Suicidality is common, with an estimated 12-month prevalence of 4% in U.S. adults (
1), and suicide prevention is a national research priority (
2). Although the literature describing interventions to address suicidality in clinical practice is growing, management of suicidality detected in research study activities, such as participant enrollment and surveys, remains understudied (
3).
Both the U.S. Food and Drug Administration and the National Institute of Mental Health have issued guidelines for developing study-specific suicide-risk management protocols (SRMPs) to address suicidal ideation and behaviors arising during research study operations (
4–
6). Nonetheless, because of the absence of empirically supported procedures to address suicidality while conducting clinical research, many studies have excluded individuals with suicidal thoughts or behavior, citing safety concerns, potential impact on study retention and outcomes, and protection of study participants (
3,
5–
7). In studies in which participants with suicidality have not been excluded, SRMPs vary widely, ranging from direct outreach by a trained mental health professional in response to every statement of suicidal ideation to multistep, automated algorithms, with direct clinician evaluation and intervention only in high-risk cases (
8–
12).
Suicidal thoughts are common, but suicide attempts are rare, and suicide risk is difficult to predict with commonly used screening tools (
1,
13). For example, although a positive screen for suicidality on the 9-item Patient Health Questionnaire (PHQ-9) predicts increased relative risk for attempted suicide, the absolute risk remains low (
14,
15). Challenges in efficient and accurate screening, combined with a need to manage study costs and demands on study staff (
11,
16,
17) and a concern about potential impacts of suicide interventions on study outcomes (
6), may lead researchers to favor low-intervention SRMPs, particularly in large pragmatic trials.
These practical concerns are weighed against an ethical one: What obligation do clinical researchers have to ensure the safety of study participants expressing suicidality? This question is particularly salient in studies involving low-income, historically marginalized communities, which are underrepresented in clinical research. In such communities, SRMP implementation may be complicated by limited availability of formal mental health services as well as by hesitation of study participants to seek treatment because of stigma surrounding depression and suicidality (
18–
20). Furthermore, distrust of mental health providers and researchers persists in some communities of color because of a legacy of racism and research abuses, such as the Tuskegee Study (
21), coupled with negative experiences, including involuntary hospitalization, when seeking treatment (
19,
22). To our knowledge, the existing literature has not addressed standards for responsible and ethical responses to suicidality arising in research in underresourced, racial-ethnic minority communities.
Here, we describe how a community-academic partnership applied a community-partnered participatory research (CPPR) framework to design a unique SRMP for use in the Community Partners in Care (CPIC) depression study, carried out in two underresourced, predominantly Black and Latino communities in Los Angeles (
23). As a variant of community-based participatory research (
24), CPPR emphasizes community-academic coleadership, co-ownership, and knowledge exchange in all research phases (
25,
26). We describe the subsequent implementation and adaptation of the SRMP using data from SRMP workgroup notes and study clinicians’ e-mail summaries of outreach calls to participants expressing suicidality. We assessed the burden of suicidality among research participants at baseline and at 6- and 12-month follow-ups. Finally, we discuss the implications of these findings and future directions for an ethical approach to addressing suicidality in clinical research involving underresourced communities.
Methods
Setting
CPIC was a group-level randomized comparative effectiveness trial designed to compare two depression collaborative care implementation approaches (
23). Participants were enrolled from 93 participating programs, including primary care clinics, outpatient mental health clinics, substance outpatient and residential treatment programs, homeless and housing services, social services, and other community-based services (faith-based organizations, hair salons, exercise centers, and park and recreation senior centers) in two Los Angeles communities. Potential participants were screened for eligibility in program waiting rooms and at events. Study surveys were completed by telephone at baseline, 6 months, and 12 months from April 2010 through March 2012. The project was approved by the institutional review board (IRB) of RAND Corporation and by Los Angeles County and other agencies requiring separate review. All participants provided informed consent.
