An emerging body of evidence suggests that stressors caused by the COVID-19 pandemic are adversely affecting the mental health of many youths in the United States (
1–
7). For example, the proportion of emergency department visits for mental health issues nationally was 31% higher among youths ages 12–17 between March and October 2020, compared with the same prepandemic period in 2019 (
1). A nationally representative survey of parents fielded in June 2020 found that 14% reported that their children’s mental health had worsened during the pandemic (
3), and a large survey of caregivers in Chicago found similar results (
2). The mental health impacts of the pandemic could be especially severe for youths served by public mental health agencies.
As Pinals and colleagues (
8) have described, “State behavioral health directors have faced inordinate challenges in facilitating responsive approaches to the COVID-19 crisis.” Furthermore, as Goldman and colleagues (
9) noted, mental health agencies are particularly vulnerable to service disruptions caused by the pandemic because they are typically underfunded. These concerns were echoed in a U.S. Government Accountability Office Report, which found evidence that public mental health agencies encountered challenges to meeting service demands during the pandemic (
10). These agencies also disproportionately serve youths from low-income families (
11) and are thus more likely to encounter technological barriers to telepsychiatry services (
12). As such, the impacts of the pandemic on mental health agencies could contribute to pandemic-related mental health disparities between socially disadvantaged and advantaged youths (
13)—similar to disparities observed among U.S. adults during the pandemic (
14–
19).
The impacts of the pandemic on mental health agencies and safety net services for youths have received little attention from scholars and virtually no empirical research has been conducted in this area. The aforementioned reviews by Pinals and colleagues (
8) and Goldman and colleagues (
9) did not address youth-specific issues. Surveys have assessed psychologists’ perceptions of the impacts of the COVID-19 pandemic on service delivery (
20–
23); however, this work has largely been limited to adult-serving direct-service providers in private practice. An international survey of 681 mental health professionals found that 59% identified the impact of the pandemic on prevention and treatment of mental health conditions among youths and on youth service systems as a top research priority (
24). However, data about these impacts and the challenges that mental health agencies have faced in providing youth services during the pandemic are lacking.
We conducted a national survey of public mental health agency officials. The study aims were to describe the extent to which these officials perceive youth mental health issues as being negatively affected by the COVID-19 pandemic; characterize the extent to which these officials perceive issues as challenges to providing mental health services to youths during the pandemic, including issues related to telepsychiatry services, across patient, provider, and financing domains; and explore associations between perceptions of challenges to providing mental health services to youths during the pandemic and perceived impacts of the pandemic.
Methods
The study was approved by the Drexel University Institutional Review Board. Between September 21 and October 30, 2020, Web-based surveys were sent to 695 U.S. state and county mental health agency officials. These individuals were identified at the state level for all 50 states and also at the county level for 15 states that have decentralized mental health systems (a table in an
online supplement to this article presents additional details).
The survey was created and distributed using Qualtrics, a Web-based survey tool. The sample frame included agency officials in roles such as director, deputy director, children’s division director, medical director, and Substance Abuse and Mental Health Services Administration program director. Each agency official was sent a personalized e-mail with a unique survey link six times, and telephone follow-up was conducted to ensure that e-mails were received.
The survey was completed by 159 respondents, 62% from state agencies and 38% from county agencies. The aggregate response rate was 23%, which is considered good for agency officials (
25) and notably higher than response rates for national surveys of psychologists during the pandemic (
21–
23). Nonresponse analysis indicated that there were no statistically significant differences in response rate by U.S. Census region. At least one survey was completed in 46 states (92% of states responding; median of two respondents per state). Among respondents, 30% (N=48) were from the Northeast, 26% (N=41) were from the South, 25% (N=40) were from the Midwest, and 19% (N=30) were from the West. We used Gender API, a marketing tool that uses a person’s first name to predict the probability of their identifying as female or male, to assess gender differences between respondents and nonrespondents. We found no significant difference in the percentage of respondents and nonrespondents who had a first name that was predicted to be female (73% versus 68%) or the average prediction probability accuracy between the two groups (98% versus 98%).
Variables
The survey focused on two domains of variables: impacts of the COVID-19 pandemic on issues related to youth mental health and challenges to providing mental health services to youths during the pandemic. The selection of variables and development of survey items to assess them was informed by practice reports about these pandemic-related issues, such as those published in the trade publication
Mental Health Weekly, and general literature about barriers to providing telepsychiatry services (
26,
27). The survey items (see
online supplement) were reviewed by five former mental health agency officials to assess the clarity of questions. The order of items in each domain was randomized to reduce the risk of order-effect bias (
28).
