Although originally developed as anticonvulsant drugs, carbamazepine, valproate, and, more recently, gabapentin and lamotrigine have been used as mood stabilizers in the treatment of bipolar disorder, much as lithium has been used (
1,
2,
3,
4). These agents are used both singly and in combination with one another (
5). Their rates of use relative to one another have changed over the past decade. According to researchers from a Veterans Affairs medical center, from 1989 to 1994 the use of valproate monotherapy came to surpass that of lithium for patients with schizoaffective disorder or bipolar disorder (
6).
After the Food and Drug Administration approved valproate for the treatment of bipolar disorder in 1995, a large increase in its use was observed among patients with bipolar disorder hospitalized in facilities operated by the New York State Office of Mental Health (
7). More than half received valproate in 1996.
The use of mood stabilizers has broadened to cover a wide spectrum of mental disorders besides bipolar disorder. These agents have been used successfully in augmentation strategies with antidepressants (
8) and neuroleptics (
9). Control of impulsiveness and aggressiveness has also been specified as a treatment goal for this group of agents in a variety of diagnoses (
10,
11). In 1993 one-quarter of the inpatient population at a state-operated psychiatric hospital in New York received a mood stabilizer, although less than 20 percent of them had been diagnosed as having bipolar disorder (
12). In that study, a review of the reasons for the prescription of mood stabilizers suggested that the intended effects of the treatment were to improve impulse control and reduce aggressive behavior.
This paper reports on the use of mood stabilizers, and of valproate in particular, among all patients with schizophrenia hospitalized in psychiatric centers operated by the New York State Office of Mental Health. Patients in this population usually are already receiving antipsychotic medication. Very few double-blind, placebo-controlled studies have been conducted on the "off-label" uses of mood stabilizers. Nonetheless, a plethora of retrospective case reviews, open trials, and case reports have served to launch the adjunctive use of mood stabilizers for a variety of conditions, most often agitation and aggressive behavior (
13). With the exception of one open trial (
14), no reports, anecdotal or otherwise, have appeared on the use of the newer mood stabilizers—gabapentin and lamotrigine in particular—for patients with schizophrenia. Because of the large numbers of patients receiving valproate (available as valproic acid or divalproex sodium), the emphasis of this report is on valproate.
Methods
To determine the extent and change over time of the use of valproate and other mood stabilizers among inpatients in the New York State psychiatric hospital system, we used the integrated research database created by the information sciences division of the Nathan S. Kline Institute for Psychiatric Research to obtain data retrospectively. The database contains patient information—such as demographic characteristics; dates of admission, transfer, and discharge; and diagnosis—and drug prescription information for every inpatient in the 19 adult civil facilities (reduced over time to 18 facilities) of the New York State psychiatric hospital system. The prescription information includes drug, dosage, and duration of order. Complete data are available from 1989 on, and partial information is available as far back as the 1960s. The integrated research database has been used previously to examine the extent, pattern of use, and effectiveness of depot neuroleptics (
15,
16) and the use of risperidone (personal communication, Javitt DC, 1999), as well as to compare valproic acid and divalproex sodium (
7).
For each calendar year from 1994 through 1998, all inpatients who received at least one dose of any mood stabilizer as well as those who received no mood stabilizers were identified. Counts of patient episodes of care were obtained for each year by counting discrete admissions.
This study linked prescription orders with current diagnosis. However, a patient's clinical presentation may change over time, and hence the diagnosis of record can change from one admission to the next. Patients diagnosed as having schizophrenia may have been diagnosed at another time as having schizoaffective or bipolar disorder. In tabulating the total numbers of patients per diagnostic category, we considered the diagnosis to be the one recorded most recently for the episode of care. In tabulating numbers of patients in specific medication categories, we used the most recent diagnosis recorded before the patient received the first dose of the medication.
Diagnoses of schizophrenia included those assigned the DSM-IV numerical codes of 295.1x, 295.2x, 295.3x, 295.6x, and 295.9x. Diagnoses of schizoaffective disorders were those coded 295.7x. Diagnoses of bipolar disorder included the codes 296.0x, 296.4x, 296.5x, 296.6x, 296.7x, and 296.8x.
