An estimated 22%–46% of individuals will experience diagnosable mental disorders during their lifetimes (
2–
4). Approximately one-third (36%) of individuals with such diagnoses will receive formal treatment (
5,
6). Conversely, a majority of individuals with mental disorders will not receive formal services. Various factors may contribute to low rates of treatment, including the increasing prevalence of alternatives such as online Internet support groups. Increasingly, individuals are seeking nontraditional, online mental health services. These alternative services offer several advantages, including greater convenience, reduced transportation time, lower costs, anonymity, and reduced exposure to stigma (
7–
10).
The majority of research regarding online treatment for mental health concerns has focused on therapist-guided online individual interventions. Therapist-guided Internet interventions have demonstrated effectiveness in treating several mental disorders, including panic disorder (
11), posttraumatic stress disorder (PTSD) (
12), pathological gambling (
7–
13), addictions (
7), and depression (
14,
15). Meta-analyses of therapist-guided online therapies demonstrate results similar to those of face-to-face psychotherapies, although effect sizes for online therapies vary across disorders—for example, effect sizes of .80 have been found for PTSD and panic disorders and of .17 for behavioral issues such as weight loss (
16). The effectiveness of online interventions also varies by population, with youths and elderly individuals benefiting least of all age groups (
16).
Internet support groups differ from therapist-guided online interventions. These online communities consist of networks of individuals who post questions and host discussions related to topics such as depression, anxiety, eating disorders, suicide, and self-harm. Online discussions typically are moderated by people without professional mental health training. Regulation of Internet support groups varies, with some requiring registration and others open to any participants.
Expansions of the original health belief model have used personal and contextual information to augment health belief variables in predicting service use. According to Andersen's behavioral model of health service use (
