Engagement of individuals with serious mental illnesses in outpatient treatment is an ongoing challenge. According to the 2017 National Survey on Drug Use and Health (
1), fewer than half of adults with serious mental illnesses received any outpatient mental health treatment in the past year. Difficulties engaging in treatment may lead to elevated risks of relapse, rehospitalization, and poorer outcomes in clinical and psychosocial domains (
2).
Prior studies and reviews have identified several sociodemographic characteristics of individuals who are at higher risk for failing to engage in mental health treatment, such as male gender, unemployment, and lower educational attainment (
3–
7). Older adults with serious mental illnesses are less likely to receive follow-up care (
8). Although these individual-level and socioeconomic factors may partially explain a patient’s level of engagement, they do not fully explain the barriers to outpatient follow-up and do not account for contextual factors beyond the control of the individual (
9). The concept of structural competence highlights the importance of clinicians directly addressing the role of social determinants of health, including neighborhood conditions, in efforts to reduce symptoms, improve outcomes, and facilitate clinician-patient interactions (
10). Neighborhood characteristics, such as distance to the nearest mental health facility, mental health stigma (discrimination), and social cohesion, could play a role in outpatient follow-up and could explain utilization better than individual factors do, for example, if patients lack access to (or face barriers in accessing) services.
New epidemiological approaches have reignited interest in the ecological relationship between mental health and neighborhood-level socioeconomic conditions, which was first studied by Faris and Dunham (
11) in 1939. They argued that those who resided in a community that lacked social integration found it difficult to develop and maintain positive affiliations with family members, neighbors, and local institutions. While some sociological models have postulated that poor social integration into communities may play a causal role in mental disorders, this framework has been criticized due to its failure to consider that poverty might have pushed people into such disadvantaged communities (
12–
14). There is also mixed evidence that “diverse disorganized” neighborhoods are more accepting of people with serious mental illnesses and that these neighborhoods are associated with better mental health outcomes. Although earlier studies found that people with serious mental illnesses had better social integration scores in moderately disorganized neighborhoods (
15–
19), more recent studies suggest that living in higher-quality housing and neighborhoods is associated with reduced mental health care costs and leads to better mental health outcomes (
20,
21). However, literature regarding the association between neighborhoods and service utilization among people with serious mental illnesses has remained sparse. The purpose of this study was to examine individual- and neighborhood-level factors associated with outpatient mental health visits among persons with serious mental illnesses.
Methods
Data were derived from two randomized trials of patients with serious mental illnesses and chronic medical illness. For both studies, individuals with schizophrenia, schizoaffective disorder, bipolar disorder, major depression, obsessive-compulsive disorder (OCD), or posttraumatic stress disorder (PTSD) and one or more chronic medical conditions, including hypertension, diabetes, heart disease, and hyperlipidemia, confirmed through chart review from electronic medical records (EMRs) were eligible to participate. Individuals were recruited through clinician referral, screening in a community mental health center waiting room, self-referral through recruitment flyers, or word of mouth (
22). A total of 650 participants were enrolled across two study sites—an urban hospital in Atlanta and a suburban community mental health facility in Conyers, Georgia—between 2011 and 2017. The current study used baseline data from both projects.