Impacts of the COVID-19 pandemic on six issues were assessed, each on a 7-point Likert scale (1, no effect; 7, major negative impact). Challenges to providing mental health services to youths during the COVID-19 pandemic were assessed through two sets of items: one focused on general challenges and one focused on telepsychiatry challenges. Each challenge item was assessed on a 7-point Likert scale (1, not a challenge; 7, major challenge). Challenges specifically related to telepsychiatry services were separately assessed across patient, provider, and financing domains. Five patient challenges were assessed and summed to create a composite patient telepsychiatry challenge score (Cronbach’s α=0.85), eight provider challenges were assessed and summed to create a composite provider telepsychiatry challenge score (Cronbach’s α=0.91), and four financing challenges were assessed and summed to create a composite telepsychiatry financing challenge score (Cronbach’s α=0.93). A composite telepsychiatry challenge score was not calculated for a respondent if the person did not respond to one or more items in the domain. Demographic characteristics related to respondents’ highest level of education, the number of years they had worked at their agency, race-ethnicity, and gender were assessed.
Analysis
Means and standard deviations were calculated for all items and composite scores. Descriptive statistics were also generated, with each 7-point Likert scale item dichotomized: responses of 6 or 7 were coded as “serious impact” or “serious challenge.” For each domain of telepsychiatry challenge (i.e., patient, provider, and financing), the mean of the mean rating for all items was calculated for each respondent. Paired-sample two-tailed t tests assessed the significance of differences in these means as well as the means of individual items. Chi-square tests were used to compare proportions. Missing data (i.e., item nonresponse) were excluded from analyses and ranged from 5% to 17% (mean=11%, median=9%).
Multiple linear regression models estimated associations between perceived challenges to providing youth mental health service during the pandemic and perceived impacts of the pandemic on youth mental health issues. Five models were run, with ratings of mental health impacts as dependent variables in separate models. We limited the variables in these analyses to instances in which there was a plausible rationale for why a challenge variable might affect an impact variable. Every model adjusted for all seven general challenges and the three telepsychiatry challenge composite scores. Variables related to demographic characteristics, geographic region, and state or county agency level were not included in the models because analyses of variance and chi-square tests revealed that they were not significantly associated with perceptions of challenges or impacts. A p value of 0.01 was used as the threshold for statistical significance in the models to reduce the risk of type 1 error. Assessment of multicollinearity showed that the variance inflation factor was between 1.0 and 4.0 for all independent variables in all models, indicating the absence of multicollinearity (
29). Assessment of the normality of the data revealed that the majority of variables were skewed at a threshold ≥0.20. Thus all variables were log transformed when entered into the regression models.
Results
Nearly half of respondents (N=78, 49%) had worked at their agency for ≥10 years, and the modal highest level of education was master’s degree (N=111, 70%) followed by a doctoral degree (N=30, 19%). Respondents predominantly identified as female (N=122, 77%) and non-Hispanic White (N=49, 73%).
Impacts of the Pandemic on Youth Mental Health Issues
The issue perceived as most serious was the disproportionately negative impacts of the COVID-19 pandemic on the mental health of socially disadvantaged youths (serious impact, 72%; mean rating=5.85) (Table
1). Issues related to the negative impacts of the pandemic on youth mental health in general (serious impact, 53%; mean=5.48) and the increasing demand for youth mental health services (serious impact, 46%; mean=5.16) were perceived as the second and third most serious issues. The differences in mean impact ratings between these three issues were all significant at a threshold of p≤0.003. The vast majority of respondents did not perceive the pandemic as having seriously negative impacts on receipt of needed youth mental health services (serious impact, 15%; mean=4.29), the quality of youth mental services (serious impact, 12%; mean=3.88), or the supply of youth mental health services (serious impact, 15%; mean=3.76).
Challenges to Providing Youth Mental Health Services During the Pandemic
General service challenges.
The general service challenge perceived as most serious was the inability to provide some youths mental health services remotely during the pandemic (e.g., home- and community-based programs and mobile crisis services) (serious challenge, 42%; mean=4.72) (Table
2). Provider staffing issues related to illness and child care obligations were perceived as the second most serious challenge (serious challenge, 29%; mean=4.25). Only 11% or less of respondents indicated that facility closures (mean=2.98), redeployment of inpatient psychiatric beds for COVID-19 patients (mean=2.60), or medication supply (mean=2.29) was a serious challenge to providing youth mental health services.
Telepsychiatry service challenges.
