Coordinated specialty care (CSC) programs provide multidisciplinary clinical services for young adults experiencing first-episode psychosis (FEP) and emphasize rapid referral processes to reduce the duration of untreated psychosis and improve clinical and functional outcomes (
1,
2). The extensive literature on CSC programs includes research related to pathways to care, service use, and treatment outcomes (
2). However, few studies have examined disparities of CSC service provision among the rapidly growing Hispanic ethnic group in the United States. Further research is needed to better understand demographic, clinical, and socioenvironmental characteristics of Hispanic youths who are referred to CSC and factors associated with their enrollment.
Disparities in mental health service use have been reported for Hispanics experiencing FEP. Using commercial insurance data, van der Ven et al. (
3) found that the probability of outpatient mental health services use was 30% lower among Hispanics ages 14–30, compared with non-Hispanic Whites, after the analysis adjusted for household income as an indicator of socioeconomic status (SES). This study did not examine service use specifically within CSC programs, in which engaging youths is more strongly emphasized than in standard outpatient services, and was limited to individuals with commercial insurance.
A secondary analysis of the national RAISE trial (Recovery After an Initial Schizophrenia Episode) (
4), which compared CSC to standard care, found that race and ethnicity of FEP patients were not associated with differences in psychiatric symptoms in the group receiving CSC. However, Hispanic participants’ families were significantly less likely to receive family psychoeducation, compared with families of non-Hispanic White participants. Hispanic participants (who accounted for only 19% of the sample) were more likely to receive only medication management, compared with non-Hispanic Whites.
Research regarding pathways to care for Hispanic youths experiencing FEP is more limited. Some data suggest that individuals from minority groups who are experiencing FEP are more likely than their non-Hispanic White counterparts to interact with law enforcement and may experience higher rates of involuntary inpatient hospitalizations (
4,
5). In a cross-sectional study, López et al. (
6), found that U.S. Hispanics with FEP and their caregivers had a poor understanding of psychosis, which was associated with a reduced likelihood of professional help seeking.
Consistent with current epigenetic etiological models of psychosis, studies of non-U.S. populations suggest that the reported higher incidence rates of FEP among migrant groups and racial-ethnic minority groups may be attributable to specific socioenvironmental factors, such as urbanicity, racial-ethnic density, or low SES (
7–
9). These same factors have also been associated with disparities in accessing care (
10). Most of these studies focus on Black minority groups from Northern Europe. Researchers in the United States have not yet explored the impact of socioenvironmental factors on incidence of psychosis or access to care among Hispanics experiencing FEP.
New Mexico’s population has the highest percentage of Hispanics (49%) of any U.S. state, which is reflected by the ethnic-racial profile of participants in the only CSC program in the state (
11). The term “Hispanic” encompasses many groups that differ across geographic region, region of origin, primary language and dialect, age, and generation of immigration. New Mexico is unique in that many residents identify as Hispanic in terms of their Spanish ancestry, and the state has a smaller proportion of first- and second-generation immigrants, compared with most states. Regardless of immigration status or length of time in the United States, most individuals who identify as Hispanic in New Mexico are bilingual (
11). This provides an opportunity to address gaps in knowledge regarding demographic, clinical, and socioenvironmental characteristics among Hispanics referred to and enrolled in CSC.
The objective of this retrospective study was twofold. First, the study examined referral sources and demographic, clinical, and socioenvironmental characteristics among Hispanics referred to and enrolled in CSC, compared with White non-Hispanics and persons from other minority groups. Second, the study explored factors associated with enrollment in CSC to determine whether Hispanic ethnicity was a significant factor and whether any interactions between demographic, clinical, and socioenvironmental factors exist.
