One in five adults experiences mental illness each year, and among these individuals, one-quarter experience serious mental illness (
1). Serious mental illness has affected an increasing number of adults in the United States, from 9.8 million in 2014 to 14.2 million in 2020 (
1). The overall prevalence of serious mental illness is estimated to be similar across rural and urban adult residents, with rates increasing from 3.8% in 2010 to 5.0% in 2020 in large metropolitan or urban counties and from 4.6% to 5.7% in nonmetropolitan or rural counties during the same period (
2). Inpatient psychiatric facilities serve as essential sources of care for individuals with serious mental illness. Among all adults with serious mental illness, an estimated 929,000 (6.5%) received inpatient treatment in 2020 (
3). Given that nearly 95% of rural counties have mental health professional shortage areas (MHPSAs) (
4,
5), the quality of the care that is available in these regions is particularly important. However, little is known about the quality of inpatient psychiatric care in rural and urban hospitals in the United States.
Patients hospitalized in psychiatric units often have complex conditions that require continual engagement with health care providers (
6). However, rural residents face provider shortages at a far greater rate than do urban residents. Across all rural counties, 65% lacked a psychiatrist in 2015, compared with 27% of urban counties (
4). Assessing the total mental health workforce, the Health Resources and Services Administration has identified 3,916 (of 6,464; 60.6%) MHPSAs in rural America (
5). As of September 2022, about 37 million rural residents lived in MHPSA communities, and 7,871 mental health practitioners are needed to remedy these shortages (
5).
The limited mental health workforce may make it difficult for rural psychiatric units to meet many patient-related quality improvement metrics (
7,
8). These measures include promoting individuals’ autonomy, independence, and safety by minimizing use of restraint and seclusion; providing appropriate justification for prescribing individuals multiple antipsychotic medications; and offering a transition record to patients and caregivers at discharge (
7). For individuals discharged from inpatient psychiatric facilities, shortages of mental health providers might also hinder their ability to receive early follow-up care, potentially leading to higher rates of suicide attempt and death (
9). Stigma surrounding mental health in small communities may pose an additional barrier, leading many rural patients to bypass their local rural hospital and instead seek care in urban hospitals (
10). Conversely, rural hospitals may have some quality advantages. Urban inpatient psychiatric units may face difficulties providing evidence-based continuity of care to rural patients because such units would need to make additional efforts to connect rural patients to outpatient care, whereas rural units discharging patients to proximal rural settings may more readily identify and work directly with local providers for transition planning and record transmission (
11). Indeed, one study found that rural residents were more likely to be admitted to high-quality facilities than were urban residents (
12).
Recognizing differences in quality of care among inpatient psychiatric care providers, the Patient Protection and Affordable Care Act required the development of metrics for care quality in mental health services. These metrics were developed by the Centers for Medicare and Medicaid Services (CMS) and were implemented in 2012 (
13). Data from the Inpatient Psychiatric Facility Quality Reporting (IPFQR) program assess quality of care within inpatient units across multiple dimensions; these data have been publicly available since 2015. Since the IPFQR implementation, studies have noted improvements in quality of care associated with IPFQR (
14,
15). However, studies of rural facilities have been sparse. One study found variation in rates of 30-day readmission across hospitals in metropolitan (20.3%), rural micropolitan (19.7%), and other rural counties (20.4%) (
16); however, that study did not focus on rurality and did not consider care coordination and patient safety performance across inpatient psychiatric facilities. In this study, we aimed to provide an overview of the quality of inpatient psychiatric care in rural and urban hospitals.
Methods
Data Sources
This retrospective study included both cross-sectional and longitudinal analyses of data from the publicly available 2015–2019 IPFQR program data sets (
13,
17). Under this program, inpatient psychiatric facilities must report their performance on a set of structure- and process-related quality measures or face a two-percentage-point penalty to their Medicare standard federal rate for that year (
13). All facilities with inpatient psychiatric services furnished by Medicare and classified as psychiatric hospitals or distinct psychiatric units in acute care or critical access hospitals are subject to the IPFQR program requirements (
13). The CMS measures inpatient psychiatric quality across the domains of continuity of care, patient experience, readmission, and substance use screening and treatment as part of the National Quality Strategy (
18). Values for measures are calculated by using Medicare claims and clinical notes data.