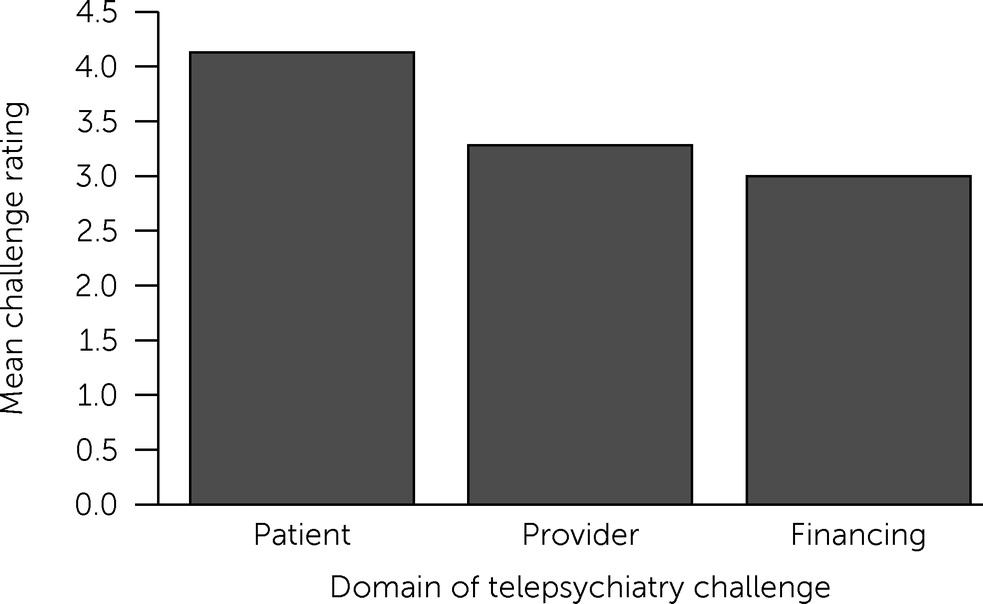
The telepsychiatry service challenges perceived as most serious were in the patient domain (Figure
1). The mean±SD rating of challenges in this domain (mean=4.13±1.35) was significantly higher—24% higher—than the mean rating of challenges in provider domain (mean=3.26±1.42) and 32% higher than challenges in the financing domain (mean=3.01±1.64).
Two specific telepsychiatry challenges, both in the patient domain, were perceived as much more serious challenges than others (Table
3). These challenges were the lack of reliable Internet access for patients, lack of data on cell phone plans, or lack of equipment (i.e., laptops or tablets) (serious challenge, 59%; mean=5.47) and the fact that telepsychiatry services are not developmentally appropriate for some youths (e.g., children of certain ages and children who are nonverbal) (serious challenge, 41%; mean=4.81). The most serious challenges in the telepsychiatry provider domain were lack of provider training on telepsychiatry (serious challenge, 18%; mean=3.71) and the fact that some types of therapies offered do not translate to telepsychiatry (serious challenge, 17%; mean=3.68). The most serious challenge in the telepsychiatry financing domain was insufficient commercial insurance reimbursement for telepsychiatry services (serious challenge, 15%; mean=3.40).
Associations Between Challenges to Providing Youth Mental Health Services and Impacts
The extent to which the inability to provide some services remotely was perceived as a challenge was positively and significantly associated with the extent to which three of the five youth mental health issues were perceived as being adversely affected by the COVID-19 pandemic (Table
4). For example, a 1% increase in the extent to which the inability to provide some services remotely was perceived as a challenge was associated with a 0.28% increase in the extent to which the pandemic was perceived as having disproportionately negative mental health impacts on socially disadvantaged youths (β=0.28, p=0.01, model 1) and a 0.39% increase in the extent which the pandemic was perceived as adversely affecting the quality of mental health services for youths (β=0.39, p<0.001, model 4). None of the telepsychiatry challenge composite scores were significantly associated with the impact variables in the adjusted models.
Discussion
This survey was the first national assessment of the impacts of the COVID-19 pandemic on safety net youth services provided by mental health agencies. We find that officials in these agencies perceived the pandemic as having seriously adverse impacts on youth mental health, particularly among socially disadvantaged youths. However, most did not perceive the pandemic as dramatically preventing access to needed services. The primary challenges to service provision were related to the inability to provide some services remotely, patients lack of sufficient technology (e.g., Internet access) for telepsychiatry services, and telepsychiatry services not being developmentally appropriate for some youths.