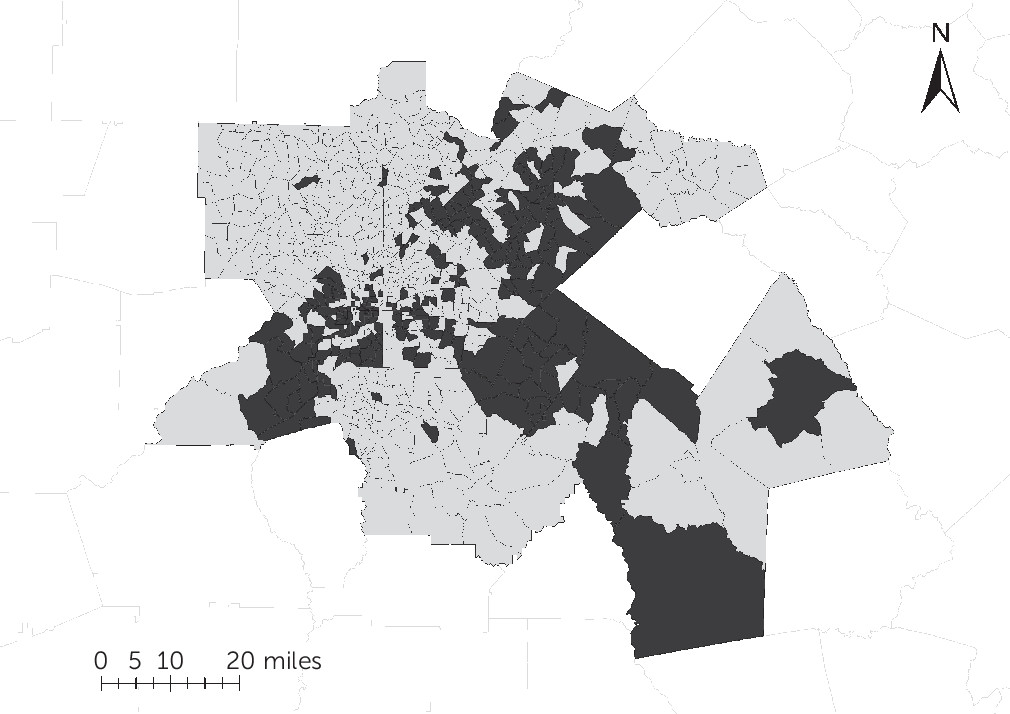
Participants excluded from this study were those who were enrolled at both sites, participants who did not provide valid responses on self-report (including invalid addresses that could not be geocoded), and participants who indicated on self-report that they were homeless or had recently moved. A total of 418 participants were included in this study. These participants were from 217 unique census tracts, which are shown in
Figure 1.
Outcome Assessment
Interviews and reviews of all medical and mental health charts were conducted at enrollment. The Service Use and Resource Form was used to measure the outcome of interest. Specifically, the following question assessed mental health provider visits: “What was the number of visits to mental health provider(s) in the past 60 days?” (
23). Because participants completed this survey on the date of enrollment, the number of visits reflects visits during the past 60 days from the date of enrollment into the study. All study participants gave written, informed consent, and the study was approved by the Emory University Institutional Review Board.
Individual-Level Variables
Individual characteristics, including age, gender, race-ethnicity, employment status, and highest level of education completed, were collected during an in-person interview and via self-report. Patients’ psychiatric and medical diagnoses were collected via self-report and verified through chart review via EMRs.
Neighborhood-Level Variables
Selected neighborhood characteristics for this analysis were guided by previous neighborhood-based research and theory (
24–
28). This research accessed neighborhood characteristics using census tract–level data designed to represent area-level properties in terms of population, economic status, and living conditions (
25). Given minimal guiding research to date, we made no a priori hypotheses regarding the relationships between specific neighborhood characteristics and outpatient mental health provider visits. Therefore, the study was considered exploratory rather than hypothesis-testing. Neighborhood characteristics were extracted from the U.S. Census Bureau’s American Community Survey 5-year estimates for 2011 to 2017 (
29). Participants’ area of residence during enrollment was geocoded to its corresponding census tract. Then, this census tract was linked to neighborhood characteristics. Because neighborhood characteristics are dynamic, the year in which participants enrolled in the study was also linked to the respective year the neighborhood characteristics were collected.
The following neighborhood characteristics were chosen on the basis of prior neighborhood-related health research (
24,
25,
28): percentage of household with income <$75,000 in 2010 inflation-adjusted dollars (low household income); percentage of residents employed in management, business, science, and arts occupations among employed civilians ≥16 years of age (white-collar occupation); percentage of owner-occupied housing (owner-occupied); percentage of residents who were high school graduates or higher (high school); percentage of female-headed households with no husband present and with children <18 years of age (single mother); percentage of families whose income in the past 12 months was below the poverty level (poverty); percentage Hispanic or Latino residents (Hispanic/Latino); percentage black or African American residents (black/African American); percentage of births in the United States (U.S. births); percentage of unemployed residents among the civilian labor force population ≥16 years of age (unemployed); percentage of residents with cash public assistance income (public assistance); percentage living in a different house in the United States or living abroad within the past year (different household); and percentage value of houses <$500,000 among owner-occupied units (low household value).