We linked IPFQR data to information from the 2015–2019 American Hospital Association Annual Surveys for hospital characteristics (
19) and to the 2015–2019 American Community Survey zip code tabulation area (ZCTA)–level 5-year estimates of community characteristics for the community in which a facility was located (
20).
Institutional review board approval was waived because the analyses were based on publicly available data. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (or STROBE) reporting guidelines.
Measures
Rurality was measured at the ZCTA level and was categorized into three groups on the basis of rural-urban commuting area (RUCA) codes: urban (primary RUCA codes, 1–3), large rural (4–6), and small or isolated rural communities (7–10). This study included 1,254 unique urban hospitals, 260 unique large rural hospitals, and 130 unique small or isolated rural hospitals, with variations in the number of hospitals across years (see Table S1 in the online supplement to this article).
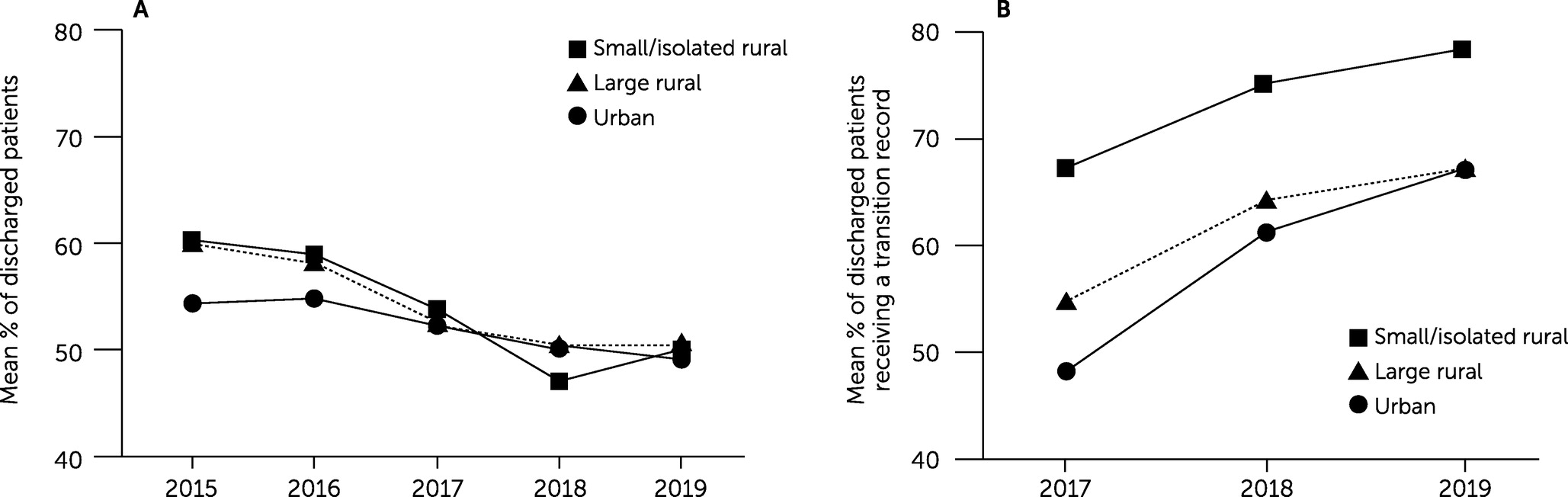
Since 2015, CMS has published and updated annually the facility-specific quality performance metrics used in this study, except for two continuity-of-care measures related to transitions to outpatient care, which were first published in 2017. Continuity-of-care measures included follow-up care, appropriate justification for multiple antipsychotic medications at discharge, and transition record management. CMS quality metrics are calculated across varying populations, as appropriate for each metric. (Descriptions of eligible populations per measure are available in the online supplement.)