Participants
Study eligibility was limited to adults (ages ≥18 years) speaking English or Spanish, with at least moderate depressive symptoms indicated by an 8-item PHQ (PHQ-8) (
27) score of ≥10 at screening. The analytic sample included 1,018 enrolled individuals who completed at least one survey (baseline, 6 months, or 12 months). Participant demographic characteristics have been previously described (
28). Briefly, the study sample was 58% female (N=595); was 48% Black (N=487), 40% Latino (N=409), and 8% White (N=43); and had a mean±SD age of 46±13 years. Relevant social characteristics included 53% (N=536) having multiple risk factors for homelessness, 74% (N=750) meeting federal poverty criteria, 20% (N=205) working for pay, and 54% (N=545) being uninsured. Additional details on recruitment, enrollment, and outcomes can be found in previous publications (
23,
28).
Community-Partnered Approach to SRMP Development and Implementation
Using a CPPR framework (
25,
26), a workgroup comprising academic and community partners, including a community health advocate, a nurse from a local mental health clinic, a clinical administrator in the Los Angeles County Department of Mental Health, a substance abuse agency administrator, a public health nurse, and the director of a safety-net primary care clinic developed the CPIC SRMP. The workgroup modified the SRMP described in the study grant proposal on the basis of the Partners in Care study (
29) during biweekly meetings over 4 months. The revised SRMP was reviewed at a community forum attended by >80 local stakeholders, including representatives from community groups, consumer and faith-based organizations, local health clinics, and social services agencies, and was subsequently reviewed and approved by the CPIC Executive Committee. The SRMP content and modifications are described in the Results section.
Data Sources
Participants self-reported gender and race-ethnicity at screening. Suicidality screening was conducted by telephone at baseline and at the 6- and 12-month follow-up surveys. Qualitative data included meeting notes from the SRMP development workgroup and study clinicians’ e-mails summarizing contact with study participants endorsing suicidal ideation. E-mail text was abstracted into Microsoft Excel and included participant study identification; event date; study data collection phase (i.e., screening, baseline, or 6- or 12-month survey); study clinician; assessment of imminent risk; intervention, such as referral to a clinic or emergency room or a 911 call; and narrative comments.
Suicidality Screening Measures
Screening for suicidality with the baseline survey utilized the following Mini-International Neuropsychiatric Interview (MINI) (
30) item: “Over the past 2 weeks, when you felt depressed or uninterested, did you repeatedly consider hurting yourself, feel suicidal, or wish that you were dead? Did you attempt suicide or plan a suicide?” At 6 and 12 months, screening utilized the following PHQ-9 (
31) item: “In the past 2 weeks, have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” In the modified SRMP, participants responding affirmatively to the PHQ-9 suicidality item were asked the follow-up question: “Are these thoughts bothering you now?”
Statistical Analysis
A chi-square test of independence was performed to examine the relationship between demographic characteristics (race-ethnicity and gender) and cumulative prevalence of suicidal ideation. We ran these analyses with SAS, version 7.4, software.
Qualitative Analysis
Workgroup meeting notes were summarized to describe the process of SRMP development and adaptation. For analysis of outreach call notes, three study team members drafted codes based on both a priori areas of interest (e.g., “problems with access to care” and “referral provided”) and emergent themes (e.g., “knows how to get help”). After several rounds of analysis in which e-mails were independently coded and reviewed for agreement, a final codebook was developed and applied.
Results
Community-Partnered SRMP Themes
During initial workgroup meetings, several broad themes emerged that guided the SRMP development, adaptation, and implementation. Community partners emphasized the importance of ensuring participant safety over and above IRB requirements, with a high priority placed on suicide prevention. At the same time, community partners were conscious of the stigma of mental illness and of potential distrust of law enforcement involved with mental health crisis interventions. Both community and academic partners shared concerns about ensuring the feasibility of timely implementation of SRMP procedures within the constraints of study resources. Finally, the group agreed that an iterative process, based on CPPR principles, would be used during study implementation to modify the SRMP if necessary. Community feedback and subsequent modifications are summarized in
Table 1.