We analyzed the 1998 data in more detail. For patients with a diagnosis of schizophrenia for whom at least one dose of valproate was prescribed or for whom no mood stabilizers at all were prescribed in 1998, further details about age, gender, ethnicity, and length of stay were retrieved from the database. For a subset of patients with a diagnosis of schizophrenia for whom valproate was prescribed for two weeks or more in 1998, we also retrieved information on the dosage and duration of valproate administration, on the proportion of time the drug was administered over the length of stay, and on whether it was coadministered with an antipsychotic medication.
Results
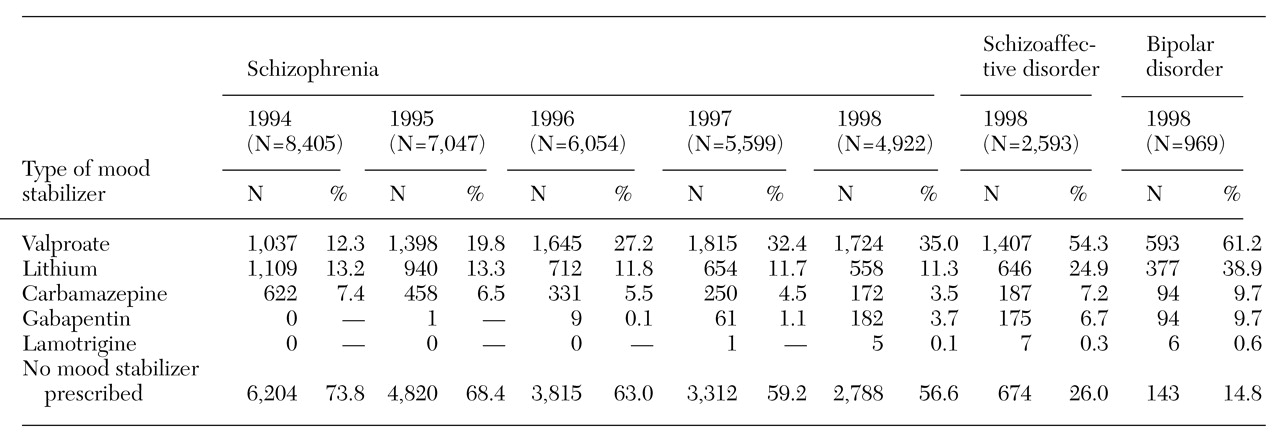
Table 1 summarizes use of valproate and other mood stabilizers from 1994 through 1998 for patients diagnosed as having schizophrenia for whom at least one dose of a mood stabilizer was prescribed in the course of a discrete hospital admission. For comparative purposes, we also included 1998 data on use of mood stabilizers for patients with schizoaffective disorder or bipolar disorder. In 1994 a total of 2,201 of 8,405 inpatients with a diagnosis of schizophrenia (26.2 percent) received a mood stabilizer. Lithium was most commonly prescribed (for 1,109 patients, or 13.2 percent), followed by valproate (for 1,037 patients, or 12.3 percent). In 1998 a total of 2,134 of 4,922 inpatients with a diagnosis of schizophrenia (43.4 percent) received a mood stabilizer, with valproate most commonly prescribed (for 1,724 patients, or 35 percent).
Patients with schizoaffective disorder or bipolar disorder were more likely than patients with schizophrenia to receive a mood stabilizer. The proportion of patients with those disorders who received a mood stabilizer also rose from 1994 to 1998 (earlier data not shown), predominantly as a result of an increase in the use of valproate. For schizophrenia, schizoaffective disorder, and bipolar disorder, a small absolute percentage decrease in use of lithium or carbamazepine was observed. In 1998 gabapentin was prescribed about as often as carbamazepine for patients with schizophrenia, schizoaffective disorder, or bipolar disorder.