For the two patient experience measures, CMS used the number of minutes that psychiatric inpatients in a facility were kept in physical restraint or seclusion and converted this figure to hours. In this study, we categorized whether physical restraint or seclusion was used in each facility each year, because more than half of the facilities had no physical restraint or seclusion events and the variation in hours of physical restraint or seclusion use was driven by urban facilities (see Figure S1 in the online supplement).
Research suggests that for-profit or nonprofit status is associated with changes in use of restraint or seclusion after the IPFQR implementation, and this characteristic was therefore included in our adjusted analyses (
21). Other hospital characteristics included hospital primary services (psychiatric or general medicine and surgery), system affiliation, teaching status, accreditation by the Joint Commission or Det Norske Veritas, critical access hospital status, rural referral center status, number of psychiatric beds, and proportion of registered nurses among all hospitalwide nurses. ZCTA-level metrics included age groups, racial-ethnic composition, and sociodemographic factors (rates of unemployment, uninsurance, households with broadband access, and households <200% of the federal poverty level).
Statistical Analysis
We first used chi-square tests for frequency distributions and one-way analysis of variance tests to compare hospital and ZCTA-level characteristics of facilities located in urban, large rural, and small or isolated rural areas. Descriptive and multivariable regression analyses were used to identify differential trends in quality of inpatient psychiatric care across urban, large rural, and small or isolated rural facilities. In the unadjusted analysis, we used Mann-Kendall trend tests for the continuity-of-care measures, because these tests are operationalized as continuous variables, and used Cochran-Armitage tests to compare trends in proportions over the years of study for use of physical restraint and seclusion. In the multivariable regression analysis, we used generalized linear regressions for the continuity-of-care outcomes and logistic regressions for the patient experience outcomes, both with adjusted standard errors to account for state-level clustering and Bonferroni-corrected p values for multiple comparisons. Models controlled for the aforementioned covariates and included interaction terms between year and hospital rurality to evaluate the annual differential trends in outcomes across urban, large rural, and small or isolated rural facilities. Variance inflation factors (VIFs) were calculated, and no violations of multicollinearity between independent variables were observed (VIF=1.86).
Discussion
To our knowledge, this is the first study to examine differences in the quality of inpatient psychiatric care in rural and urban hospital settings and their changes over time. We found that, at baseline, patients served in rural hospitals had better continuity of care and care experiences than those served in urban hospitals. Continuity of care declined over the study period at all locations, with the exception of management and timely transmission of transition records. The proportion of patients receiving outpatient mental health follow-up care within 7 or 30 days of discharge also declined across all locations. Similarly, appropriate justifications in the discharge record for patients receiving multiple antipsychotic medications decreased across all facilities. Conversely, management of transition records consistently improved in rural and urban facilities over 2017–2019. Rural facilities were less likely to use physical restraints and seclusion than were urban facilities, with no significant annual changes in use.
The higher quality of inpatient psychiatric care in rural facilities is encouraging, given that rural residents had a higher prevalence than urban residents of suicide death after discharge (
22), readmission (
23), and emergency department (ED) visits for mental illness (
24). Previous studies have found that patients who did not receive follow-up care after discharge were six times more likely to be readmitted than those who received follow-up care (
25). Moreover, the risk for suicide has been found to be highest immediately after discharge from psychiatric care and to remain elevated for months thereafter (
9,
26,
27). Follow-up after psychiatric hospitalization is therefore critical to ensure that patients’ transition to communities is supported by outpatient mental health providers to mitigate suicidal ideation, avoidable readmission, and ED visits.
