Risk factors for violent behavior have mainly been validated in populations of males. Therefore, it is reasonable to question the relevance of applying the same risk factors to females (
1,
2). In 2009, a total of 14,348 individuals were convicted of a violent crime in Sweden, of whom 1,741 (12%) were females (
3). This relative difference is consistent even for severe violent crimes, such as homicide. However, the gender gap seems to shrink when measurements of violence other than convictions—such as self-reports—are taken into account. A population-based study using interview data found that 18% of the males in a national household sample reported being violent during the five years preceding the interview. The corresponding figure for females was 6% (
4). The base rate of violent behavior in different populations is one crucial factor to consider in decisions concerning best practice in risk assessments (
5–
8).
There are mixed and even contradictory empirical results with respect to gender differences in violent behavior within clinical samples of psychiatric patients. Some findings suggest that the gender gap concerning violent behavior is marginal or nonexistent (
5,
7,
9–
12), and others indicate a gender gap similar to that found in the general population (
13–
15). There is more agreement with respect to the lack of evidence for the validity of risk assessment methods when used with female psychiatric patients. Clinicians more often make valid predictions of violent behavior by male psychiatric patients than by female psychiatric patients (
6,
7,
16,
17). One study found that regardless of their professional background or gender, clinicians made equally poor predictions of violent behavior by females, (
18). The underlying reasons are unknown, but some have speculated that underestimation of the base rate of violent behavior among female psychiatric patients is one factor (
5,
19). Few guidelines exist to support clinicians conducting risk assessments with female patients and offenders. Also, very few risk assessment methods have been constructed for female samples or mixed-gender samples, and even fewer methods have been validated for females.
The MacArthur Violence Risk Assessment Study (MacVRAS) has developed risk assessment software called the Classification of Violence Risk (COVR) (
20–
22). The COVR uses a decision tree–based prediction model, involving numerous risk and protective factors (
21). Risk factors are assessed according to the patient’s answers to prior questions. The software analyzes an individual’s responses and assigns the respondent to one of five risk groups, with an estimated likelihood of future violence ranging from 1% to 76%. The COVR software is a commercial product that currently costs $320. The cost for each produced report after installation of the software is approximately $10. One of the major advantages of COVR is that the instrument is empirically constructed, with a base of nearly 1,000 patients, of whom over 40% were females.
Cross-validation of COVR has produced mixed results. In an earlier validation study, Monahan and colleagues (
22) concluded that the COVR may be helpful for clinicians when making decisions about acute psychiatric patients. Snowden and colleagues (
23) concluded that the instrument also can be used to predict institutional violence within the forensic mental health system in the United Kingdom (UK). However, another UK study concluded that the instrument did not significantly predict violent acts 20 weeks postdischarge among nonforensically involved psychiatric patients (
2). In an earlier report, our results suggested that COVR could predict violent behavior in Sweden significantly better than chance (area under the curve [AUC] for the receiver operator characteristic [ROC]=.77). However, because there were few individuals in the very-high-risk group, the 95% confidence intervals (CIs) were wide (
24). It is possible that COVR is valid for one gender but not for the other. Therefore, gender-specific validation is important and was the goal of this study.
Methods
Design
We conducted a prospective clinical follow-up study in which the patients were interviewed after discharge or after leaving a psychiatric emergency unit. They were followed up with telephone interviews ten and 20 weeks later. Persons providing support to these patients also were interviewed, and data from both sets of interviews were combined with follow-up data from the National Register for Criminal Convictions.
Setting and sample
Sampling was conducted at the two largest public psychiatric hospitals in Stockholm County. Both hospitals provided voluntary as well as involuntary care. Patients were recruited from psychiatric wards and the emergency unit that serves all of Stockholm County. At the emergency unit, prior psychiatric contact or referral by a third party is not required.
Inclusion criteria for the study were age between 18 and 60 years, returning home after an acute consultation or admission at either of the two hospitals, having a Swedish social security number (needed for access to records and national registers), having a clinical
ICD-10 diagnosis (
25), and being able to participate in an interview in Swedish or English.
A total of 497 patients were approached, and 390 (78%) gave informed consent to participate in the research. There were no significant differences between participants and nonparticipants except that patients with a diagnosed personality disorder were significantly more likely to participate than patients with other diagnoses. A more thorough description of the patients can be found in our previous reports (
24,
26). A comparison of the patients with and without any follow-up interview showed that those who were followed up had significantly shorter hospitalizations. Participants born outside Sweden and participants with psychosis were significantly less likely than others to be followed up. Eighty-six percent of the participants (N=283) were classified by COVR as having low or very low risk of violence, 11% (N=37) were classified as having average risk, and the remaining 3% (N=11) were in one of the two high-risk groups.