Distance to the Nearest Mental Health Facility (MinDistance)
“MinDistance” was considered a neighborhood-level factor because distance depended only on the individuals’ addresses and not on the clinic where the individual received care at the time of enrollment (
30). That is, MinDistance was calculated as the shortest distance from the patient’s address to any of the 164 mental health treatment facilities in Georgia derived from the National Directory of Mental Health Treatment Facilities—2015, including treatment facilities that responded to the 2014 National Mental Health Services Survey (
31). Google Maps Distance Matrix application programming interface was used to calculate the distance between each mental health facility and the patient’s address.
Statistical Analysis
First, we calculated the correlation between the 13 census tract–derived neighborhood characteristics. Second, after reverse-scoring the variables with negative weights (denoted “reverse”), we conducted a factor analysis to identify the neighborhood-level variables that were highly correlated with each other. For variables with loadings ≥0.40 on more than one factor, we assigned the variable to the factor onto which it loaded the strongest to ensure nonoverlapping factors and to minimize intercorrelations.
Poisson regression was chosen because the dependent variable was a count (with many low counts) rather than a continuous variable. The analysis first showed bivariate risk ratios between both individual-level and neighborhood-level characteristics and visits to outpatient mental health providers. Then, model 1 showed mutually adjusted risk ratios between the four known risk factors and fewer outpatient mental health visits. Next, model 2 showed the mutually adjusted risk ratios between the four neighborhood variables (including three census tract–derived factors and MinDistance) and visits to outpatient mental health providers. Finally, model 3 showed the risk ratios between all eight variables, including four individual-level factors and four neighborhood-level factors, and outpatient mental health visits. To avoid overfitting, only four known individual-level risk factors were chosen for models 1 and 3. All analyses were conducted by using the IBM SPSS, version 18.0.0 statistical software package.
Results
Among the participants, 76% were between the ages of 41 and 60 years, 33% were male, 62% were black/African American, 96% were non-Hispanic/non-Latino, 91% were unemployed, and 53% had 9 to 12 years as their highest level of education completed. Participants had one or more of the following psychiatric diagnoses: schizophrenia (74, 18%), schizoaffective disorder (61, 15%), PTSD (93, 22%), major depressive disorder (303, 72%), bipolar disorder (132, 32%), and OCD (24, 6%). Sociodemographic and clinical characteristics of the sample are summarized in
