In a hospital, persons with severe mental illnesses, such as schizophrenia, bipolar disorder, and severe anxiety and depression, often receive disjointed care when admitted for acute general medical conditions (
1). Inpatient medical services are typically not equipped to manage individuals experiencing agitation or paranoia (
2). Moreover, inpatient medical teams often are not aware of the range of supportive services in the community or of the need for intensive integration of mental, social, and general medical resources after discharge (
3).
Previous studies have examined the effects of specialized hospital units—also known as med-psych units or complexity intervention units (
4)—created to address the needs of patients who are too medically ill for a psychiatric unit and too psychiatrically ill for a medical unit (
5–
8). In a recent review of five med-psych units, Chan et al. (
8) noted that despite the successes of these units with regard to patient and staff satisfaction and overall cost reductions, hospital discharge planning remained a significant challenge. In this article, we describe a med-psych unit that was created in 2007 as a complement to a primary care clinic that was co-located with psychiatry services for 14 years. From its inception, the inpatient medicine in psychiatry (IMIP) unit had a dual goal: to provide optimal acute medical care targeted to persons with severe mental illnesses and to provide person-centered discharge planning to help patients succeed in the community.
As a first step to determine the impact of the IMIP unit, we measured three process metrics routinely reported by the hospital to monitor care-related parameters: length of stay, discharge to community settings (rather than to institutional or long-term care), and readmission rate. These metrics have been used previously to assess the effects of med-psych units (
5,
9–
11). Results from such studies have been variable, likely as a result of unit-specific differences in patient characteristics and treatment approaches. For example, one med-psych unit focused on providing psychiatric stabilization in the context of acute medical illness and reported a shortened average length of stay after implementation (
12). In contrast, a med-psych unit that provided psychotherapy for patients with somatoform disorders reported a longer length of stay (
5).
We tested three related hypotheses, comparing the IMIP unit to other acute medical units in the same medical center that admitted similar patients. With the IMIP’s multidisciplinary approach to assessment, management, and discharge planning, we hypothesized that the unit would have a shorter length of stay, a greater proportion of patients discharged to community versus institutional placements, and lower readmission rates.
The IMIP Unit
The IMIP unit was opened in 2007 by the Department of Psychiatry at the University of Rochester Medical Center, with collaborative planning from the Department of Medicine, with 10 beds, which grew to 20 beds in 2010. The Department of Psychiatry provides operational and budgetary oversight and is responsible for hiring and credentialing the nursing staff and medical providers. The initial medical director was a dual-boarded physician (internal medicine and psychiatry) who also ran the department’s primary care clinic for patients with severe mental illnesses and substance use disorders. Together with a nurse manager who was hired from the University of Rochester Medical Center’s Department of Medicine, the medical director hired primarily medically trained nurses, nurse practitioners, and physician assistants who had been working in various departments in the hospital. Once hired, staff received an orientation to psychiatry (described below). A social worker was drawn from the hospital’s inpatient medical social work services. As the IMIP unit expanded, the Department of Psychiatry hired additional physicians trained in family medicine and internal medicine, as well as nurse practitioners and physician assistants. All physicians had primary appointments in psychiatry and secondary appointments in family medicine or internal medicine. Several physicians, nurses, and nurse practitioners had experience in the department’s primary care clinic for patients with severe mental illnesses.
At the time of data collection (2016–2018), most nurses working on the unit received 1 week of psychiatric nurse orientation, 2 days of medical-surgical nurse orientation, and 8 to 12 weeks of supervised on-the-job training. In these sessions, topics covered include substance use disorders, personality disorders, mood disorders, and psychotic disorders. Nurses learned important communication strategies and skills, such as de-escalation techniques and how to communicate with a patient who has paranoia or delusions. Nurse practitioners and physician assistants participated in a longer orientation with seasoned psychiatric and medical staff and attended parts of the psychiatric nursing orientation. During the study, two social workers were on the unit who had extensive experience working with older adults; one also had community mental health expertise. Typically, medical physicians participated in ongoing continuing medical education, including weekly case presentations and didactics focused on the integration of medicine and psychiatry. The role of psychiatric providers is described in more detail below.
Although situated in the psychiatry wing of the University of Rochester Medical Center, Strong Memorial Hospital, the IMIP unit operates under a medical license and is inspected by the New York State Department of Health, rather than by the Office of Mental Health. The placement of the unit in the psychiatry wing of the hospital facilitates communication between IMIP staff and staff on nearby psychiatric floors, who are available to help out in the event of acute psychiatric emergencies (e.g., severe agitation or aggression).