Methods
The University of New Mexico’s Early CSC program provides CSC services statewide to individuals ages 15–30 who have experienced FEP within the past year. The Early CSC program’s clinical team assesses referrals for eligibility. Qualifying diagnoses include primary psychotic disorders, either affective or nonaffective. Individuals whose psychotic symptoms are better explained by medical conditions, substance use disorders, posttraumatic stress disorder, or other nonprimary psychotic disorders and individuals with an IQ below 70 are not eligible.
Data Collection
A retrospective review was completed for all individuals referred to the Early CSC program between January 1, 2018, and January 1, 2020. Referral sources were recorded from initial contact notes in electronic medical records (EMRs) and grouped as inpatient mental health services, outpatient mental health services, or non–mental health services (family, schools, or self-referrals). Demographic and clinical data extracted from EMRs included race, ethnicity, sex, age, insurance type, and residential zip code. Three groups were identified on the basis of race and ethnicity: White Hispanic, White non-Hispanic, and other minority groups. Clinical data on diagnosis and substance use at the time of intake were available only for individuals who enrolled. Diagnosis was coded as nonaffective, affective, or unspecified psychoses. Substance use was coded as either present or absent.
Residential zip codes were cross-referenced with publicly available socioenvironmental data from two sources. First, 2018 U.S. Census data were extracted to determine the proportion of residents in each zip code who were high school graduates, living below the poverty level, unemployed, and living in households that were primarily English or Spanish speaking (
12). “English spoken at home” refers to the percentage of the population ages 5 and older who primarily speak English. “Spanish spoken at home” refers to the population ages 5 and older who, if they speak a language other than English, speak Spanish at home. Unemployment rates are based on the percentage of the workforce population ages 16 and older currently without work.
Additional data were extracted from the Environmental Systems Research Institute (ESRI), which collects and aggregates data from reputable sources, such as the Census Bureau, in addition to modeling its own data (
13). Measures gathered from ESRI by zip code included the overall crime index, diversity index, median household value, and per capita income growth. Applied Geographical Solutions maintains the overall crime index, and Feature Service maintains the other three measures. The overall crime rate is a measure of total crime committed by block, weighted by population size and aggregated to national totals. A value of 100 is the national average; values above or below 100 represent percentage changes relative to this benchmark. The diversity index represents the likelihood that two persons, chosen at random from the same area, belong to different racial or ethnic groups ranging from no to complete diversity (0–100). Median home value measures middling home values by zip code. ESRI’s measure of per capita income growth is forecasted at the block level and aggregated up to varying levels, including zip code, and is designed to distinguish local variation in changes in income inequality and urbanicity.
Participants
Over the 2-year period, the Early CSC program received 224 referrals. Referrals still in process (N=5) and those of unknown ethnicity (N=25) or race (N=14) were excluded, resulting in a final data set of 180. Among all referrals, 32% (N=58) were ineligible, and 68% (N=122) were eligible for services. Of all the eligible referrals, 75 individuals (61%) enrolled in the Early CSC program and 47 (39%) individuals never enrolled.
To address the second objective, data for the subset of eligible individuals (N=122) were analyzed separately to explore factors associated with enrollment. Eight additional records were missing data and were subsequently excluded from this analysis, resulting in a final data set of 114 (74 enrolled and 40 not enrolled).
The institutional review board of the University of New Mexico Human Research Protection Office approved this study (no. 20–076).
Statistical Analysis
Objective 1.
Nonparametric tests were used because of the nonnormal distribution of the data. Dichotomous comparisons were analyzed with Fisher’s exact test. Larger contingency tables were analyzed by using chi-square tests. Dichotomous variables were compared with continuous data with the Wilcoxon Mann-Whitney U test, and nominal variables were compared with continuous variables with the Kruskal-Wallis test. Continuous variables were compared with the Kendall rank correlation coefficient. Secondary analyses were applied when significant relationships were identified: pairwise nominal independence tests following Fisher’s test and chi-square test with Bonferroni correction, and Dunn tests following the Kruskal-Wallis test. Odds ratios (ORs) and 95% confidence intervals (CIs) were generated for dichotomous and categorical variables by transforming each into a series of dummy variables, indicating the condition (i.e., commercial insurance versus other types). ORs and CIs could not be calculated for those enrolled in CSC because of the small sample size.