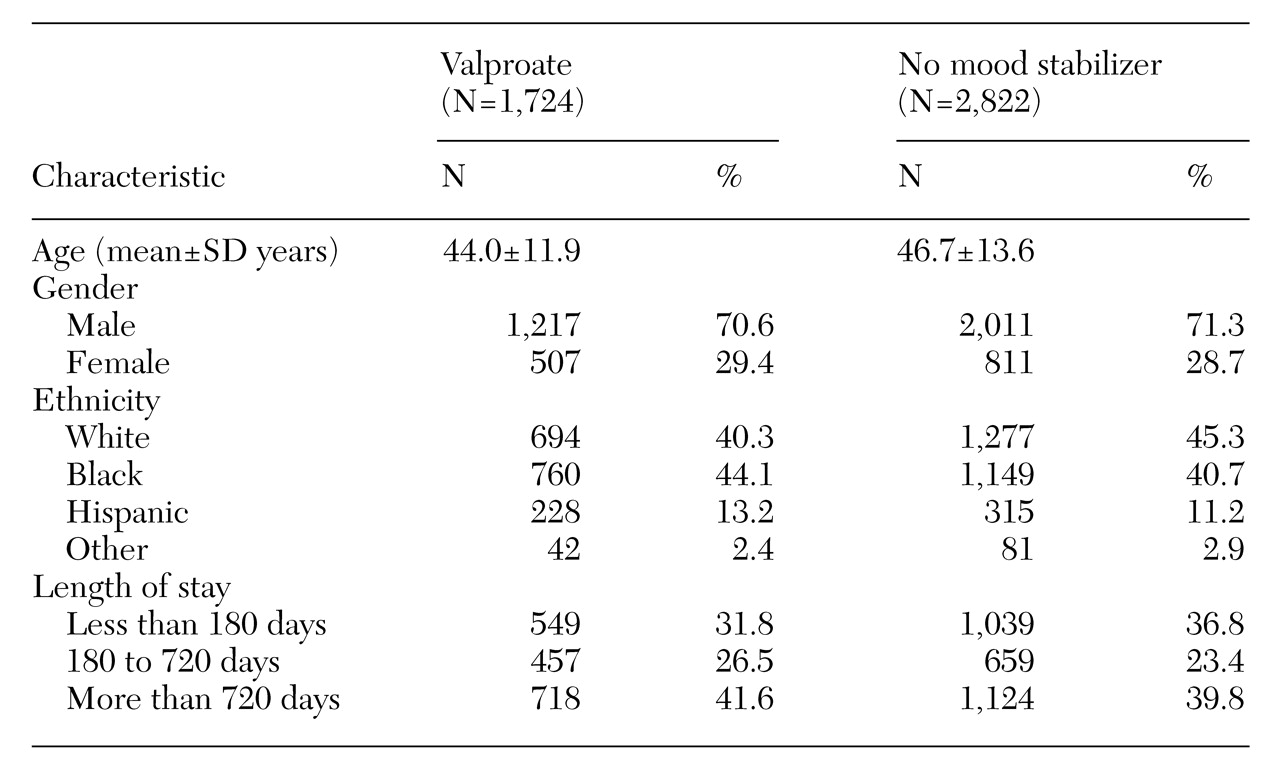
Additional data were retrieved for 1998 on patients with schizophrenia for whom at least one dose of valproate was prescribed and on patients for whom no mood stabilizer was prescribed.
Table 2 summarizes the data on patient age, gender, and ethnicity as well as length of stay for these groups.
In 1998, of 1,724 patients diagnosed as having schizophrenia and receiving valproate, the drug was prescribed for two weeks or more for 1,601 patients (92.9 percent), which constitutes 32.5 percent of all patients diagnosed as having schizophrenia. On average, they received the drug for about 72 percent of their hospital stay at a mean±SD dose of 1,520±655 mg per day; 32.4 percent received valproate for their entire hospital stay.