A Person-Centered Approach to Help Patients Succeed in the Community
Person-centered health care focuses on the self-identified needs of patients and often crosses the artificial boundaries of medical, psychiatric, and social services (
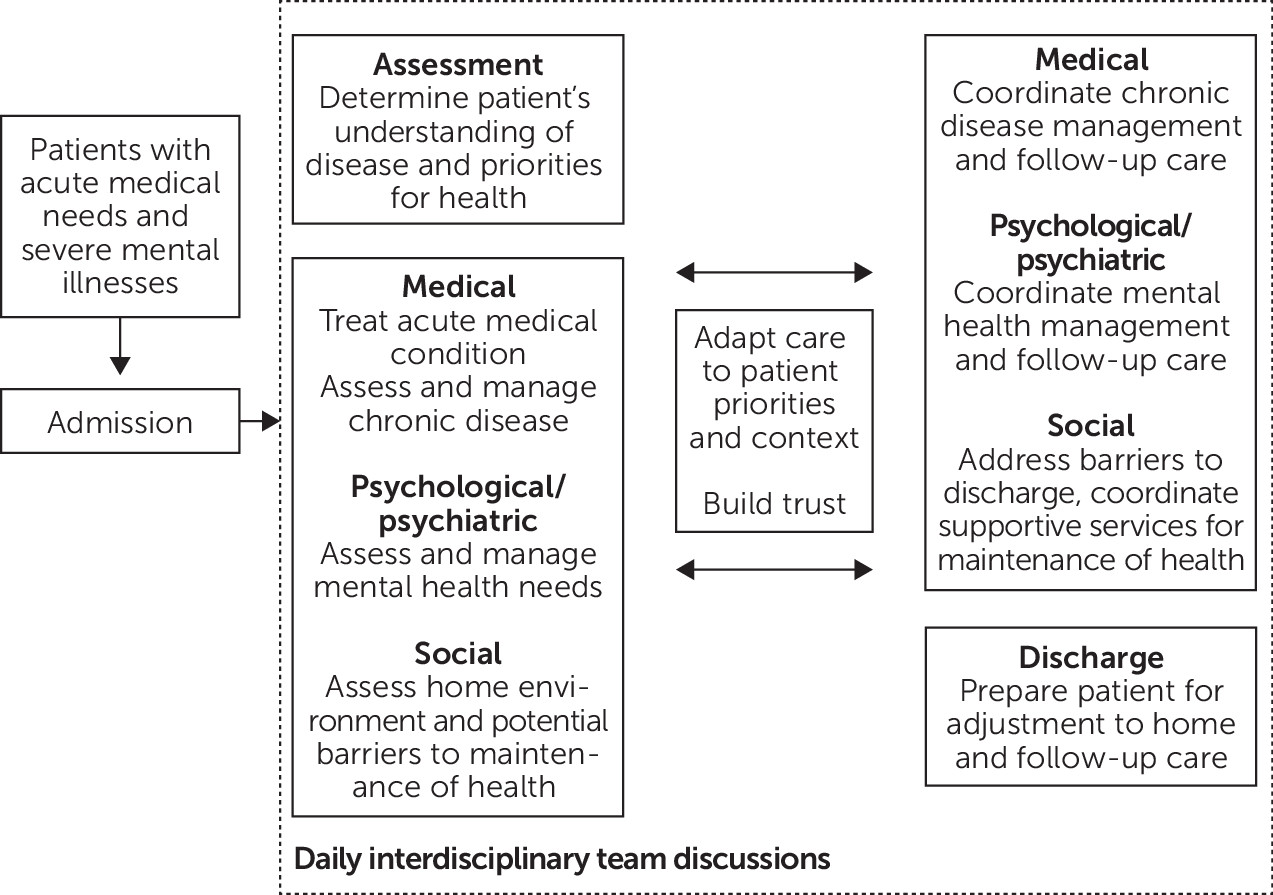
13). To help patients with severe mental illnesses succeed in maintaining their health after hospitalization, the IMIP unit takes an explicitly integrated biopsychosocial approach to anticipate patients’ near- and longer-term needs (
Figure 1). Patients with severe mental illnesses who require acute medical care are admitted directly from the emergency room or other medical units in the hospital, particularly intensive care units; admission decisions are made by the IMIP admitting physician.