Objective 2.
A random forest model was generated to classify eligible individuals as enrolled or not enrolled, according to individual demographic factors and selected zip code–level socioenvironmental factors. A random forest model is a machine learning method, based on growing
n decision trees and applying them to a test and train data set to minimize the out-of-bag error rate (
14). A forest of 85 trees was constructed, with a minimum of nine variables tried at each node. The random forest was optimized on the number of variables examined at each node and the number of trees grown, with seed set at 150 for replicability and comparison across parameters. The package “forestFloor” (
15) was used to extract the partial dependence of each variable after assembly of the final model. Significant differences between enrollment groups and nominal variables were examined with Fisher’s exact test, and differences in continuous variables were compared with one another with the Wilcoxon signed rank test. Mantelhaen tests were used to examine interaction effects between enrollment status, race-ethnicity, and other individual-level and socioenvironmental factors. Significant differences among ethnic groups, enrollment status, and other variables are described as ORs or difference of medians (MdD). All analyses were conducted with RStudio for Mac, version 1.1.423 (
16).
Results
Objective 1
Table 1 summarizes the associations of individual-level demographic variables and socioenvironmental factors with race-ethnicity among all individuals referred to the Early CSC program and by subgroup. Among those referred, 41% were Hispanic, 37% were non-Hispanic White, and 22% were from other minority groups.
Table 2 presents ORs, MdDs, and 95% CIs for associations among all referrals. Secondary analyses indicated that Hispanics were significantly more likely than non-Hispanic Whites to be referred by inpatient or outpatient mental health providers and not by other referral sources (OR=0.30, p=0.004). Hispanics were significantly more likely than non-Hispanic Whites to have Medicaid (OR=3.29, p<0.001) and less likely to use commercial insurance (OR=0.31, p<0.001). Compared with non-Hispanic Whites, Hispanics were also significantly more likely to live in areas with lower rates of high school education (MdD=−4.70, p<0.001), higher rates of poverty (MdD=5.60, p=0.003), lower rates of speaking English (MdD=−1.61, p=0.009), higher diversity (MdD=3.10, p=0.002), lower median home values (MdD=−10.76, p=0.001), and higher per capita income growth (MdD=0.29, p=0.001). Hispanics, compared with non-Hispanic Whites, lived in areas with greater unemployment (MdD=2.00). Compared with individuals from other minority groups, non-Hispanic Whites were less likely to live in areas with greater unemployment (MdD=–2.00, p=0.016). Additionally, Hispanics lived in areas with higher rates of speaking Spanish, compared with non-Hispanic Whites and persons from other minority groups (MdD=7.41, p=0.012 and MdD=0.02, p=0.001, respectively).
Among the 58 individuals who were not eligible for program enrollment, reasons for ineligibility included attenuated symptoms of psychosis not meeting the threshold for FEP (N=14, 24%), no symptoms of psychosis (N=6, 10%), psychosis secondary to another disorder or illness (N=13, 22%), onset of psychosis greater than 1 year ago (N=20, 35%), or another reason (N=5, 9%). No significant differences in reasons for ineligibility were found by race-ethnicity.
Of the 47 individuals who were eligible and who did not enroll, 19 (40%) were lost to follow-up, seven (15%) declined participation, 13 (28%) chose to receive services elsewhere, and eight (17%) did not enroll for some other reason. No significant differences in reasons for not enrolling were found by race-ethnicity.
Table 3 summarizes the bivariate associations of individual-level variables and socioenvironmental factors with race-ethnicity among eligible referrals who enrolled in the Early CSC program (N=75). Of those enrolled, 52% were Hispanic, 35% were non-Hispanic White, and 13% were from other minority groups. Among those enrolled, 61% reported using substances. Nonaffective psychosis was the diagnosis for 46%, 27% were diagnosed as having affective psychosis, and 27% were diagnosed as having unspecified psychosis. Hispanics enrolled in the Early CSC program were significantly more likely than non-Hispanic Whites to have Medicaid (p=0.002).