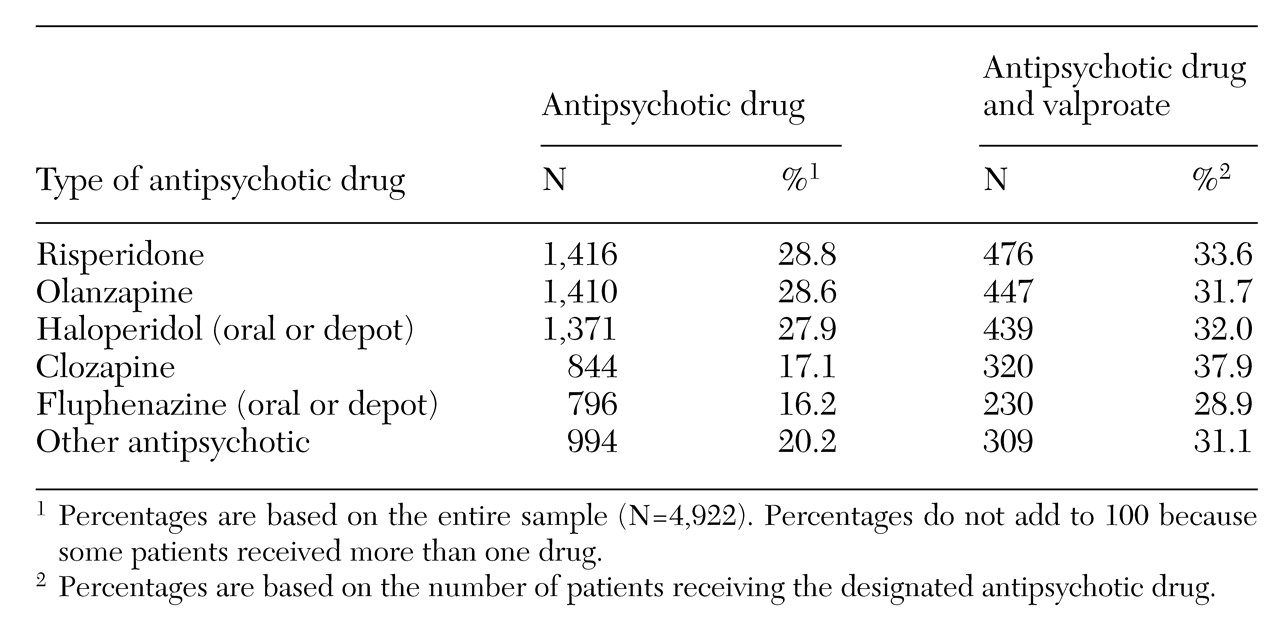
For 95 percent of the patients with schizophrenia who received valproate, an antipsychotic medication was prescribed simultaneously.
Table 3 summarizes coadministration rates for the different antipsychotic medications used with valproate. The rates of valproate use, calculated as a percentage of all patients receiving a given antipsychotic, are in a relatively narrow range, from 28.9 percent to 37.9 percent.
Discussion
The increase in use of mood stabilizers, and valproate in particular, for patients with schizophrenia has paralleled similar increases for patients with schizoaffective disorder or bipolar disorder. For the latter two diagnoses, mood stabilizers have held an established place in the psychopharmacological armamentarium and have been evaluated in a number of controlled clinical trials. Mood stabilizers prescribed for patients with schizophrenia have not received such evaluation.
Only a few reports have described clinical trials of the adjunctive use of valproate for patients with schizophrenia. Wassef and colleagues (
17) counted a total of 130 patients in the eight papers they reviewed in detail. Among the positive studies examining the use of valproate in the treatment of schizophrenia, most were open label (
9,
18,
19,
20,
21,
22,
23,
24), some were double blind (
25,
26), and some also included patients with diagnoses other than schizophrenia (
9,
18,
25). Negative reports have also been published (
27,
28), including one in which valproate was prescribed after antipsychotic medications were stopped (
29).
The adjunctive use of mood stabilizers is widely believed to reduce aggressive and impulsive behavior (
12). Expert consensus guidelines suggest the adjunctive use of mood stabilizers for patients with schizophrenia and "persistent excitement" (
30), but little has been presented in the way of evidence obtained in randomized clinical trials. For lithium, clinical trials have produced negative reports (
31,
32). Carbamazepine has been studied in small trials or in trials that lump together patients with schizophrenia and schizoaffective disorder (
11,
33,
34,
35,
36,
37). Valproate may have antiaggressive effects, but the evidence for its efficacy is based principally on uncontrolled studies and case reports describing mostly patients with dementia, mental retardation, personality disorders, and brain injuries (
18,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48).
The increase in the use of mood stabilizers for patients with schizophrenia may be partly attributable to a changing state hospital population. As the hospital system's census and capacity decline, the patients who remain and the patients who continue to be referred to these tertiary care psychiatric centers may be more treatment resistant and prone to aggressive behavior and therefore more likely to be exposed to novel psychopharmacological approaches. The proportion of patients admitted to these hospitals and diagnosed as having schizophrenia has increased from 39.8 percent of all admissions in 1994 (8,405 of 21,132) to 47.6 percent of all admissions in 1998 (4,922 of 10,335).