23), predisposing characteristics (such as personal and social demographic characteristics), enabling resources (such as time and money), and perceived need are additional determinants of service utilization. Taken together, health belief and service use models offer a powerful explanatory framework that helps predict use of health services; however, they have not been used to examine decision making related to the use of Internet support groups for mental health concerns. This study examined the following predictors of Internet support group use among respondents to a national survey: health beliefs regarding formal treatment, practical barriers (such as time, transportation, and affordability), and stigma.
Methods
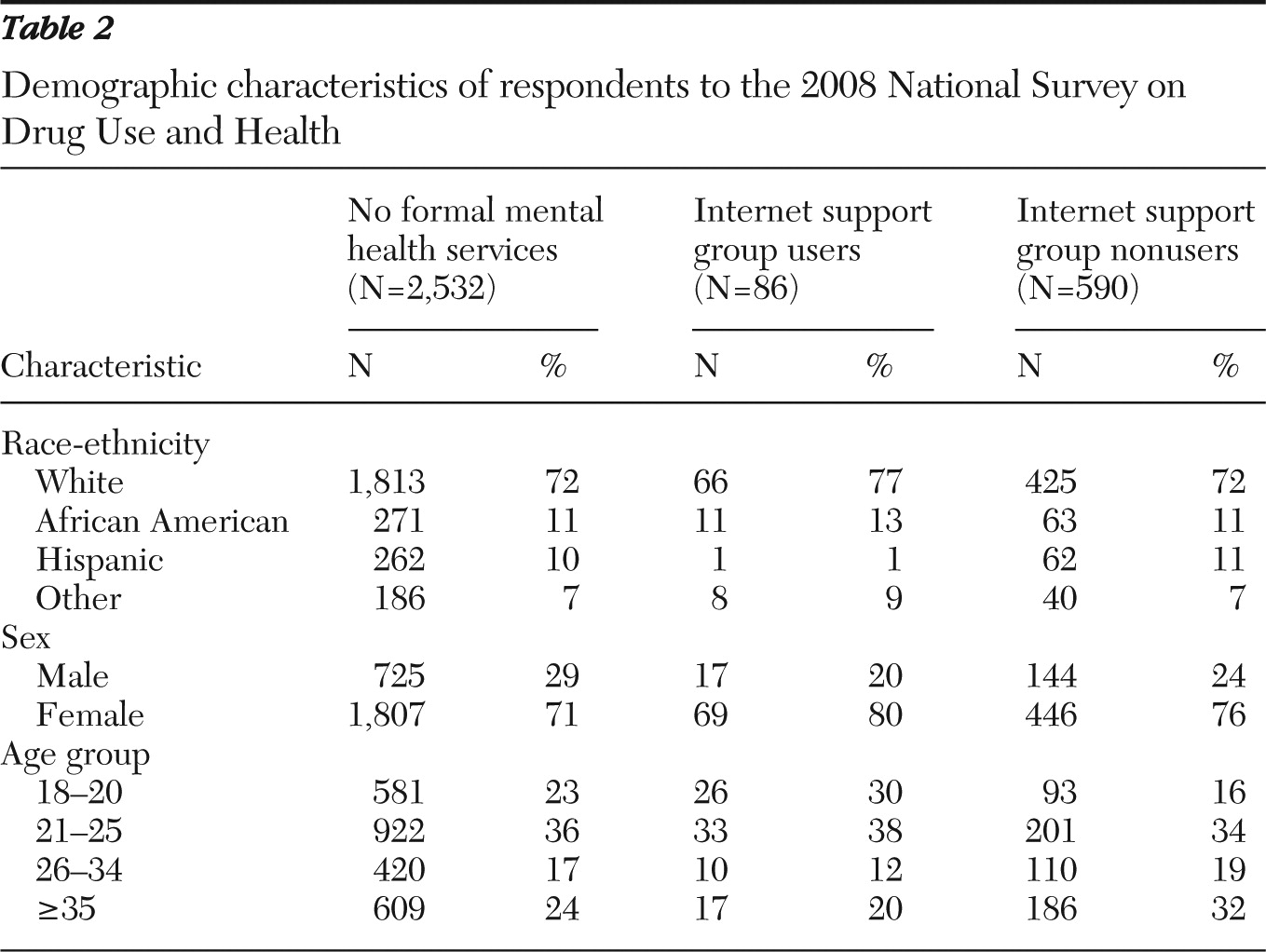
We analyzed data from a subsample of respondents to the 2008 National Survey on Drug Use and Health (NSDUH) 2008 (
24). The deidentified data were exempt from institutional review board review and have been archived at
www.icpsr.umich.edu. The NSDUH measures the prevalence and correlates of drug use in the United States with a nationally representative sample of 55,739 persons ages 12 and older. Although the primary purpose of the NSDUH is to assess alcohol and drug use, a subsection of this survey focuses on mental health disorders, impairment related to mental health symptoms, and use of formal and alternative mental health treatments. Data used in this study were drawn from a subsample of 2,532 respondents ages 18 and older who responded affirmatively to the following question: “During the past 12 months, was there any time when you needed mental health treatment or counseling for yourself but didn't get it?” Participants were provided with a list of reasons for not obtaining formal treatment and were asked to give a yes or no response to indicate whether each reason factored into their decision about treatment. [A copy of these questions is available online as a data supplement to this article.]
Respondents were asked whether they used any alternative services for mental health concerns during the previous year. [A sampling diagram is available as an online supplement to this article at
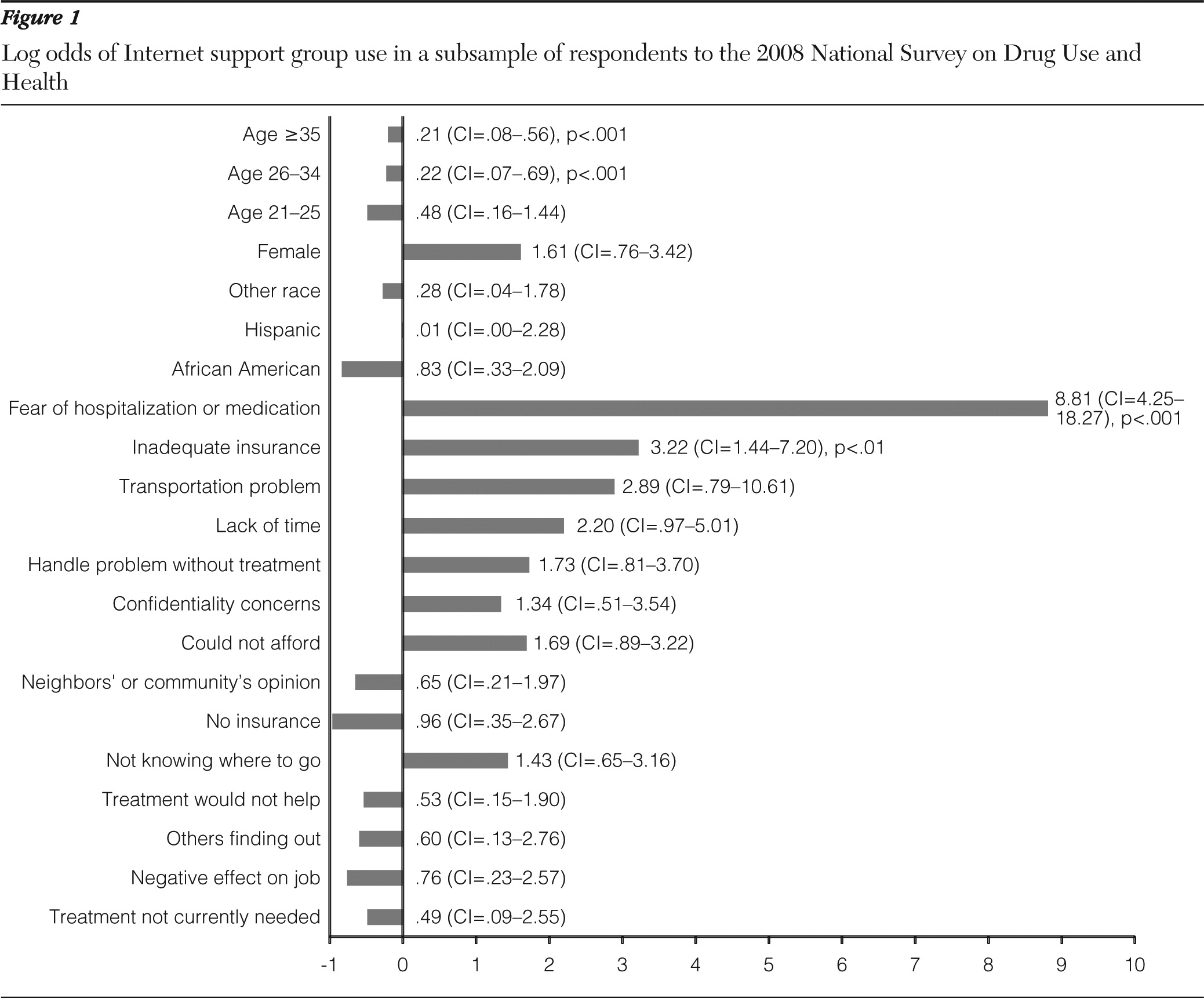
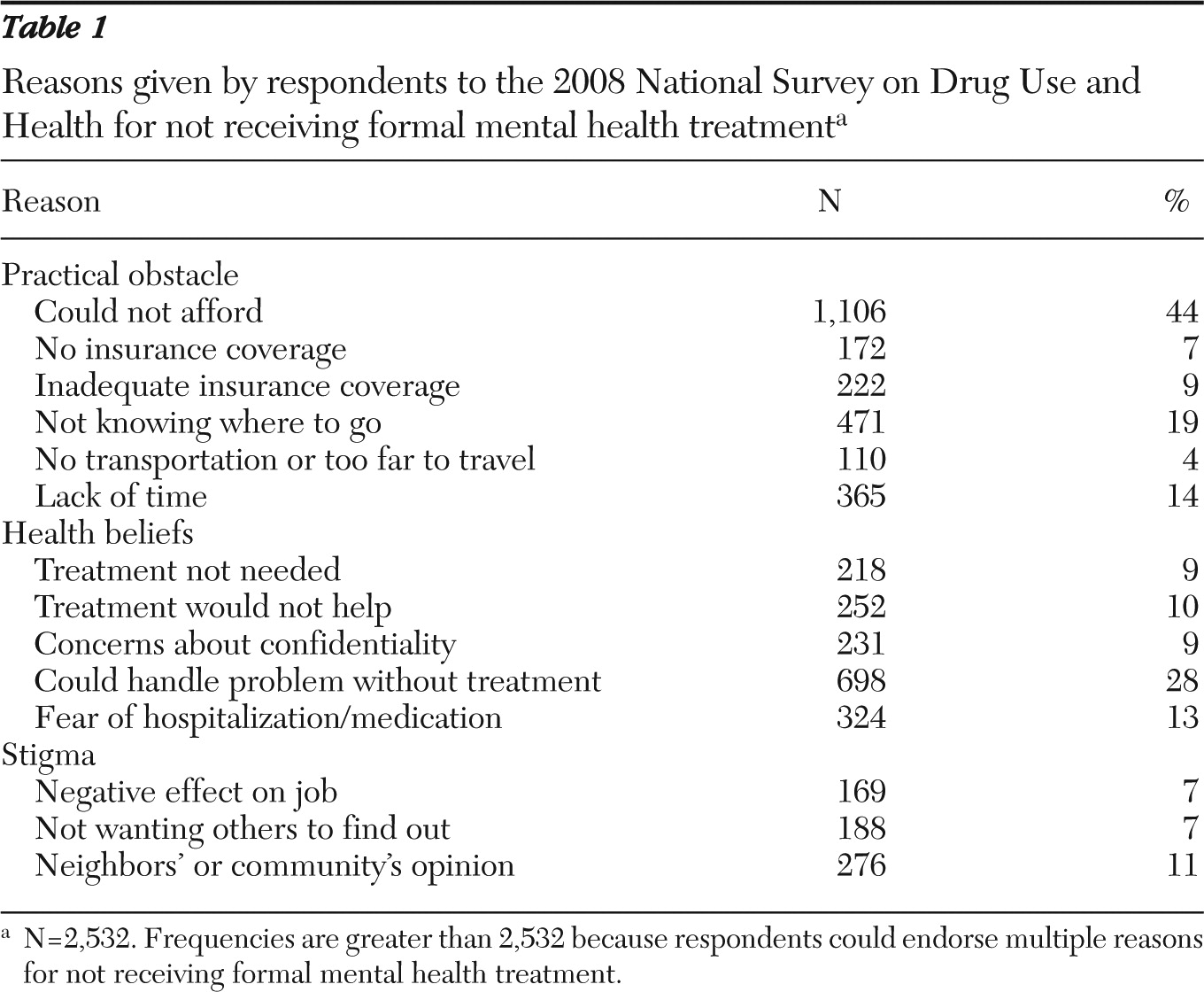