Patients were interviewed in 2007 by two research assistants. When hospital staff announced that a patient was due to return home, we verified eligibility for inclusion and asked the patient to participate. The duration of the interview was 15–20 minutes. The study was approved by the Stockholm Regional Ethical Committee.
Measures
Baseline data.
Data on gender, age, civil commitment status, diagnosis, admission, and duration of hospitalization were collected from medical case records and via communication with the responsible clinician. The patient interview comprised questions concerning country of birth and patient’s income, which were followed by the COVR assessment. The COVR instruction manual states that clinical judgment may be used to raise or lower the risk estimate generated by the software, but in this study the COVR-generated risk estimate was not clinically adjusted. If there were any inconsistencies between the information in the records and the information provided by the patient, the patient was asked to clarify his or her response. We relied on the patient’s clarification as the final information. We chose to use the clinical diagnosis in the records rather than conduct a specific diagnostic research interview for two reasons: an extension of the research interview might have jeopardized the response rate and data quality, and the exact diagnosis was not a main concern of the study.
Heavy drinking was assessed by the CAGE Questionnaire (
27), and the cutoff to indicate heavy drinking was set to three or more positive answers. Victimization in childhood, level of anger (Novaco Anger Scale [
28]), and violent thoughts (Schedule of Imagined Violence [SIV]) were extracted from the COVR assessment. On the SIV an individual was assessed as positive if he or she answered affirmatively to having had in the past two months at least one thought to harm others (
29). Violent behavior preceding inclusion in the study was assessed with the MacVRAS instrument (
21), and victimization preceding inclusion in the study was measured by using questions from the Annual Survey of Living Conditions conducted by Statistics Sweden (
www.scb.se/Pages/Product____12187.aspx) (
26). The participants were assured that information from the research interview would not be reported to the responsible clinician unless it concerned a threat toward a named person or a case of child mistreatment.
Follow-up data.
The patients were interviewed by telephone ten and 20 weeks after inclusion. Twenty-five percent of the sample consented to our conducting an additional telephone interview with someone providing support to the patient, including a family member, friend, or staff member. These interviews were conducted by professional interviewers from Statistics Sweden, specifically trained for this project and chosen for their record of having clinical experience in psychiatry, the criminal justice system, or both. The interviewers were blind to the information from the baseline assessment. Data on violent behavior were collected through the questionnaire from the MacVRAS (
21). The National Register for Criminal Convictions, administered by the Swedish National Council for Crime Prevention, was consulted to identify criminal violence among the participants. The outcome measure, violent behavior, was defined as in MacVRAS—that is, any battery with physical injury, use of a weapon, threats made with a weapon in hand, and any sexual assault (
21,
24).
Statistical analysis
We compared participants with those who had no follow-up by using chi square for categorical data and the t test for continuous data. All tests were two-tailed, and p<.05 was regarded as statistically significant.
To analyze the predictive validity of the COVR and specific risk factors, analyses of the ROC were conducted. The ROC is frequently used to assess predictive validity of different prediction methods and has the major advantage that it is less dependent on base rate (
30). The ROC produces an effect size called the AUC, which is reported together with the 95% CI. The range of the AUC is 0 to 1, where 0 equals a perfect negative relationship, .5 equals chance, and 1 equals perfect prediction. The correlation between COVR scores and violent behavior is also reported with the use of Spearman’s correlation. The proportions of patients with violence for specific risk factors during the follow-up are presented, along with the odds ratios from logistic regression. The statistical analysis was computed in SPSS, version 18 for Windows.