SRMP Procedures
The SRMP was activated in response to suicidality endorsed on the MINI or PHQ-9 or disclosed to survey staff. After the activation, staff immediately paged the on-call study clinician (a licensed physician or psychologist) and shared the participant’s name, telephone number, preferred language, and reason for SRMP activation. Within 30 minutes, the study clinician placed an outreach call to the participant, with ongoing attempts if the initial call was unsuccessful. For Spanish speakers, translation was provided via a three-way call. At least one of six study clinicians was on call during all hours of survey operation, including evenings and weekends, over an 18-month period.
Study clinicians received guidelines for follow-up and resources for referrals. If the clinician determined that a participant was at high risk for self-harm, the clinician would facilitate a referral to an emergency department or, in case of imminent risk and as a last resort, call 911. Participants deemed at low immediate risk, and with a current outpatient provider, were coached in how to discuss suicidality with the provider; if assistance was needed, permission could be obtained for the study clinician to speak to the provider. For participants with no current provider, the study clinician would provide a referral to a partner mental health or primary care agency where the patient would be seen within 2 business days, with a “warm handoff” during which study staff would speak directly to a clinic staff member.
Suicidality Prevalence
Suicidal thoughts were common, endorsed by 32% of study participants at one or more of the three survey time points, and by 15% of participants at baseline, 24% at the 6-month follow-up, and 20% at the 12-month follow-up (
Table 2). Of all participants endorsing suicidal thoughts during the study (N=329), 215 (65%) did so at a single survey time point, 89 (27%) at two time points, and 25 (8%) at all three time points. As shown in
Table 3, overall prevalence of suicidal ideation was higher for men than for women (37% vs. 29%; p=0.01); no statistically significant differences were detected among different race-ethnicities.
SRMP Modification
As the study progressed, we noted that no participants had been deemed to be at high immediate risk of self-harm on the outreach calls, despite the high frequency of SRMP activation; some participants reported passive thoughts of death or hopelessness without intent or plan to act on those thoughts, whereas others reported current resolution of suicidal thoughts. Midway through the 6-month follow-up survey, after discussions involving community partners, research staff, and the RAND IRB, the decision was made to modify the SRMP (
Table 1). Subsequently, participants screening positive for recent suicidality on the PHQ-9 (used for the 6- and 12-month surveys) were asked an additional question to assess current suicidality: “Are these thoughts bothering you now?” Outreach was triggered only when a participant answered affirmatively. Before the SRMP modification, this key question was posed by study clinicians during the outreach calls, and its incorporation into the survey limited outreach calls to assessment of ongoing suicidal ideation, reducing burden on the study staff.