ps.psychiatryonline.org.] The dependent variable in this study was the use of Internet support groups as an alternative to formal mental health treatment. Variables from the aforementioned series of yes-no questions that assessed health beliefs (such as beliefs about treatment effectiveness and handling symptoms without treatment), practical issues (such as time and affordability), and stigma (such as not wanting others to find out and concern about negative effect on employment) were evaluated to determine whether they related significantly to use of Internet support. Univariate frequencies summarizing reasons why respondents did not use formal services are presented in
Table 1.
Logistic regression was conducted with R version 2.12.2 (
25) to examine the relationships among health beliefs, practical variables, stigma, and Internet support group use. Person-level weights provided by the Substance Abuse and Mental Health Services Administration and the U.S. Department of Health and Human Services were recalculated to reflect the final subsample of respondents used in this survey. The recalculated sample weights were designed to preserve the proportional representation of each participant in the subsample without artificially inflating statistical power. First, the sum of the weights for all respondents was used to estimate the size of the total target population: Σ
iw
i=estimated size of the target population, where the summation included all respondents in the 2008 NSDUH. Subsequently, new weights were calculated to reflect the sample size of 676 individuals who responded to the Internet support group use question:
Discussion
Our findings indicate that inadequate insurance coverage, fear of hospitalization or of taking medication, and younger age were significant predictors of Internet support group utilization in lieu of formal mental health services. These findings raise important concerns, given that the efficacy and effectiveness of Internet support groups for psychological problems has not been established.
The significant association between inadequate insurance coverage and use of Internet support groups among individuals who report not receiving formal treatment is consistent with existing literature regarding health insurance and access to medical and mental health treatments. It supports the “enabling resources” component of the behavioral model of health service use (