In addition, secondary pairwise analyses indicated that compared with non-Hispanic White enrollees, Hispanic enrollees were significantly more likely to live in areas with lower rates of high school education (p=0.001), greater unemployment (p=0.005), lower rates of speaking English (p=0.007), higher rates of speaking Spanish (p=0.01), higher rates of diversity (p=0.01), and lower per capita income growth (p=0.001).
Objective 2
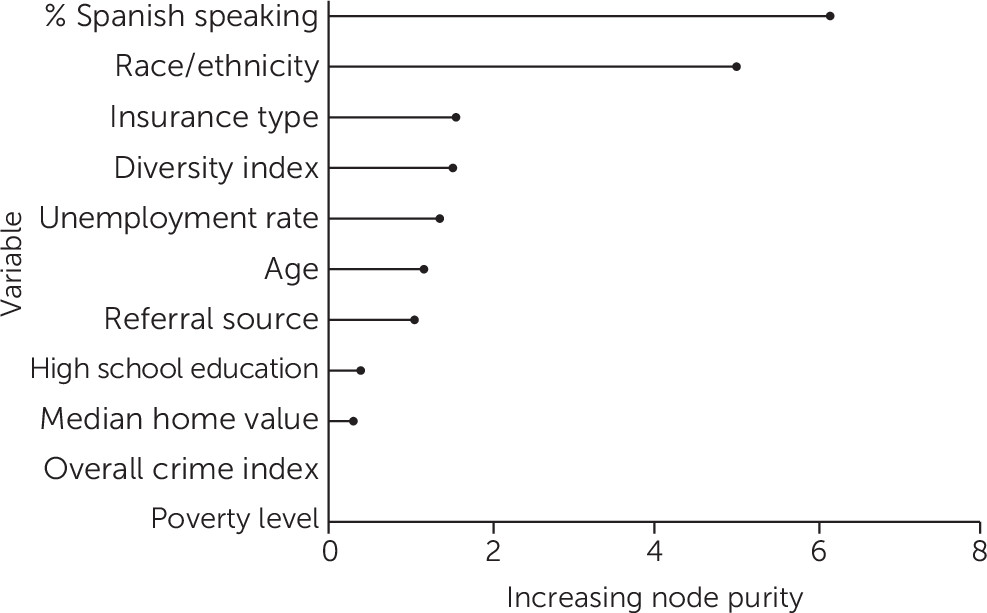
Of the 114 individuals who were determined to be eligible, 74 enrolled and 40 did not enroll. The final random forest model correctly classified 72% of individuals, with higher accuracy of classification among those enrolled (N=64, 87%), compared with those not enrolled (N=18, 45%). In the overall model, the following variables most accurately classified enrollment status: percentage Spanish speaking, race-ethnicity, and insurance type (
Figure 1). This was measured by the mean decrease in accuracy of the model when a given variable was excluded. The least important variables in classifying enrollment were median home value, poverty level, and overall crime index.
Compared with eligible individuals from other minority groups, eligible Hispanics were more likely to enroll (OR=4.97, 95% CI=1.82–13.55, p=0.001), as were eligible non-Hispanic Whites (OR=4.42, 95% CI=1.52–12.87, p=0.006). Eligible individuals were significantly more likely to enroll if they were living in areas with a lower prevalence of Spanish speaking (MdD=−0.05, 95% CI=−0.12, −0.03, p=0.04). Lower prevalence of Spanish speaking was defined as 30% or less of the community speaking Spanish, and it was determined by the median split value used in classifying enrollment status, among all trees in the random forest model.