SRMP Implementation
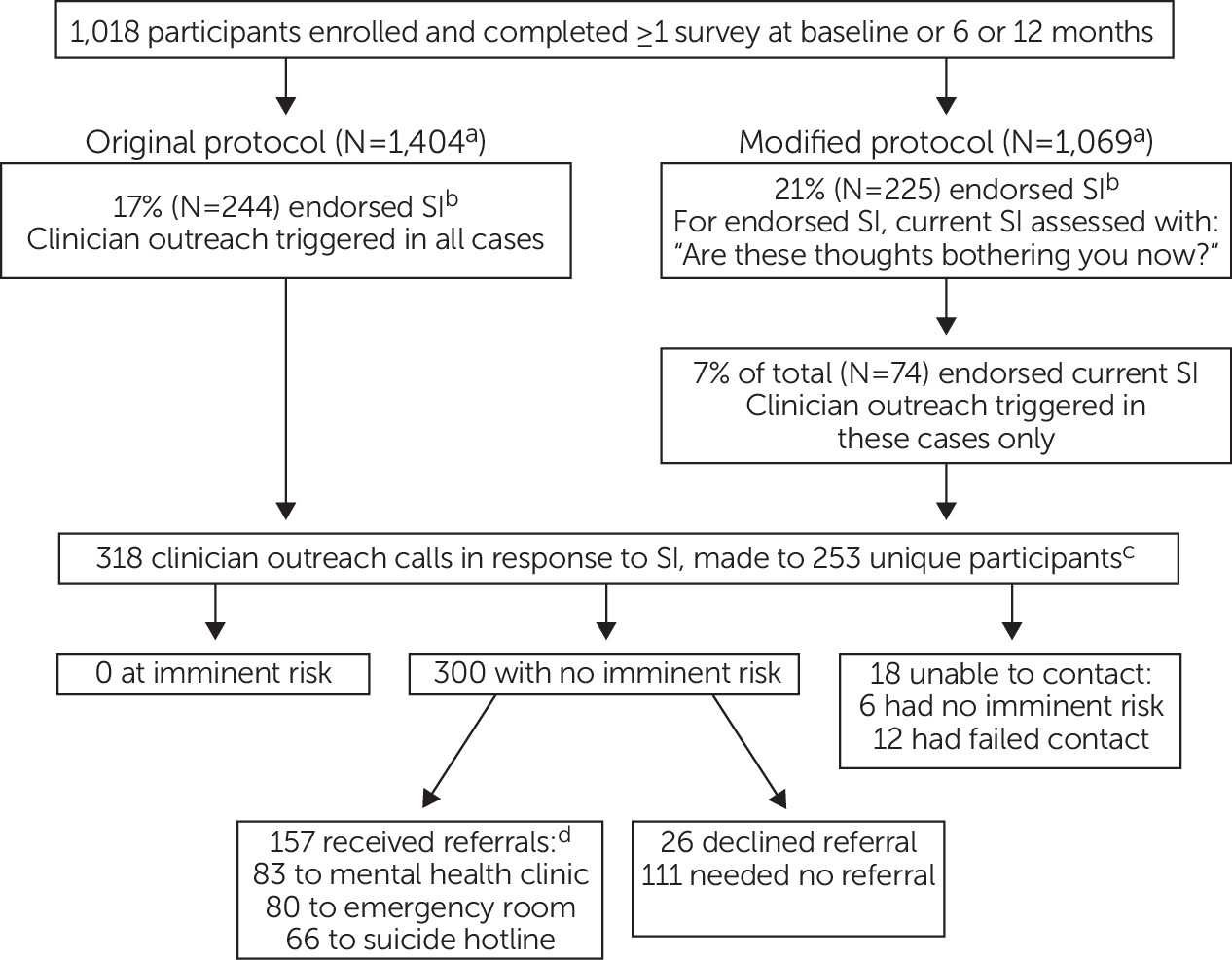
Of 1,018 participants surveyed, study clinician outreach was triggered in 318 instances across 253 unique participants during telephone surveys at three time points (
Figure 1). Participants were successfully contacted in 300 instances; all of them were found to be at low immediate risk for suicide. In 157 outreach calls, participants were provided one or more referrals, which included mental health clinics (N=83), emergency room recommendations for future reference (N=80), and a suicide hotline number (N=66). Referrals were either declined or deemed unnecessary (e.g., because the participant was already in treatment) in 137 calls. Referral data were missing for six calls. Study clinicians were unable to reach a participant in 18 cases, six of whom were determined to be at low immediate risk on the basis of further discussion with the participant’s study survey administrator or outpatient clinician; the 12 remaining cases were coded as lost to follow-up.
As detailed above, the SRMP was modified midway through the study, leading to a higher threshold for study clinician outreach. Under the original protocol, 244 calls were triggered, representing 17% of telephone surveys (N=1,404). Under the modified protocol, 74 calls were triggered after 225 initial reports of suicidal ideation, representing 7% and 21% of telephone surveys (N=1,069) endorsing current and previous or current suicidal ideation, respectively. Outreach frequency did not vary by CPIC study arm (see online supplement to this article).
In the 4-year follow-up of the CPIC study, which included intensive tracking of all enrolled participants and review of death records, no known suicide deaths occurred among the study participants. One study participant was hospitalized for a nonfatal suicide attempt 3 weeks after the baseline survey, at which time he had endorsed suicidal thoughts, received a study clinician outreach call, and was found to be at low immediate risk for suicide.
Participant Responses to Study Clinicians’ Outreach
Key themes identified from study clinicians’ notes included discussion of participants’ current stressors, such as personal or family illness; housing, financial, or legal problems; trauma history; and difficulty either obtaining or remaining in mental health treatment. Participants often expressed surprise and appreciation in response to the clinicians’ outreach. Quotes from participants included the following: “This program is wonderful—it should be a national resource for communities like ours,” “I wish this project could be available to everyone in the community,” and “You’re the only person who has ever called me just to check on how I’m doing.” Some participants expressed skepticism about treatment: “What would an old person like me do talking to someone about how I feel? I mean, how could it help?” No complaints were noted about violation of privacy.