After a patient is admitted, basic psychiatric assessments are incorporated as part of standard medical and nursing evaluations. Although psychiatric consultations are provided on an “as-needed” basis by the department’s psychiatric consultation-liaison team in a fashion typical of many hospitals (
14), a consultation psychiatrist or advanced practice provider serves as the psychiatric “liaison to the unit.” He or she attends the daily IMIP interdisciplinary work meetings. In addition to helping to problem solve with the interdisciplinary team, the psychiatrist assesses and manages acute psychiatric needs and coordinates follow-up psychiatric treatment. Although communication happens between psychiatric and medical providers throughout the day, key discussions occur during daily interdisciplinary team rounds, in which physicians and advanced practice providers, nursing staff, social workers, and consultants discuss each patient from medical, psychological/psychiatric, and social perspectives. (A checklist used at these meetings is included in an
online supplement to this article.) In addition to focusing on immediate clinical stabilization of patients, the meeting is used to consider chronic medical disorders, future psychiatric treatment after hospitalization, and evolving social needs (
Figure 1). Hospitalization on the IMIP unit serves as an opportunity to develop a long-range comprehensive treatment plan that aims to ensure effective, stable discharge—requiring both an intensive person-centered approach to address immediate acuity and safety concerns and a rigorous biopsychosocial assessment that requires clinicians and staff to stretch their view beyond near-term stabilization in the hospital to ensure continuity of care and future community stability through close collaboration with the patient’s primary care physician and mental health providers.
Methods
Participant Inclusion and Exclusion Criteria
Patients were included in the study if they were age 18 or older on admission, were assigned one or more diagnostic codes for mental disorders (i.e., ICD-10 codes with F prefix; see online supplement for a list of codes), and were admitted as an emergency (as opposed to an urgent or elective admission) to a non–intensive care, general medical-surgical unit. We excluded patients who were admitted to an acute rehabilitation unit or observation unit, patients for whom the discharges were coded as “expired” or “left against medical advice,” and patients who were discharged to medical rehabilitation units (e.g., after hip fracture).
Health Care Process Metrics
After review and approval of the protocol by the University of Rochester Research Subjects Review Board, we obtained health care process metrics from the electronic medical record data at the University of Rochester Medical Center, Strong Memorial Hospital. The following variables were extracted for patients discharged from January 1, 2016, through May 31, 2018: unique individual medical record number, patient demographic characteristics, dates of admission and discharge, the hospital’s inpatient unit identifier, admission status (emergency, urgent, or elective), discharge disposition (e.g., discharged to home, skilled nursing facility, or another hospital), primary payer type (commercial, Medicare, or Medicaid), up to 20
ICD-10 diagnosis codes, and All Patient Refined Diagnosis Related Groups (APR-DRG) severity of illness categories (referred to as “illness severity” in this study, in the following categories: minor, moderate, and major) (
15).
IMIP Comparison Study
In conceptualizing the analysis, we considered the IMIP unit as an inpatient unit–level intervention—that is, all patients treated in the IMIP unit were considered to be in the intervention group, regardless of their medical conditions or the types of care they received in the IMIP unit. Accordingly, the comparison group—i.e., patients who were not treated in the IMIP unit—was defined by the inpatient units from which the patients were treated, rather than by individual patient characteristics.
After adjustment for patients’ demographic characteristics, medical complexity, and acuity that may have confounded the results, we compared unit-level means or proportions between the IMIP intervention group and the non-IMIP comparison group on length of stay, discharge to home (self or with family), and readmission during the 2-year period.
Subsample Comparisons
We posited that the impact of the IMIP unity would be greater for patients with more severe mental illnesses—that is, the IMIP unit’s comparative advantage would be more pronounced for patients who require more targeted and biopsychosocially integrated approaches. Thus, we explored whether reductions in length of stay were greater for patients with more complex psychiatric comorbidity. Specifically, we created a subsample of patients limited to those with a combination of one or more psychiatric disorder diagnosis codes plus one or more substance use disorder diagnosis codes. This subsample, labeled “higher psychiatric complexity,” represented patients with more complex psychiatric needs.
Analytic Plan
Differences in patient characteristics between the IMIP unit and the comparison units were first assessed via bivariate t tests. Subsequently, multivariate regression models were used to estimate the IMIP unit’s impact, with control for potential confounders, on the following three dependent variables of interest: length of stay, measured in days; a binary indicator that equaled 1 if the patient was coded as having been discharged to home and 0 otherwise; and a binary indicator that equaled 1 if a given discharge for a patient was followed by another admission within 30 days of the discharge and 0 if there was no readmission within 30 days. The key explanatory variable in all the regression models was a binary indicator that equaled 1 if the patient was discharged from the IMIP unit and 0 if not discharged from the IMIP unit.
