention ground rules. Sessions 2 and 3 identified personalized wellness strategies to combat negative feelings, including social connections to overcome isolation, relaxation activities, positive distraction techniques (such as listening to music, reading, and watching movies), and counseling. Session 4 introduced development of a daily maintenance plan to enhance mental health, including using medications as prescribed, getting adequate sleep, exercising to boost serotonin and endorphin levels, and eating a healthy diet to stabilize mood swings. Session 5 covered the early warning signs of recurrence of depression, anxiety, or other symptoms along with targeted coping strategies such as contacting a care provider, cognitive restructuring (such as changing negative thoughts to positive ones), or managing upsetting feelings via journaling.
Throughout the first five sessions, key recovery concepts were imparted with the use of didactic instruction, discussion, and exercises to foster hope for a meaningful future, belief in one's personal self-worth, and recognition of the value of peer support. One such activity involved writing a description of what one is like when feeling well, another called for making a list of personal strengths, and still another involved practicing peer support with a partner during class. Sessions 6 and 7 involved creation of a detailed crisis plan, and session 8 covered development of a postcrisis support plan and WRAP retooling after crises to prevent future relapse.
WRAP facilitators at all sites had a Mental Health Recovery Educator certificate from the Copeland Center for Wellness and Recovery. They also attended a 2.5-day training workshop organized by UIC researchers at which they reviewed and practiced the eight-session curriculum, learned fidelity assessment and attendance-tracking procedures, and discussed research procedures and related logistical issues. All educators were observed on multiple occasions by the local study coordinators for quality control purposes and provision of detailed feedback. Fidelity was assessed weekly with a detailed checklist of curricular components by session to track adherence to prescribed topics, time frames, and instructional modalities. Each curriculum component (for example, lecture with prescribed content, numbered handouts, and guided group discussion) was scored 1 if the prescribed element occurred and 0 otherwise. Fidelity scores were computed as the proportion of prescribed elements present for that session. Across all sessions taught in all waves, total course fidelity ranged from 90% in wave 1 to 92% in wave 5 (mean±SD=91.00±.01). There were no significant differences in course fidelity by wave or by study site. Overall, results indicated excellent intervention fidelity.
Instructors maintained attendance logs for each participant, with attendance at each class coded as 1 if present (either in person or by makeup session) and 0 otherwise. Total attendance was computed by summing attendance scores for each participant. On average, participants attended five of eight classes (5.05±3.10), and there were no significant differences in attendance by wave. Significant differences in attendance by site were observed (F=3.30, df=5 and 270, p=.01), with average attendance ranging from a low of 4.4 classes at one site to a high of 6.4 classes at another. Thus site was used as a control variable in all multivariable analyses.
Control condition
Participants in the control group received services as usual and were assigned to a course waiting list that guaranteed them an opportunity to receive WRAP after their final interview. Comparison of seven services (such as medication management and individual therapy) received by persons in the control group versus the intervention group revealed no significant differences (
Table 1). Throughout the study period, no other WRAP classes were offered at any of the sites, so the intervention was not available locally to participants in the control group.
Statistical analysis
Data were downloaded into a commercially available database system (SPSS) (
21) to test the success of randomization and to examine intercorrelations among model variables. Next, multivariate, longitudinal random-effects linear regression analysis was conducted to test for differences between intervention and control group participants' outcomes over time. A two-level random-intercepts model was fitted to the data, with the analysis controlling for study site as a fixed effect (WRAP=1 and control condition=0; time was coded as 1=baseline, 2=two-month follow-up, and 3=eight-month follow-up). We chose our modeling approach to address problems of serial correlation among repeated observations within individual participants; missing observations, given that not all participants completed all assessments; and inclusion of both time-varying and fixed covariates (
22). Analyses were conducted with SUPERMIX 1.0 software. Given that randomization was successful (described below), models controlled only for study site using indicator variables, with the Lorain site serving as contrast.