Discussion
Exclusion of people of color from clinical research has limited the widespread applicability of research findings (
18,
32). Correction of this exclusion is increasingly viewed as a national priority, highlighted by a mandate that studies funded by the National Institutes of Health address inclusion of women and racial-ethnic minority groups (
33). In our study, community stakeholders made clear that conducting research in Black and Latino communities with limited access to health care and a legacy of negative interactions with the academic and medical establishments requires careful consideration of how to address suicidality ethically and responsibly.
Using a CPPR framework, our community-academic partnership developed an SRMP that significantly differed from those in the published literature, grounded in community partners’ emphasis that the protocol go beyond basic risk assessment and mitigation and actively prevent any study-related suicides. First, the SRMP featured a low threshold for rapid, high-quality outreach, assessment, and brief counseling by a licensed clinician. Although the study was not designed to measure the impact of the clinician outreach, the outreach calls themselves may have served as a therapeutic intervention. Second, the SRMP included arrangements with local outpatient clinics to facilitate expedited mental health intake for individuals not currently in treatment. Given that limited access to appropriate care is a well-established barrier to depression treatment, particularly for Black and Latino individuals (
18,
34,
35), these referrals may have served as an important bridge to treatment.
Outreach calls were well received but labor intensive, and it was challenging to ensure adequate staffing to respond to the high volume of positive screenings for suicidality. Thus, midway through the study, the protocol was modified to raise the threshold for study clinician outreach. Similar to findings by Corson et al. (
36), only about one-third of participants endorsing the PHQ-9 screening item reported ongoing suicidality in the follow-up question (“Are these thoughts bothering you now?”). Given the poor predictive value of many suicide screening items (
13), researchers may consider incorporating key follow-up questions into study surveys, as we did in the modified protocol. Our results highlight the tension around how to design an SRMP that reflects a commitment to the safety of the study community while also being feasible to implement, particularly in large trials such as this one. Academic-community partnerships must weigh these considerations when developing future SRMPs.
The CPIC study was not designed to track suicidality or SRMP implementation, leading to several limitations. First, clinicians’ e-mails summarizing outreach calls varied in detail, limiting the depth and precision of the analyses. Second, two different suicidality screening tools were used: the MINI at baseline and the PHQ-9 in subsequent surveys. Both items address thoughts of self-harm or death, but the MINI includes the word “suicide” (see Methods for full items); this difference may explain the lower endorsement when the MINI was used (15%) rather than the PHQ-9 (22%). Finally, because of the somewhat nonspecific language of the screening items, our results do not provide detailed information on forms of ideation, which may range from thoughts of nonsuicidal self-harm, to passive thoughts of death, to a specific suicide plan.
The results of our study reveal a high burden of suicidality among individuals with depression in two low-income, predominantly Black and Latino communities in Los Angeles, with 32% of the participants endorsing suicidal ideation at one or more time point. Despite researchers’ concerns about community stigma associated with depression and suicidality, the participants largely welcomed and appreciated the outreach calls by the study clinicians. Our data on SRMP implementation were included in an annual report shared with community members and stakeholders, who expressed appreciation for the efforts taken to ensure the safety of potentially vulnerable study participants. We believe that engagement of community stakeholders in SRMP development facilitated the high degree of acceptability of SRMP procedures by both study participants and the broader community.
Conclusions
This work adds to the limited literature on the development of SRMPs for clinical and services research and, to our knowledge, is the first to address the particular implications of SRMPs in underresourced communities. Further research is necessary to determine the impact of interventions related to suicidality in research studies and whether similar protocols could be implemented as part of community services in response to suicidality and beyond the context of research study operations. We argue that government agencies, funders, and investigators have an obligation to assess the feasibility and effectiveness of efforts to address suicidality emerging in research studies, particularly in those involving underresourced communities.