Results
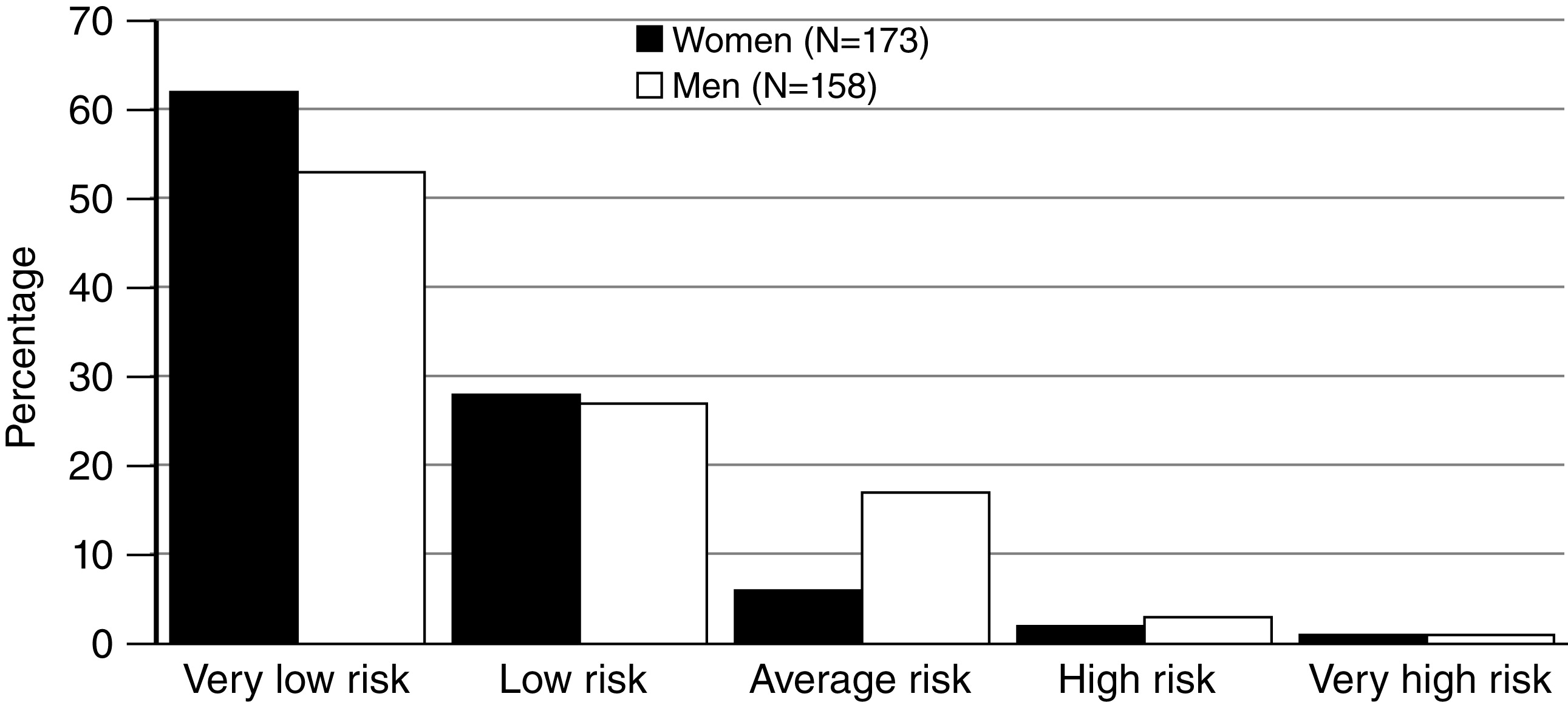
Descriptive details for the 331 participants are presented in
Table 1. The women were somewhat younger than the men. Personality disorder was significantly more prevalent among women (p≤.001), and psychosis was significantly more prevalent among men (p≤.05). Risk categories are displayed by gender in
Figure 1.
Prevalence of violent behavior
The self-reported base rate of violent behavior was 5% (N=16). Information provided by persons supporting the patient resulted in the addition of one patient with violent behavior, maintaining the 5% base rate. The criminal register added another two patients, for 19 patients total and a final base rate of 6%. The prevalence of violent behavior was similar between genders. Eleven of the 173 women (6%) and eight of the 158 men (5%) had been violent 20 weeks after discharge. To allow for confounding effects of age, we split the sample into a younger (18–29 years) and an older (30–60 years) group. Among people ages 30 to 60, the differences between base rate and follow-up were nonsignificant among women (8% in the younger group and 5% in the older group), but base rates were significantly lower among the oldest men (13% and 2%; p<.01).
Risk factors for violent behavior
As shown in
Table 2, four specific risk factors significantly predicted violent behavior among female psychiatric patients: victimization in childhood, positive results on SIV, higher level of anger, and showing violent behavior in the previous year. Young age was the only significant risk factor for future violence within the male group (
Table 2).
Predictive validity of COVR
As reported earlier, the numbers of patients in the high-risk groups were small (
24). This was true for both female (N=5) and male patients (N=6). An interesting finding is that the proportion of violent patients in the average-risk group of men was 8%, whereas it was 46% for the corresponding group of women (
Table 3). [A figure illustrating these proportions by risk group is available online as a
data supplement to this article.] In addition, the proportion of violent female patients in the average-risk group (46%) was higher than that in the high-risk group (33%). The correlations between COVR score and violent behavior were .28 (p<.001) for female patients (AUC=.78, CI=.60–.96, p<.01) and .22 (p<.01) for male patients (AUC=.76, CI=.59–.93, p<.05).