Results
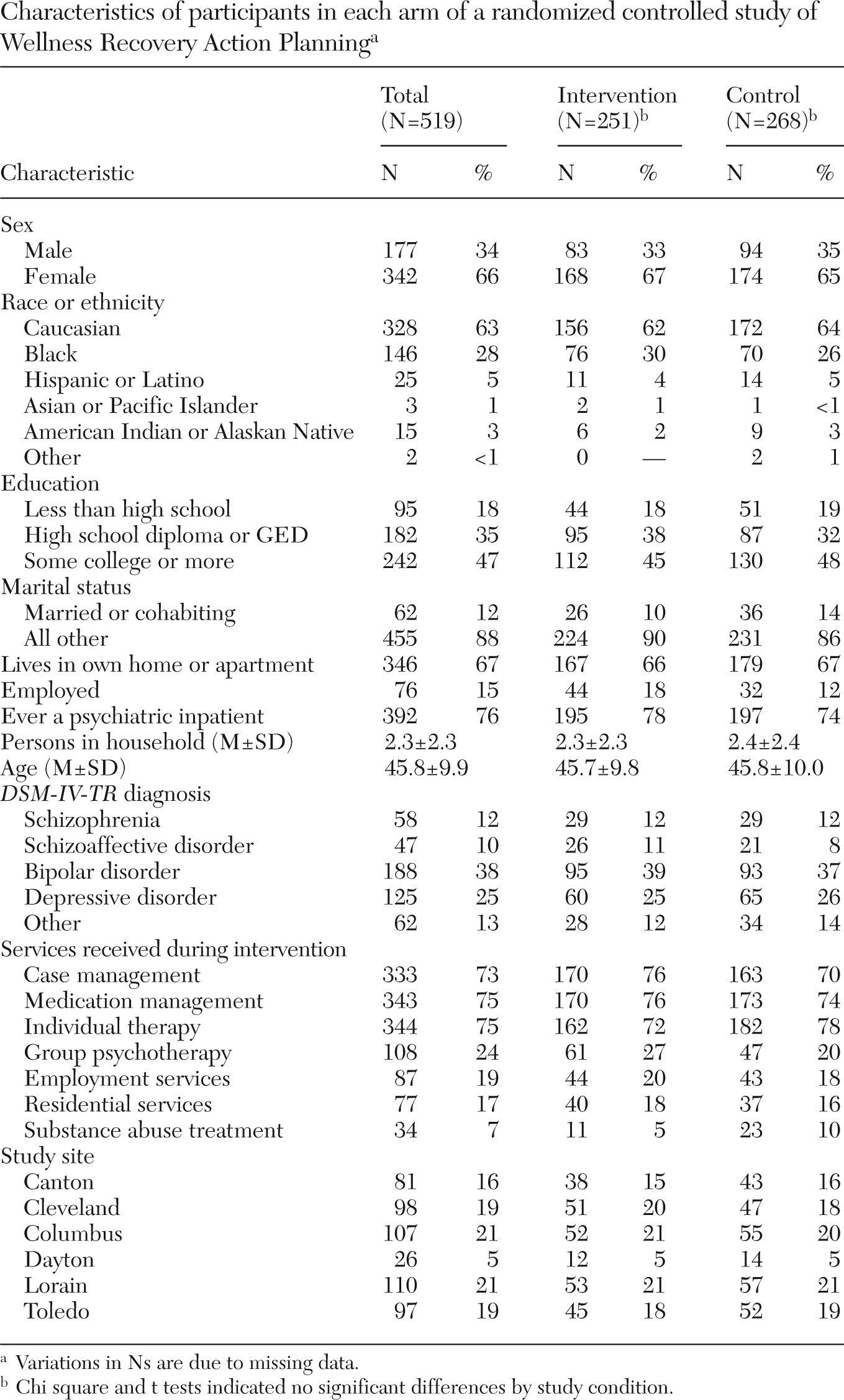
Table 1 presents baseline demographic characteristics, clinical status, employment status, and service utilization of study participants. All difference tests by study condition were nonsignificant, confirming the success of randomization.