The finding that the COVID-19 pandemic was perceived as having disproportionately negative impacts on the mental health of socially disadvantaged youths is consistent with research about the impacts of the pandemic on adults. Surveys have indicated that U.S. adults who are financially insecure, African American, or Hispanic have experienced elevated levels of stress and psychiatric morbidity because of the pandemic (
14–
19). Disparities in pandemic-related stress and psychiatric morbidity among adults could adversely disrupt household dynamics and subsequently contribute to disparities in pandemic-related mental health problems among youths (
13,
30). A key question for future research and practice is how public mental health agencies can best engage socially disadvantaged youths in care. One approach might be social marketing campaigns that reduce mental illness stigma among youths and caregivers and improve attitudes about mental health services (
31). Research among U.S. adults indicates that such attitudinal barriers are major impediments to mental health treatment among persons with psychiatric disorders from racial and ethnic minority groups (
32).
The finding that the COVID-19 pandemic was not perceived as dramatically preventing access to youth services in public mental health systems likely reflects rapid systemwide transitions to telepsychiatry. Recent studies have indicated that mental health providers successfully transitioned to telepsychiatry during the pandemic (
20–
23,
33,
34). Our finding that mental health agency officials did not perceive provider issues as major challenges to youth telepsychiatry services is consistent with this literature.
However, agency officials in our survey perceived patient issues related to lack of reliable Internet access, lack of data on cellphone plans, and lack of equipment as major barriers to youths’ access to telepsychiatry services during the COVID-19 pandemic. These issues could contribute to disparities in the pandemic’s mental health impacts, because such technological challenges are disproportionately prevalent among socially disadvantaged groups (
35). For example, data from the Pew Research Center indicate that only 56% of adults with annual household income <$30,000 have broadband Internet in their home, and 71% have a smartphone, compared with 81% and 85%, respectively, of adults with household incomes of $30,000–$99,999 (
12).
The results of exploratory regression models highlight areas for future research. One area is related to the challenge of mental health agencies’ inability to provide some services remotely. This challenge was significantly and positively associated with the extent to which the pandemic was perceived as adversely affecting three of the five youth mental health impacts assessed. Counterintuitively, this challenge was not significantly associated with the extent to which the pandemic was perceived as preventing youths from receiving needed mental health services. This could be because services that cannot be offered remotely—the examples provided in the survey were “home-based and community-based programs, mobile crisis, respite for caregivers”—might constitute a small proportion of youth mental health services offered by agencies. It should also be noted that none of the challenges assessed were significantly associated with perceptions of the pandemic’s preventing youths from receiving needed mental health services, and none of the models significantly explained any of its variance. Future research using administrative data sets is needed to understand the impacts of the pandemic on youth mental health service utilization in safety net settings.
Our survey had at least five main limitations. First, although 92% of states had at least one respondent, and nonresponse analysis revealed no statistically significant differences in the response rate by U.S. Census region or gender, it is possible that survey respondents were not fully representative of all youth-serving mental health agency officials. As noted, our response rate was higher than rates in two national surveys of mental health service providers fielded during the pandemic, which achieved response rates of 11.8% (
21) and 13.6% (
22,
23).
Second, the survey covered a wide range of topics and, with the exception of challenges related to telepsychiatry services, assessed constructs with single Likert scale items. Third, the regression analyses were exploratory and not hypothesis driven. The models may have been statistically underpowered to identify all significant associations. Fourth, it should be noted that agency officials did not respond to some items—for each item, about 10% of officials did not respond. It is likely that respondents did not respond to these items because they did not have an opinion about the issue, but the reasons are unknown. Fifth, it should be emphasized that the survey focused on the perceptions of agency officials and may not reflect the perceptions of other important stakeholders, such as patients and providers. Many challenges—such as youth privacy concerns related to telepsychiatry encounters—may be formidable but not reflected in the survey findings because information about these challenges did not reach agency officials. There would be value in future research that assesses the extent to which agency officials’ perspectives are aligned with objective measures of barriers to treatment, such as those available in health care claims databases.
Conclusions
Mental health agency officials perceived the COVID-19 pandemic as having serious and disproportionately negative impacts on the mental health of socially disadvantaged youths; however, they did not perceive it as dramatically preventing access to youth mental health services. The inability to provide some types of youth mental health services remotely during the pandemic was perceived as a major challenge by many agency officials, as were patient-related challenges to telepsychiatry services for youths. However, telepsychiatry provider and financing issues were generally not perceived as major challenges. The survey findings provide an empirical foundation to inform future research and financing, policy, and programming initiatives to support mental health agencies in their efforts to address the mental health consequences of the COVID-19 pandemic among youths.