Table 1.
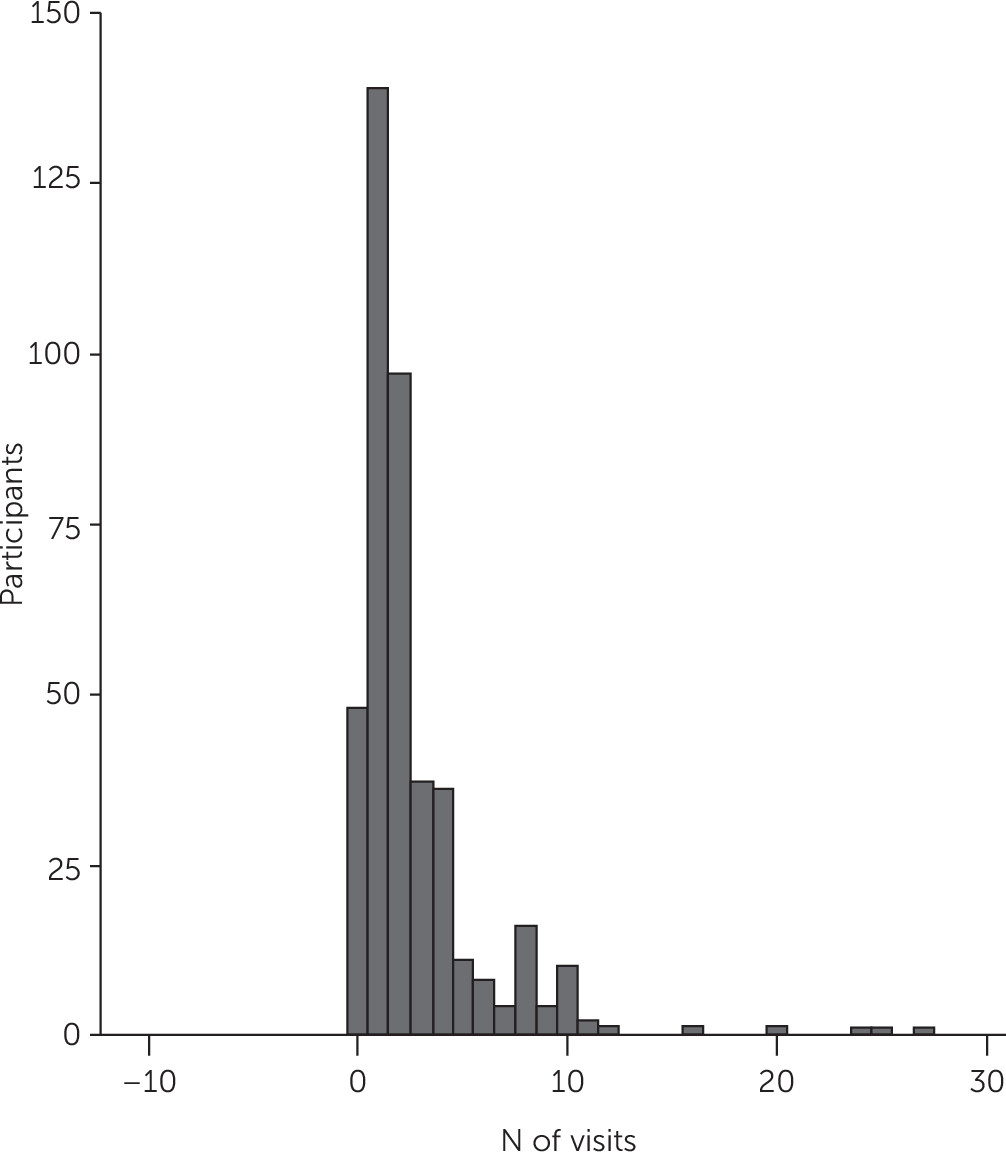
Of the 418 participants, the median number of visits to mental health providers was two. Forty-eight participants had no visits (12%), 139 had one visit (33%), 97 had two visits (23%), and 134 had three or more visits (32%). A histogram of the number of visits is displayed in
Figure 2.
The three factors produced by the factor analysis of census tract variables were as follows. Factor 1, socioeconomic deprivation, included white-collar occupation (reverse), low household income, poverty, single mother, unemployed, black/African American, low household value, and public assistance. Factor 2, ethnicity/education attainment, included Hispanic/Latino (reverse), U.S. birth, and high school. Factor 3, residential mobility, included different household and owner-occupied (reverse). Factor loadings (after Varimax rotation) from the exploratory factor analysis are shown in
Table 2.
Results of individual and neighborhood regression models—including the risk ratio for the bivariate model (RR
1), risk ratio for adjusted variables (RR
2), 95% confidence intervals (CIs), p values, and value/df of each model—are shown in
Table 3. For individual-level characteristics, age (RR
1=0.81, RR
2=0.84, 95% CI=0.75–0.95, p=0.004), male gender (RR
1=0.69, RR
2=0.73, 95% CI=0.64–0.83, p<0.001), unemployment (RR
1=0.62, RR
2=0.71, 95% CI=0.60–0.84, p<0.001), and lower educational attainment (RR
1=0.76, RR
2=0.81, 95% CI=0.73–0.91, p<0.001) were associated with fewer visits in both the bivariate and adjusted models (model 1). For neighborhood-level characteristics, bivariate analysis showed that both socioeconomic deprivation (RR
1=0.84, 95% CI=0.78–0.92, p<0.001) and residential mobility (RR
1=0.86, 95% CI=0.80–0.92, p<0.001) neighborhood factors were significantly associated with fewer visits. After mutual adjustment for two other neighborhood-level factors, only neighborhood-level residential mobility (RR
2=0.87, 95% CI=0.80–0.95, p=0.001) was significantly associated with fewer visits (model 2). After adjustment for both individual and neighborhood factors, all individual-level factors and neighborhood-level residential mobility (RR
2=0.92, 95% CI=0.84–0.99, p=0.034) remained significant (model 3).
Discussion
This study found individual- and neighborhood-level characteristics associated with the number of outpatient mental health provider visits among individuals with serious mental illnesses. Consistent with prior literature, male gender, older age, unemployment, and lower educational attainment were associated with fewer visits. After we controlled for known individual-level predictors of outpatient mental health provider visits, greater census tract–level residential mobility was associated with a fewer outpatient visits.