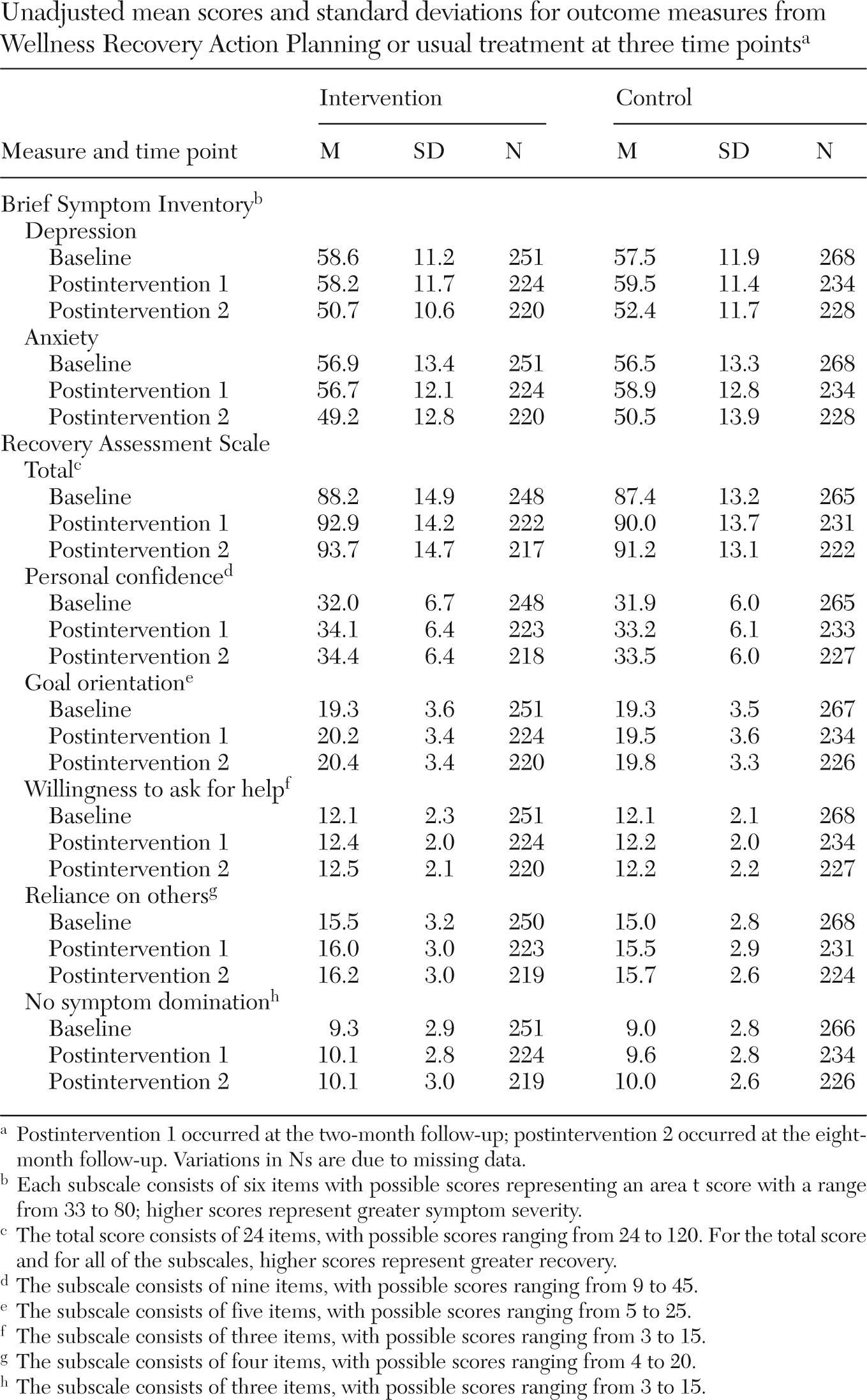
Table 2 shows unadjusted mean values over time for all outcomes by study condition.
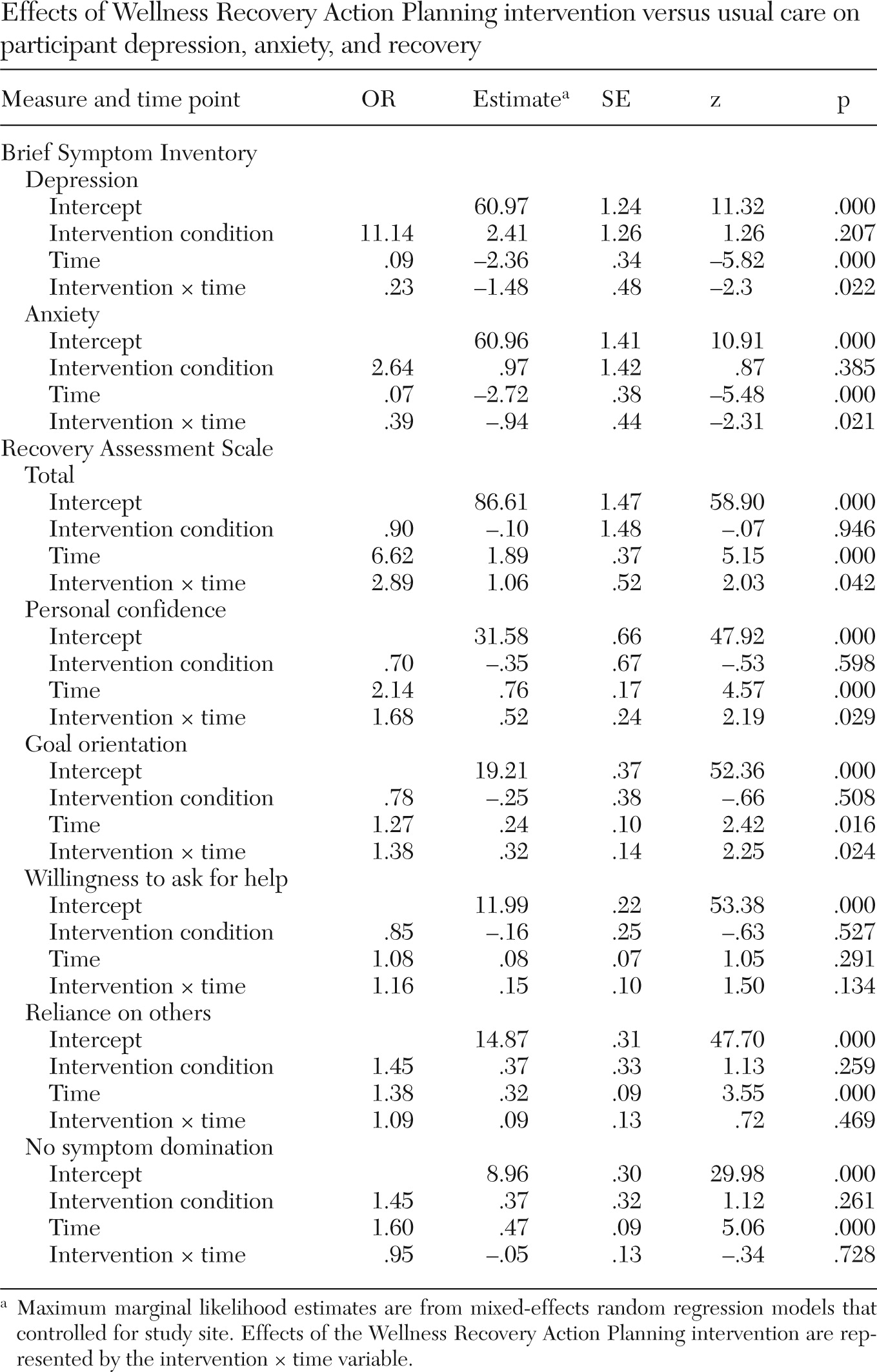
Table 3 presents the results of multivariable random regression analysis. Effects of the WRAP intervention are represented by the intervention × time variable. The intervention variable represents outcome differences by study condition at baseline (that is, success of randomization). Compared with the control group, WRAP participants reported significantly greater reductions in BSI depression and anxiety subscale scores over time. Intervention participants also reported significantly greater improvement over time than control group participants in self-perceived recovery, as indicated by the total RAS score. WRAP participants also reported significantly greater improvement over time compared with control group participants in RAS subscales measuring personal confidence and goal orientation but not in willingness to ask for help, reliance on others, or tolerable symptoms.
To address whether degree of exposure to the WRAP intervention was related to study outcomes, we used ordinary least-squares regression analysis. Among only the participants in the intervention group (N=251), we examined associations between number of WRAP sessions attended (ranging from none to eight) and study outcomes at the final follow-up time point while controlling for study site. Results revealed that the partial B for degree of exposure was significant in all models. For the BSI depression subscale, partial B=−.65 (p=.01), indicating over a half-point decrease in depression score for each WRAP session attended. For the BSI anxiety subscale, partial