23), which posits that treatment disadvantages (financial burden, for example) affect decisions to use services. Research has shown that individuals who are uninsured or underinsured receive either no treatment or sporadic treatment for mental health problems (
26–
28). Furthermore, higher copayments required under various insurance plan benefit structures are negatively associated with medication adherence (
29) and mental health follow-up care (
30). Concerns about insurance and finances are among the most commonly reported barriers to accessing mental health services (
31). Thus it is not surprising that people may turn to the Internet as a cost-saving means of receiving support for psychological difficulties.
Fear of being hospitalized or being required to take medications was the strongest predictor of turning to Internet support group use instead of formal services in our study. This finding supports the behavioral evaluation component posited by the health belief model, in which perceived consequences of an illness are weighed against the costs and benefits of treatment (
20–
22). Among those who have not received formal treatment, it is possible that the fear of losing personal autonomy associated with treatment is juxtaposed unfavorably against potential benefits of treatment. This is noteworthy, given that the study sample came from a subset of individuals who reported having concerns regarding their mental health yet did not receive treatment for those concerns. It raises the possibility that individuals who choose not to receive treatment may view mental health services as potentially coercive or restrictive, a concern that is avoided in the anonymous context of the Internet.
A well-replicated finding in mental health research is that people who have been treated for serious mental illness are likely to experience various degrees of coercion (
32,
33) and exhibit concern about future coercive treatment (
34–
36). This concern is associated with a reduced likelihood of seeking medical services, even for life-threatening general medical illnesses (
37), and is the source of debate in legal, psychiatric, and psychological arenas (
38). Although the majority of research regarding fears of the consequences of mental health treatment has been conducted with mental health consumers, several studies have demonstrated that these fears are also a concern among the general public (
39–
41) and interfere with treatment seeking (
31).