Previous research in the United States has found that patients who were discharged from hospital inpatient psychiatric units made millions of ED visits within 30 days of discharge (
9). A multistate study found that nearly 18% of ED visits or hospital acute care visits were for complications related to a recent psychiatric hospitalization (
28,
29). Ensuring early follow-up care within at least 30 days of discharge is especially important in rural communities, which have shortages of mental health professionals and constraints on acute care capacity (
5). However, in this study, even though rural facilities had a better baseline performance in follow-up care compared with urban facilities, the rural units had a steeper decrease in the proportion of patients receiving follow-up care over the study period. These results suggest a need for systematic quality improvement at the facility level to support all—and particularly rural—facilities’ efforts to ensure early follow-up after psychiatric hospitalization.
Detailed discharge information is necessary to maximize benefits from early follow-up care after hospitalization because it often serves as the primary mode of communication between psychiatric units and outpatient providers (
30). Coordinated transitions from inpatient to outpatient settings, within the same institution or among different organizations, can prevent hospital readmissions, duplication of services, medical errors, and waste of resources. Previous literature has reported that patients participating in a hospital program of providing detailed, personalized instructions at discharge, including a review of medication routines and assistance with arranging follow-up appointments, had 30% fewer subsequent ED visits and hospital readmissions than patients who received usual care at discharge (
31). Of note, this study found that provision and transmission of transition records has progressed across urban and rural facilities, with increases of about 15 percentage points annually, from 53% in 2017 to 83% in 2019. Yet, variations in transition record provision and timely transmission were still prominent in 2019, with the bottom quartile of facilities providing only 47% of their patients with detailed discharge information and transmitting only 31% of their patients’ records in time for a patient’s first postdischarge physician visit. These results raise concerns regarding the substantial deviations in adherence to evidence-based practices in some inpatient psychiatric units, despite nationwide improvements overall.
Rural facilities, especially more isolated facilities, outperformed urban facilities on coordinating postdischarge transition records for their patients. This finding might be due to the proximity of patient residence to the facility, the collaborative nature of small rural communities and organizations, or the data management requirements of the swing bed program in certain rural hospitals. First, compared with rural facilities, urban facilities might serve more nonlocal patients, including a higher proportion of nonlocal patients with serious mental illness, hindering the ability of urban units to provide adequate transition records or to connect rural patients with outpatient care (
10). When discharging rural patients, urban inpatient psychiatric units often must collaborate with distant outpatient care settings, whereas rural units discharging patients to proximal rural settings can more readily identify and work directly with local providers for transition planning and record transmission (
11). Second, rural communities are known for a strong spirit of collaboration—especially in towns where the population is smaller, residents know one another, and mental health care resources are limited—leading to closer networking and collaboration than in urban communities (
32). These connections might facilitate the provision of detailed, personalized discharge records to local patients and families and timely transmission of transition records to other local outpatient providers. Third, since 2002, after passage of the Balanced Budget Act of 1997 (
33), rural hospitals with ≤100 beds have been eligible to participate in the swing bed program—a reimbursement mechanism that covers posthospitalization extended care services. These swing beds are not used for postdischarge psychiatric patients. Still, small rural hospitals with swing beds must document detailed transition records, likely contributing to high performance in transition record coordination for discharged patients across all hospital settings.
Several limitations of this study are worth noting. First, our analysis was solely based on facility-level data and could not be adjusted for the complexity of cases. Important factors that may have affected receipt of follow-up care among patients include, for example, disease acuity, proximity to care, psychotropic medication use, and family functioning and social support. Future studies are warranted to examine patient-level quality of care, especially between rural residents who received and those who did not receive care in local psychiatric units. Second, the follow-up measure uses data only from Medicare fee-for-service claims, and results cannot be generalized to facility performance for patients with other payers, including Medicare Advantage. Third, our findings cannot be generalized to psychiatric units that are not eligible for IPFQR. Finally, using ZCTA-level sociodemographic characteristics and socioeconomic mix as proxies for potential patient mix in a facility might not reflect the actual composition of the patient population.