Significant interactions between race-ethnicity and socioenvironmental factors emerged in classifying enrollment. Compared with individuals from other minority groups, Hispanics were 2.4 times more likely to enroll if they were living in areas with a lower prevalence of Spanish speaking (95% CI=1.07–8.34, p=0.025).
Discussion
To our knowledge, this is the first study to examine demographic, clinical, and socioenvironmental characteristics among Hispanics, compared with other racial-ethnic groups, referred to and enrolled in CSC and to explore whether these factors are associated with enrollment in services among eligible referrals.
Objective 1
Compared with non-Hispanic Whites, Hispanic youths were less likely to be referred to the Early CSC program by nonmental health providers, including family or community members. Hispanic youths were also more likely than non-Hispanic Whites and individuals from other minority groups to live in areas with a higher prevalence of Spanish-speaking individuals. These findings suggest the need for improving pathways to care for Hispanic youths experiencing FEP by targeting Spanish-speaking communities. Research suggests that public health campaigns specifically targeting Spanish-speaking communities increase psychosis literacy among family members (
17–
19). This could improve referral pathways, because Hispanics with serious mental illness often live with their families (
18). Future research would need to include more information regarding the number and type of contacts with mental health services or other community services prior to engagement with specialized services. In addition, as the only FEP program in New Mexico, the Early CSC program would need to have enough staff not only to provide the community outreach but also to field and screen any resulting referrals. Depending on the appropriateness of the referrals, the program would also need to have the capacity to accept more clients.
Significant differences were found between Hispanics and other groups referred to the Early CSC program in regard to demographic, clinical, and socioenvironmental factors. Compared with non-Hispanic White referrals, Hispanic referrals were significantly more likely to be insured by Medicaid; furthermore, Hispanic referrals were more likely to live in disadvantaged, diverse areas, compared with non-Hispanic White referrals and referrals from other minority groups. In addition, the data suggest that Hispanics were underrepresented among referrals to the program (41% of referrals were Hispanic, compared with 49% of the population) but that Hispanics were overrepresented among enrollees (52%). It is possible that the higher rates of enrollment among Hispanic referrals was related to higher acuity, because this population was more likely to be referred by mental health providers and less likely to be referred by other sources. However, this study was unable to examine this effect, because the medical records did not include symptom rating scales at intake that could be extracted for analysis.
Objective 2
The main predictors of enrollment in the Early CSC program were Hispanic and non-Hispanic White racial-ethnic status. The finding of interest lies within the interactions found regarding race-ethnicity and socioenvironmental factors, particularly percentage Spanish speaking. Even though eligible Hispanic clients were from communities with higher rates of speaking Spanish, living in an area with a lower rate of Spanish speaking was a factor significantly associated with enrollment among Hispanics. Further work is needed to explore the pathways to care for individuals in areas where Spanish is commonly spoken and how primary language affects enrollment rates for various race-ethnicity groups.
Retrospective reviews are useful exploratory studies to direct subsequent prospective investigation (
20,
21). We followed best practices in conducting a retrospective review to increase the scientific validity of our findings, including operationalization of all variables and standardized abstraction. Another strength of the study was the use of the random forest model, which is able to maintain power with relatively small samples, eliminate the need to create explicit interaction variables by examining variables sequentially, and handle unbalanced data (
22). Findings related to the communities in which Hispanics were more likely to live (based on publicly available databases) must be interpreted with caution, because observations at the aggregate level may not apply at the individual level (
23).
Conclusions
Hispanics are currently about 18% of the U.S. population (
24), and the proportion is expected to grow to 30% by the year 2060 (
25). More research is needed to inform CSC program development and outreach in New Mexico and other regions with growing Hispanic populations. The Early CSC program at the University of New Mexico has a larger proportion of Hispanic FEP clients, compared with most CSC programs in the United States, providing a unique research opportunity. A more rigorous study design utilizing the population of Early CSC program clients and documenting pathways to care and outcome data will add to the knowledge base.