One study previously reported the relationship between neighborhood residential stability and mental health service utilization. Ngamini Ngui et al. (
32) found that in Montreal, greater census tract–level neighborhood residential stability was associated with increased mental health service use among those with mental disorders. They defined residential stability as the combination of proportion of the population who moved outside of their census tract during the past year and the past five years. Although our measure of neighborhood residential mobility is a combination of percentage of residents living in a different house in the past year and percentage of non-owner-occupied housing, the association between neighborhood stability and outpatient visits is a similar finding, even in a different study setting and sample.
This association may occur through several mechanisms. It is possible that neighborhoods with higher numbers of homeowners have a higher number of residents who stay in the same home, which could result in stronger social integration in the community. Prior studies have shown that homeowners are more likely to participate in activities that increase neighborhood social capital, such as volunteering or participating in block group meetings, even among low- and moderate-income homeowners (
33–
35). Homeowners have been reported to be more likely than renters to intervene when observing deviant behavior (
36). If living in an area with higher homeownership is associated with increased social support, then perhaps such support may extend to people with serious mental illnesses; homeowners may be more likely to encourage people with serious mental illnesses to use health services or may work together to attract health services to their neighborhood (
32). However, evidence also suggests that people with serious mental illnesses living in sheltered facilities have better social integration in less socially cohesive communities (i.e., communities that have a higher proportion of rent dwellings suggestive of transiency) (
15). Perhaps individuals with serious mental illnesses living in shelters experience social integration differently from those who have more stable housing situations.
Certain subgroups of individuals with serious mental illnesses who are less engaged with care may also select to live in more residentially unstable neighborhoods or live farther from mental health facilities. People with serious mental illnesses who have poor insight into the need for treatment and poor outpatient follow-up may prefer to live in slightly more disorganized neighborhoods (where “deviancy,” or being different, is more accepted, less stigmatized, and less criminalized), which happen to be residentially unstable or farther from mental health facilities. Alternatively, institutional factors may force these people to live in more disorganized neighborhoods. Factors including residential segregation and discrimination may leave people with serious mental illnesses with no choice but to live in more disorganized areas. Such structural factors often are more responsible compared with individual factors for people’s choices.
Another explanation for this association is that individuals with serious mental illnesses living in residentially mobile neighborhoods may experience more social stress that limits their ability to follow up with outpatient visits. Prior studies have found that neighborhood residential mobility was associated with higher rates of schizophrenia, major depression, and psychosis (
28,
37) and with earlier age at onset of psychosis (
38). Just as urbanicity and individual-level migration have been hypothesized to be related to the experience of social fragmentation (
39), living in an area in which many people in the community are residentially mobile may also contribute to increased social stress, which may affect health at the biological level (
40). A large body of research has shown that stressful life events and lack of social support affect the onset and course of a mental disorder (
41–
44). Therefore, patients living in residentially mobile neighborhoods may experience more stress and a higher risk of relapse, predisposing them to rehospitalization or involvement with the criminal justice system and limiting their ability to attend mental health services.
There were several limitations to the generalizability of the findings. First, the study sample was recruited from two study sites in a single metropolitan area and was not a random sample. Second, it included a relatively high proportion of women and older patients. Third, people in this study had both chronic serious mental illnesses and a comorbid medical condition. Given these sample characteristics, findings should be considered preliminary, and further research is needed to explore external validity. Another limitation to this study was the lack of a multilevel model due to the small sample. Use of a single-level model may have resulted in an underestimation of the standard errors and 95% CIs associated with the risk ratios because the nonindependent structure of observations was not considered. Additionally, many of the variables used, such as outpatient visits, were derived from self-report. Moreover, this research was not able to directly test the mechanisms by which neighborhood characteristics are related to health service use. Longitudinal samples are needed to better distinguish cause versus effect between neighborhood factors and service utilization.
This study also had several strengths. To our knowledge, it is the first study to investigate individual- and neighborhood-level predictors of outpatient mental health service utilization among patients with serious mental illnesses in the United States. A particular strength of identifying neighborhood-level risk factors is that, unlike gender or age, these factors are modifiable and have the potential to positively influence a patient’s level of engagement and the course of his or her mental illness. If future studies show that neighborhood characteristics directly affect service utilization (e.g., if certain neighborhood characteristics are barriers to patients receiving mental health care) policy makers and program planners would need to take this finding into account. Increasing awareness of the structures that shape clinical interactions can inform planning of the location and design of mental health services as well as cross-collaborations between mental health services and other sectors, such as housing, residential design and development, urban planning and zoning, and transportation.