B=−.64 (p=.01), indicating a similar decrease in anxiety scores for each session attended. Finally, for total RAS score, partial B=.88 (p=.01), indicating an almost 1-point increase in total recovery score for each session attended. Thus the greater the exposure to WRAP, the more participants' outcomes improved.
Discussion
We found that peer-delivered WRAP is an effective intervention for reducing symptoms of depression and anxiety, with outcomes superior to those achieved by usual treatment. This finding supports the results of earlier WRAP research, including a nonexperimental study of overall symptom severity (
8) as well as our own previously published finding regarding global symptom severity (
4). WRAP also increased participants' perceptions of their own recovery from mental illness, especially recovery attitudes related to enhanced personal confidence and feelings of goal orientation.
Ours is the first randomized controlled trial demonstrating conclusively that WRAP has a positive and sustained impact on feelings of depression and anxiety. Symptom severity continued to decrease among WRAP recipients for six months after the intervention, suggesting that newly acquired symptom management skills persist beyond the time of WRAP group participation. Results were also consistent across study site, confirming WRAP's effectiveness in diverse regions of a large Midwestern state. We also found that the greater participants' exposure to WRAP, the more they improved on depression and anxiety symptom severity and self-perceived recovery. This finding supports the ongoing availability of this model to ensure that participants obtain adequate exposure to affect their recovery.