For length of stay, a multivariate linear regression model was used, treating length of stay as a continuous variable. In a sensitivity analysis in which a Poisson or a negative binomial regression model was used instead, the results were similar. For the probability of discharge to home and of 30-day readmission, a logistic regression model was used in which the IMIP unit’s impact was represented as odds ratios (ORs). Because multiple discharges may be associated with a single patient over time, clustered robust standard errors were obtained to allow correlation of the error terms within each patient (
16). All statistical analyses were conducted using Stata, version 15.
In all the regression models, the following covariates were included to account for potential confounders, specifically those that captured case-mix differences between the IMIP unit and the comparison units: patient age category (18–45, 46–60, 61–75, and >75), sex, race (white versus nonwhite), and payer type (commercial, Medicare, or Medicaid). Also, APR-DRG severity-of-illness category (
17), Charlson Comorbidity Index (
18) (calculated based on the 20
ICD-10 diagnosis codes), and count of medical diagnosis codes (i.e.,
ICD-10 codes with prefixes other than F) were included as measures of medical complexity and case mix (
19). Furthermore, interaction effects between age and gender and between the count of medical diagnosis codes and APR-DRG severity-of-illness categories were included in all the regression models to further adjust for case mix. Finally, indicator variables corresponding to each calendar year and month of admission were also included to capture seasonality and secular trends (see table in the
online supplement for the full regression output).
To check for the robustness of the results, another set of sensitivity analyses was conducted in which the previously excluded patients (i.e., those for whom the discharges were coded as “expired” or “left against medical advice” and those who were discharged to medical rehabilitation units) were included in the sample.
Results
Table 1 shows descriptive characteristics of patients who were discharged from the IMIP unit versus comparison patients drawn from the hospital’s general units, for both the full sample and the subsample with higher psychiatric complexity. IMIP patients appeared to be younger and to have higher counts of psychiatric diagnosis codes, versus those in the comparison units. At the same time, the IMIP patients had lower Charlson Comorbidity Index values, suggesting that they tended to have fewer comorbid general medical conditions, versus those in the comparison units. In addition, patients in the IMIP unit had shorter stays and a higher probability of being discharged to home. Similar patterns were generally observed in both the full sample and the subsample, although the difference in the 30-day readmission rates between IMIP and non-IMIP patients was not statistically significant in the full sample and the proportion of patients with Medicaid was much higher in the subsample.
With respect to prevalence of psychiatric (F code) diagnoses,
Table 2 shows that the IMIP patients in the full sample were significantly more likely than those in the comparison units to have F code diagnoses, a pattern consistent across all F code diagnostic categories except for cognitive impairment (see
online supplement for a list of diagnosis codes included in each category). Similar patterns were also observed in the subsample, although the prevalence of mood disorders was slightly lower among IMIP patients, versus patients in the comparison units (note that the prevalence of substance use disorder diagnoses was 100% because of the subsample definition).
The impact of the IMIP unit on health care process metrics is shown in
Table 3. The regression-adjusted estimates of the IMIP unit’s impact are shown for the full sample, as well as for the subsample. Consistent with our expectation, the estimated IMIP unit’s impact appeared to be larger among the patients with higher psychiatric complexity (subsample), as indicated by an average length of stay shorter by nearly 1 day, higher odds of discharge to home (OR=1.51), and lower odds of 30-day readmission (OR=0.69), all of which were statistically significant. Note that these associations were observed even after the analysis controlled for the extensive list of covariates in the regression models that captured potential confounders (see
online supplement for a table with the complete regression outputs). Moreover, the results of the sensitivity analysis in which the previously excluded patients were added back into the sample as described above were comparable to the main results and did not change the conclusion (see
online supplement).
Discussion
In this study, we assessed the impact of the IMIP unit, a person-centered medical unit, housed in a psychiatry department, that explicitly implements an integrated, pervasive, multidisciplinary team approach. The unit staffing model emphasizes training to teach strategies such as de-escalation and consistency in communication and incorporates an efficient presence of psychiatric consultants. Daily interdisciplinary meetings are guided by a biopsychosocial conceptual model. An important goal of the team-based approach to care is to identify approaches that can help patients improve in the hospital and succeed in the community after discharge. The IMIP unit may be unique in its broader clinical focus, compared with other med-psych units described previously (
8,
11,
20,
21), which were reported to deal with more narrowly defined patient groups, such as those with psychosomatic disorders (
5) or those with higher psychiatric acuity (
7).
