Community integration is often held as a value and goal of programs serving persons with severe mental illness. However, it is a rarely measured program outcome (
1–
5). Although definitions vary, community integration has been defined as having three components: physical integration (extent to which an individual participates in activities and uses community goods and services), social integration (extent to which an individual engages in social interactions with community members), and psychological integration (extent to which an individual feels a part of the community) (
6).
This exploratory study examined whether assignment to an intervention designed to reduce homelessness, critical time intervention (CTI), was associated with aspects of community integration among formerly homeless adults with severe mental illness after discharge from inpatient psychiatric treatment.
Methods
Data were from a randomized controlled trial of CTI, conducted from 2002 to 2006, details of which are available elsewhere (
7). Briefly, CTI is a nine-month care coordination model that aims to enhance continuity of support for persons with severe mental illness during the critical period of transition after discharge from shelters, hospitals, and other institutions (
8,
9). CTI strengthens individuals' long-term ties to services, family, and friends and provides time-limited direct emotional and practical support.
After discharge from a psychiatric hospital, 150 participants were randomly assigned to either CTI plus usual services or usual services only and were followed for 18 months. Eligible participants had a lifetime DSM-IV diagnosis of a psychotic disorder, were homeless at the index hospitalization (or homeless at some point during the previous 18 months), and spent their first night after discharge in a place other than jail or a hospital. Primary psychiatric and substance use diagnoses were assessed at baseline with the Structured Clinical Interview for DSM-IV (SCID). Housing data were collected every six weeks via participant self-report. The study was approved by the discharging hospital's institutional review board under a multisite collaborative agreement overseen by the New York State Office of Mental Health. Written informed consent was obtained from all participants.
Subscales from the Lehman Quality of Life Interview (LQOLI) that conceptually map onto two of the three aspects of community integration noted above were administered at the 18-month follow-up interview (
10). Social integration was measured by the LQOLI social relations subscale, which contains questions about contact with people who are not relatives. Participants were asked how often they did things with a close friend, visited someone, phoned someone, wrote a letter, did something that they planned ahead of time with another, and spent time with a romantic partner. The six items were dichotomized (at least once a month=1, less than once a month=0) and summed for a possible score of 0 to 6, with higher scores reflecting better social integration. The internal reliability for the scale was acceptable (Cronbach's
α=.67).
Physical integration was measured by the LQOLI daily activities and functioning subscale. This subscale has 16 items; many but not all of the items reflect physical integration. Participants were asked (yes or no) whether in the past week they went on a walk, went to a movie or play, watched TV, went shopping, went to a restaurant or coffee shop, went to a bar, read, listened to the radio, played cards, went for a ride in a bus or on the subway or in a car, prepared a meal, worked on a hobby, played a sport, went to a meeting of some organization or social group, went to a park, or went to a library. Responses were summed for a possible score of 0 to 16, with higher scores reflecting better physical integration. The scale's internal reliability was acceptable (Cronbach's α=.69).
Housing stability was measured by whether participants were continuously domiciled (private housing or housing program) between baseline and 18 months. Baseline clinical factors included lifetime substance use diagnoses assessed by the SCID and symptoms assessed by the Positive and Negative Syndrome Scale (PANSS).