A number of WRAP program components may have contributed to the changes we observed in participant outcomes. Becoming familiar with specific triggers for their own negative thoughts and feelings may have helped participants avoid situations and people that made them feel depressed or anxious in the past. Creation of a daily maintenance plan to enhance mental health, such as using medications as prescribed, exercising to boost serotonin and endorphins, and maintaining good nutrition to stabilize mood swings, may have helped participants avoid the onset of symptoms of depression and anxiety. Awareness of the early warning signs of sad or anxious feelings along with targeted coping strategies, such as cognitive restructuring or recording upsetting feelings in a journal, may have helped participants better manage symptoms once they emerged and thus prevent their worsening. Learning recovery concepts through didactic instruction, discussion, and exercises designed to foster hope for a meaningful future may have contributed to increased self-perceptions of recovery. Creation of detailed plans for dealing with crises and postcrisis adjustment may have helped to reduce anxiety among participants who previously felt that they lacked control over their lives. Finally, interactions with credible role models (peers in recovery) who were WRAP facilitators may have enhanced participants' belief in their own ability to self-manage their lives, increasing perceptions of recovery and lowering feelings of depression.
At the same time, study results point to somewhat divergent effects of WRAP on the dimensions of recovery studied. On the one hand, significant improvement occurred in personal confidence, suggesting that WRAP enhanced participants' sense of self-efficacy. Similarly, recovery goal orientation may have improved because WRAP may have inspired participants to believe that they could set and achieve life goals. On the other hand, no differences were observed in recovery dimensions regarding reliance on others, willingness to ask for help, or symptom tolerance. Future research is needed to understand the differences between these recovery dimensions and their relationship to other personal changes in areas such as functioning, empowerment, self-advocacy, and self-esteem.
This study had a number of limitations, the first being that study participants were not drawn from a national probability sample of individuals with serious mental illness, which limits the generalizability of our results. Second, because all participants came from a single Midwestern state, we could not assess potential U.S. regional variations in WRAP implementation and outcomes. A third caveat concerns the wait-list control condition design of the study; use of an attention-control placebo intervention would have been a more rigorous research design. A fourth caveat concerns our reliance on participant self-report uncorroborated by clinicians or research staff. A fifth caveat is that fidelity assessment was limited to WRAP facilitator self-report; the additional use of direct observation to verify the validity of self-reports would have added credibility to fidelity assessment. Finally, a longer follow-up period might have revealed different longitudinal results.
Conclusions
Our findings build on prior evidence of the positive impact of WRAP on recovery from serious mental illness (
6–
9) and go further in demonstrating the longitudinal effectiveness of this intervention when subjected to rigorous testing. Results of the analysis show that participation in WRAP reduced symptoms of depression and anxiety and enhanced perceived recovery. Previously published findings from this research show that WRAP also enhances hopefulness and quality of life (
4) and promotes self-advocacy in treatment settings (
23). Applying a self-determination framework (
24) to these findings suggests that WRAP may create a supportive environment in which participants' motivation for health behavior change is truly volitional, with peers acting as role models for recovery and offering ongoing support for lasting wellness. WRAP's focus on enhancing competence, relatedness, and autonomy—processes that have been shown to improve health outcomes for chronic illnesses and conditions such as diabetes, obesity, and nicotine dependence (
25)—has much to offer the field of recovery as it expands and develops.
Acknowledgments and disclosures
This work was funded by cooperative agreements H133B050003 and H133B100028 from the National Institute on Disability and Rehabilitation Research, U.S. Department of Education, and by the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. The authors gratefully acknowledge the cooperation and assistance of the following organizations: the Ohio Department of Mental Health; the Lorain County Board of Mental Health; the Mental Health and Recovery Services Board of Lucas County; the Alcohol, Drug and Mental Health Board of Franklin County; the Mental Health and Recovery Services Board of Stark County; the Alcohol, Drug Addiction, and Mental Health Services Board for Montgomery County; the Alcohol, Drug Addiction and Mental Health Services Board of Cuyahoga County; Ohio Advocates for Mental Health; Depression and Bipolar Support Alliance Ohio; and the UIC Survey Research Laboratory. The views expressed herein are those of the authors and do not necessarily reflect the policy or position of any federal agency. This study is registered at
clinicaltrials.gov as trial NCT01024569.
The authors report no competing interests.