The age, gender, ethnicity, and length-of-stay distributions for patients admitted with schizophrenia changed slightly from 1994 to 1998. The number of patients whose length of stay was less than 180 days decreased from 46.4 percent to 33.9 percent; the number of women patients decreased from 33.3 percent to 28.8 percent; the number of white patients decreased from 50 percent to 43.5 percent; and the mean age rose from 44.8 years to 45.8 years. None of these differences explain the observation that the use of valproate has nearly tripled in this population, from 12.3 percent to 35 percent. In absolute terms the number of patients with schizophrenia receiving valproate increased from 1,037 to 1,724, or 66 percent, over the five-year period, despite the decrease in system bed capacity of approximately 50 percent.
With the passage of time, clinicians may become increasingly familiar with mood stabilizers, leading to increased use. It is unlikely that the increase in utilization is attributable to the treatment of a concomitant seizure disorder. In an earlier study of this state hospital population, about 10 percent of all patients receiving valproate in 1996, regardless of psychiatric diagnosis, were reported to have a history of seizure disorder (
7).
An unexpected finding was that in 1998, use of gabapentin exceeded use of carbamazepine for patients with schizophrenia. Gabapentin is an anticonvulsant drug that recently has come into use in the treatment of bipolar disorder (
49), and it has been suggested that it may be useful in the management of behavior dyscontrol (
50). Only one report could be found in the literature describing the use of gabapentin for patients with schizophrenia (
14). The report described an open-label study of 18 patients with anxiety symptoms, ten of whom had been diagnosed as having schizophrenia; 14 experienced clinical improvement.
The population studied here resided in 19 hospitals (reduced to 18 over time) across New York State. The prescriptions counted represent the combined practice patterns of a geographically diverse group of more than 500 psychiatrists. One limitation of this study, however, is that the data cover inpatients only. The rate of use of valproate and other mood stabilizers among patients with schizophrenia being treated as outpatients in clinics operated by New York State psychiatric hospitals is unknown. One report in the literature describes antipsychotic and concomitant medication use among 316 indigent patients with schizophrenia being treated in 1995 as outpatients in an inner-city environment (
51). In that study, 13.3 percent received adjunctive valproate, 10.8 percent lithium, and 3.5 percent carbamazepine. These figures indicate a significant adjunctive use of mood stabilizers, with rates only somewhat lower than those we report for inpatients in 1995: 19.8 percent, 13.3 percent, and 6.5 percent for valproate, lithium, and carbamazepine, respectively (see
Table 1).
The monetary cost of valproate treatment and the attendant costs of obtaining and measuring blood levels are not trivial. The bulk cost of a four-week supply of valproate at 1,500 mg per day is approximately $10.87 for the generic valproic acid, and $98.98 for divalproex sodium (as reported by the pharmacy at the Rockland Psychiatric Center, May 1999). The New York State Medicaid reimbursable cost of a valproate plasma level determination is $10.50, exclusive of venipuncture costs; the full rate is $77.70 (as reported by a local private laboratory in Rockland County, New York State, May 1999). From 1996 data, 430,981 patient-days in which valproic acid was prescribed and 253,185 patient days in which divalproex sodium was prescribed can be counted; the drug cost is at least $1 million during that year for the state-operated psychiatric centers in New York, exclusive of any associated costs for blood monitoring.
Conclusions
From 1994 to 1998, the adjunctive use of valproate has nearly tripled among patients with schizophrenia. Valproate has become the most commonly prescribed mood stabilizer in this population despite the paucity of evidence in the literature that this use is efficacious. Whether prescribing valproate for patients with schizophrenia is good or bad is impossible to determine without outcomes data. Research is lagging behind clinical practice. The results reported here reveal an urgent public health need for controlled clinical trials to test the efficacy of the adjunctive use of mood stabilizers, particularly valproate, for patients with schizophrenia.
Acknowledgments
Maintenance of the integrated research database of the Nathan S. Kline Institute for Psychiatric Research is supported by grants from Eli Lilly & Co. and the Janssen Research Foundation.