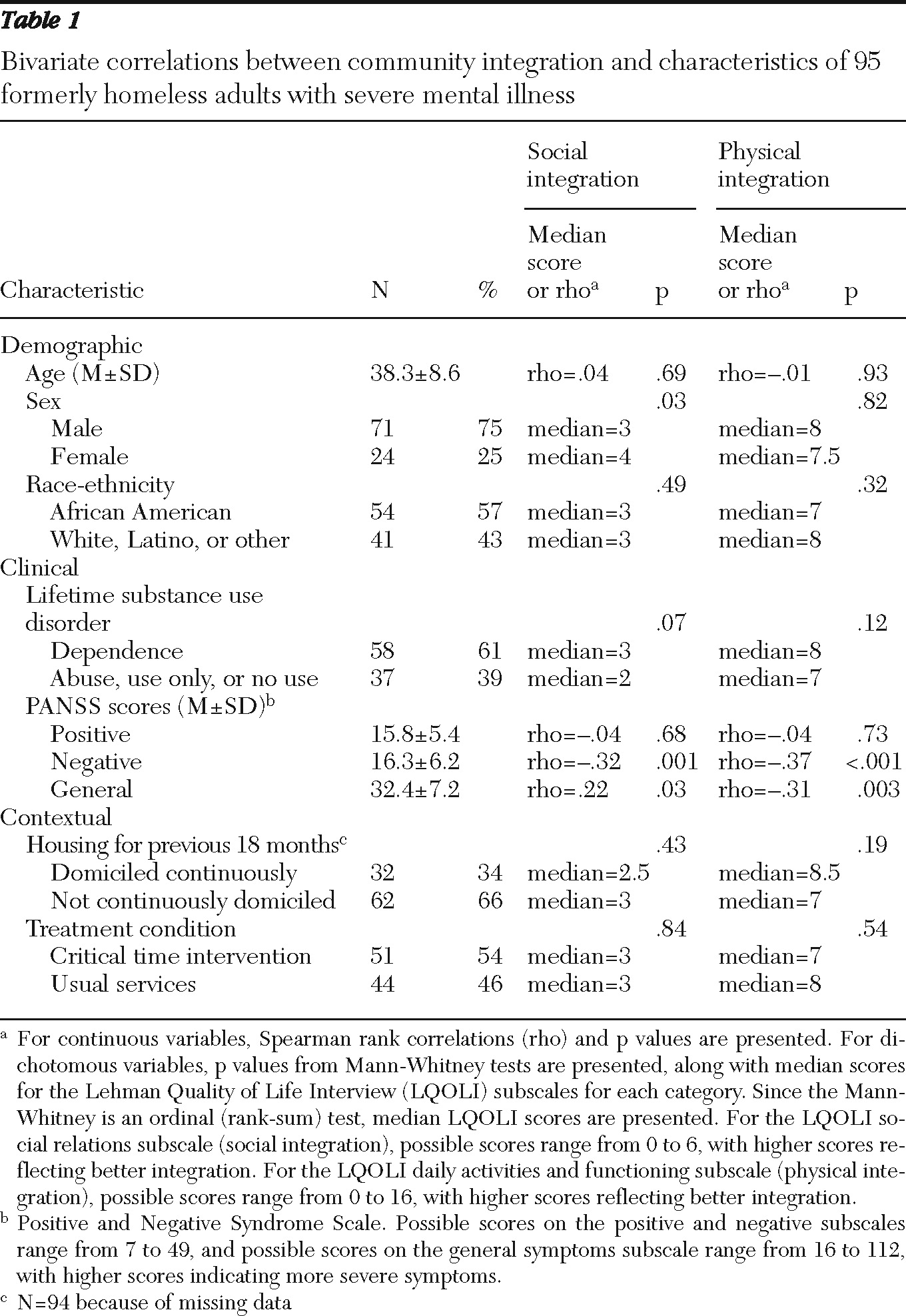
We examined bivariate associations between LQOLI subscale scores and demographic characteristics (sex, age, and race-ethnicity), clinical characteristics (symptoms and lifetime substance use disorder), housing status, and experimental condition. Because of skewed LQOLI distributions, Spearman rank correlations were used for continuous variables and Mann-Whitney U tests were used for categorical variables. Linear regression was used to model the unique association between variables and both LQOLI subscales. As an exploratory study with data from only 95 of 150 participants, the analysis did not follow usual analysis standards for randomized controlled trials.