Discussion
Base rate and risk factors for violent behavior
One main finding of the study is that the base rates of violent behavior were similar among men and women. This finding might seem surprising. However, similar results have been shown in earlier studies (
5). Results from a UK study even indicated that female gender was a significant positive predictor of postdischarge violent behavior (
2). An unexpected finding of our study is that young age was the only significant risk factor for men. It is widely assumed that the risk factors targeted in this study (including earlier violent behavior, violent thoughts, and level of anger) are predictive of violence among males but not yet validated among females (
1,
2).
The gender-specific age analysis showed differences between men and women. Among men, violent behavior was more common from younger participants. For women, however, violent behavior was equally prevalent among younger and older participants. This difference implies that for males, the risk of violence decreases with age. Female patients on the other hand were more prone to continue acting violently, even in older age groups. This finding is in line with another Swedish study of nonforensic psychiatric patients (
31). That study showed that the fraction of violent behavior attributable to the population was relatively stable for men, 2% in the youngest age group and 7% in the oldest. However the risk attributable to women was 3% in the youngest age group and 19% in the oldest age group. Further research should study this finding in other societal settings. It has been reported that violent behavior toward others and victimization share substantial risk factors (
32), and victimization has even been proposed to be a link between mental illness and offending (
33). Base rates of violent behavior in Sweden were considerably lower than base rates reported in the United States; however, the difference in overall violent behavior is known from before (
5,
24). Also, lethal violence is five times more prevalent in the United States than in Sweden (
34).
Predictive validity of COVR between the genders
The distribution of risk categories was similar for men and women. In contrast to our hypothesis, COVR predicted violent behavior with the same validity for women as for men and also predicted violent behavior better than chance for both genders. Indeed, predictive validity was somewhat better for women than men. This finding is contradictory to an earlier research finding that violent behavior differs between males and females. Therefore, the findings underscore the benefits of using a gender-mixed sample when constructing violence risk assessment methods. The effect sizes of COVR were similar compared with those in a UK study (
23). That study examined the predictive validity of COVR to predict physical violence by forensic inpatients. The fact that correlations and effect sizes were comparable between the UK study by Snowden and colleagues and our study emphasizes the predictive validity of COVR even in different types of samples.
A study from the United States with 268 civilly committed nonforensic psychiatric patients, which examined the predictive validity of three risk assessment methods—the Psychopathy Checklist–Revised (
35), Historical, Clinical, Risk Management–20 (
36), and Violence Screening Checklist (
37)—showed results similar to ours (
38). Whether investigating violence in institutions or violence after discharge, no significant differences between the genders could be detected. The conclusion of the study by Nicholls and colleagues (
38), as here, is that the prediction methods are valid for female civil psychiatric patients.
Clinical implications
The results of this study have several implications for risk assessments among nonforensic psychiatric patients. First, the study clearly demonstrated that risk management should be a concern within the psychiatric population in Sweden regardless of gender, because the base rates of violent behavior were similar for men and women. Our finding that the base rate of violent behavior was similar between genders for psychiatric patients is also a common result in inpatient settings (
39,
40) and during follow-up in the community (
5,
11). Second, Yang and colleagues (
41) concluded that no instrument is superior to another concerning predictive validity and that clinicians should use one or more instruments that are constructed for and validated with the specific population to be assessed, rather than use an instrument that is considered superior in a more general sense.
Methodological issues
This study had several strengths, including a prospective design as well as the comparatively low attrition rate and sufficient information about refusals and dropouts. The internal validity of the findings was improved by the fact that the baseline interviews were conducted in conditions resembling the typical clinical situation. Moreover, the follow-up interviews were conducted by clinically experienced interviewers who were blind to the results of the baseline assessment. Furthermore, the baseline assessments of risk were conducted after the patients left the ward; therefore, they did not receive any treatment after the assessment that may have influenced the dynamic risk factors. The measurement of violent behavior was triangulated, with information from self-reports, persons supportive to the patient, and official registers. Thus observational bias is of low concern for the results in the study. The ROC analysis has some disadvantages (
24) but is currently seen as state of the art for assessing predictive validity (
30); furthermore, in this study, it was complemented by other statistical measures of predictive validity, such as sensitivity and specificity.
Conclusions
Violent behavior was uncommon for patients regardless of gender. In general psychiatry in Sweden, COVR has acceptable predictive validity for both female and male patients and therefore may be useful in informing clinical judgment when performing violence risk assessments.
Acknowledgments and disclosures
The study was funded by grants from the National Board of Health and Welfare, Sweden, and Centre for Gender Medicine at Karolinska Institutet, Sweden.
The authors declared a 40% research discount from Psychological Assessment Resources, Inc., when purchasing the COVR software. Dr. Monahan is a developer of COVR and has a financial interest in the software.