We found that compared with patients on the comparison units, those on the IMIP unit were more likely to be younger and tended to have fewer comorbid general medical conditions and thus could be considered to have less severe conditions. However, the prevalence rates of psychiatric and substance use disorders were much higher among the IMIP patients. Notably, IMIP patients had a higher prevalence of nicotine dependence, which is associated with chronic medical conditions and with worse outcomes for patients with severe mental illnesses (
22,
23). Even though the study found these underlying differences, it also found evidence in support of the hypothesis that IMIP admission was associated with a shorter stay, a greater percentage of discharges to self or family care, and a lower 30-day readmission rate, particularly among those with higher psychiatric complexity—findings that may indicate both potential cost-of-care savings and enhanced quality of care. Although assessing the impact on other medical services was beyond the scope of this study, we also suspect that the IMIP unit had an impact on these services by drawing patients who posed substantial behavioral management challenges from the general medical floors, especially patients with co-occurring substance use and mental disorders. Indeed, this impression has been reinforced by the hospital’s seeking to expand the IMIP service from 20 to 32 patients by opening an additional unit.
Our results reinforce previous findings that integrating general medical and psychiatry services on a med-psych unit may reduce length of stay and likelihood of admission to a long-term care facility (
11). More recent models of hospital integration, such as “pro-active” psychiatry consultation, have also been shown to be associated with a reduced length of stay (
24). In addition, our results indicate that IMIP care was associated with lower 30-day readmission rates—a finding that has not been previously reported.
In terms of limitations, a prospective trial that randomly allocated persons with F code diagnoses to different units would have been a stronger design. However, randomization to units is not feasible in a busy medical center that operates near or above capacity. A second potential limitation is that despite the extensive list of covariates in the regression models we employed to account for potential confounding due to case mix, the results may still be subject to some unobserved bias. As such, it is difficult to make causal inferences on the basis of our data. Finally, it is important to note that our readmission data were limited to readmission to University of Rochester Medical Center, Strong Memorial Hospital only. Even though most patients discharged from a given hospital are generally readmitted to the same medical system (
25,
26), we had no method of assessing whether Strong Memorial Hospital patients, including those from the IMIP unit, were readmitted to other hospitals.
Our results call for further research to discern the active ingredients of IMIP admission and to ascertain whether the IMIP unit served as a meaningful moment of engagement that influenced longer-term outcomes. It will be useful to measure patient satisfaction and discharge preparedness (
27), as well as post-discharge engagement with primary care and mental health services. At the same time, we do not know whether being treated on the IMIP unit had any unintended consequences for patients. Although staff members are trained to use de-escalation techniques and take precautions to prevent agitation, future studies should include data on the use of physical and chemical restraints.
As described above, IMIP staff have ready support from psychiatric staff—regularly each day and rapidly at times of acute management challenges. Since the unit was established in 2007, IMIP staff have become more effective at using strategies to help patients who are fearful of medical procedures and in using de-escalating techniques when patients become acutely agitated. Staff have also become more knowledgeable about when to proactively ask for help from their psychiatry colleagues.
Conclusions
Persons with severe mental illnesses are dying 20 years earlier than the rest of the population (
28–
30). Most of this premature mortality arises from the early onset and rapid progression of chronic general medical conditions, such as diabetes and heart disease (
31,
32). These health disparities reflect a failure to meet the challenges associated with providing services that effectively engage patients and address their complex medical, psychiatric, and social needs (
33–
37).
The initial goal of the IMIP unit was to provide a hospital setting that serve persons hospitalized with acute medical needs and severe mental illnesses. Our findings suggest that the unit has an impact on important hospital process metrics, notably reducing length of stay and improving discharge to home and readmission rates. The historical beginnings of the unit, which grew from the department’s primary care clinic for patients with severe mental illnesses that opened in 1993, may partially account for some of the findings. Having clinicians work in both settings may facilitate continuity of care and lead to more trusting relationships between patients and the rest of the care team. These are key components of other promising care models such as the comprehensive care physician model targeted to patients with complex medical and social needs (
38). It remains to be established whether the IMIP unit and its associated primary care clinic prove to be sites of engagement that can alter the shortened life expectancy of patients with severe mental illnesses.
Finally, the IMIP unit’s location in an academic medical setting has led to educational opportunities for psychiatry and medical residents, nurses, social workers, and clinical psychologists to learn how to work collaboratively, building skills in team-based care (
14). Next steps will include assessing the impact of specialized units such as IMIP on educating clinicians about the values of comprehensive and integrated care.