Results
Ninety-five participants (71 men and 24 women) with a mean±SD age of 38.3±8.6 years had complete LQOLI data at the 18-month assessment. Fifty-four (57%) were African American, 18 (19%) were white, 17 (18%) were Latino, and six (6%) classified themselves as other; 75 (79%) had never married and 18 (19%) were separated or divorced. Ninety participants (95%) had a diagnosis of schizophrenia or schizoaffective disorder, and 79 (83%) met criteria for lifetime substance abuse (22%) or dependence (61%). Mean PANSS scores were 16±5 for the positive symptoms scale, 16±6 for the negative symptoms scale, and 32±7 for the general symptoms scale, with higher scores indicating more severe symptoms. Thirty-two participants (34%) were continuously housed during the 18-month follow-up period. Fifty-one participants (54%) were assigned to the CTI condition.
Complete follow-up data were obtained for a significantly greater proportion of participants with a substance dependence diagnosis than those without (N=58, 75%, of those with substance dependence and N=37, 54%, of those without substance dependence; χ2=7.5, df=1, p<.01). There were no other group differences in follow-up rates related to baseline characteristics.
The mean score for social integration was 2.6±1.8, and almost half the participants (N=43, 45%) scored 2 or less (range 0–6). For physical integration, the mean score was 7.5±2.9, and half the participants (N=47, 49%) had scores between 1 and 7 (range 1–14).
Bivariate analyses are presented in
Table 1. Assignment to CTI was not associated with either integration measure. Inverse associations were found between social and physical integration and baseline PANSS negative and general symptom scores—that is, more severe symptoms were related to poorer integration. Female sex was positively associated with social integration.
In the regression analyses adjusting for all covariates (not shown), assignment to CTI was not significantly associated with either integration measure. However, both PANSS negative and general symptom scores were associated with social integration at the trend level (β=−.06, p=.08, and β=–.07, p=.08, respectively). PANSS negative and general symptom scores retained significant associations with physical integration (β=−.15, p<.01, and β=−.13, p=.03, respectively). Female sex was significantly associated with social integration (β=−.89, p=.03). There was no relationship between housing status and the integration measures in the bivariate or multivariate analyses.
Discussion
The findings of this exploratory study suggest that CTI assignment was not associated with our measures of community integration. Although improving community integration was not a primary goal of CTI, we felt that CTI might have some impact on this outcome because the intervention aims to strengthen ties to formal and informal supports. Although CTI and other community support models, such as assertive community treatment, may improve housing stability and reduce hospitalization, these interventions may not, on their own, improve community integration (
11). Rather, it is likely that additional strategies, including those explicitly focused on promoting active participation in civil society (including employment), will be needed to enhance community integration for persons with severe mental illness. In regard to the lack of association between housing and integration, although living in the community is inherently part of community integration, this finding is in line with other literature noting that living in the community does not necessarily mean someone is part of the community and participating accordingly (
4,
6).
A study limitation is that the integration measures we used may omit important areas, such as psychological integration and interactions with people whom the respondent does not know, which may have led us to underestimate the true impact of the CTI. However, the QOL measures we employed have significant conceptual overlap with recognized definitions of community integration (
6,
12–
15), and there is little consensus in the field on the best way to measure this broad construct.
Conclusions
Community integration is rarely studied as an outcome of mental health interventions, and surprisingly little is known about its correlates among adults with severe mental illness. The lack of theoretically based, carefully validated measures of community integration may hamper efforts to assess this key domain as a program outcome. Promising recent efforts are developing the idea that integration is determined by the interaction between personal capacity (such as cognitive ability, motivation, and psychiatric symptoms) and social opportunity (such as housing and employment status, case management support, and a nonstigmatizing environment) (
12,
13). Future work may build upon this framework to guide both the development of valid measures and more effective interventions in this critically important domain.
Acknowledgments and disclosures
Funding for this work was provided by grants R01MH59716 and T32 MH013043-36 from the National Institute of Mental Health.
The authors report no competing interests.