Our finding that older age groups (≥26 years old) were less likely than 18- to 20-year-olds to use Internet support is consistent with existing research regarding how the Internet is used by youths and young adults experiencing psychological distress (
42,
43) and aligns with general knowledge about the Internet's role in the social lives of younger individuals. The behavioral model of health service use (
23) suggests that predisposing characteristics (such as age) have substantial bearing on treatment decisions. In this study, age was relevant to the decision to use the Internet instead of formal treatment and may reflect the ubiquitous nature of the Internet as a social medium in the lives of young people. Particularly concerning in this regard are studies suggesting that younger people receive fewer benefits from Internet-based mental health interventions than older users do (
16). Adolescents and young adults are a subgroup that is especially vulnerable to catastrophic outcomes such as suicide (
44), yet they are more likely than older people to be attracted to Internet support.
Stigma was not a significant predictor of Internet support group use in this study. This is inconsistent with previous research suggesting that those who have experienced past stigma or who fear future stigmatization may opt for anonymous support (
45,
46). Further research is needed to understand why stigma was not associated with Internet support group use in this NSDUH subsample. One explanation is that previous research has been conducted with selected samples of individuals with problems that were difficult to hide—for example, the suicide of a loved one (
45). In contrast, participants in the NSDUH came from a general population sample that was not selected for specific disorders or social problems. Regardless, social isolation has important clinical and societal consequences in that stigma may restrict intervention options for people who have serious mental health problems.
Our study highlights relationships between predisposing characteristics (age, for example), enabling resources (such as inadequate insurance coverage) and concerns about treatment (such as fear of hospitalization or taking medications) that predict use of Internet support in lieu of formal mental health treatment. Further research efforts to elucidate the efficacy and effectiveness of Internet support groups for specific populations are important given persistent questions about possible iatrogenic effects of online supports. For example, Internet support group abuses have been noted in documented cases of falsified suicide and death by purported Internet support group members who infiltrate discussion groups and misrepresent themselves (
47). These incidents, as well as the potential for negative interactions between message posters (
48) and sites that promote or normalize self-injurious behavior (
42,
49), carry significant clinical implications for individuals experiencing psychiatric symptoms.
Furthermore, the asynchronous nature of Internet support group communication presents a potential concern during mental health crises. Synchronous communication may be more paramount for users who seek support during times of crisis. Currently, little research evidence is available regarding the efficacy or effectiveness of Internet support groups for users experiencing mental health crises (
50).
However, advantages of Internet support group use have been documented. Online groups can provide individuals with emotional support and information (
51), empowerment (
52), and anonymity (
53). Internet support groups reduce transportation costs and may increase accessibility of support (
54). The Internet offers the potential for communicating in a social arena that differs from usual interpersonal contexts, offering potential protection from stigma (
52). Furthermore, Internet groups may offer opportunities for support to people whose expectations of stigma erect barriers to engagement with formal services (
46). Internet groups may also be a valuable resource for members of marginalized subgroups (
42).
This study had limitations common to secondary data analysis. Individuals provided yes-no answers to questions regarding their reasons for not seeking formal mental health services. More finely grained responses may be informative for evaluating the degree to which people are influenced by stigma, financial constraints, and practical obstacles to treatment. In addition, the NSDUH was designed to assess substance use, psychiatric symptoms, and service utilization; it was not designed specifically to examine health beliefs and their relationship to the use of Internet support groups. Detailed surveys that focus on these relationships are needed to outline more definitively the advantages and disadvantages of formal treatments versus online supports.
Item content was combined across several items for ease of survey administration. For example, the combined item “fear of hospitalization/taking medicine” may represent two unique constructs to which survey participants would respond differently if the presentation had been separate. Further research is needed to examine whether individuals view these aspects of mental health treatment differently in deciding whether to seek services.
Further research is needed to refine our measurement of the role of finances in decisions regarding formal treatment. Specifically, lack of affordability, absence of mental health insurance coverage, and inadequacy of insurance coverage may play different roles in decisions to use formal treatment versus Internet support. We were unable to examine these issues within the parameters of this survey.
Finally, the sample included only 86 individuals who endorsed using Internet support groups instead of formal treatment services. Although the sample size provided sufficient power for the analyses presented herein, it may not have captured fully the characteristics of people who use the Internet for psychological support (
42). Future studies are warranted to evaluate characteristics of this population of Internet support group users as well as to establish whether Internet support groups are efficacious and effective.