Societal stigma significantly impedes the opportunities of persons who have serious mental illnesses such as schizophrenia and bipolar disorder. The 1999 Surgeon General's report (
1) pointed to stigma as a key variable in understanding the course of illness and outcomes of people who have psychiatric disabilities. As we and others have reported elsewhere (
2,
3), the general public is less likely to hire persons who are labeled mentally ill, to lease apartments to them, or to freely interact with them. Moreover, persons who have mental illnesses are less likely to seek mental health services because of the accompanying stigma (
4).
Two constructs are significantly related to the stigma of mental illness: familiarity and social distance. The effects of these constructs can be thought of as anchoring each end of a path describing the impact of stigma: familiarity influences stigma, which in turn influences social distance. Research suggests that members of the general public who are familiar with mental illness—those who have some contact with persons who have psychiatric disabilities—are less likely to endorse stigmatizing attitudes (
5,
6,
7,
8). Conversely, individuals who perpetuate stigma are likely to socially distance themselves from persons with mental illness; social distance may manifest itself in such discriminatory practices as not renting to or hiring people who have psychiatric disabilities (
5,
8,
9,
10). The purpose of this study was to directly test the three components of this path—familiarity, stigma, and social distance.
We have adopted a social psychological model for describing components of stigma that affect the outcomes of persons who have mental illness (
2,
11). According to that model, members of the general public hold stigmatizing attitudes about mental illness and react emotionally as a result of those attitudes—for example, "Persons who have mental illness are dangerous, and I fear them." This emotional reaction leads to a behavioral response—for example, "Because of my fear, I am going to avoid persons with mental illness." This attitude-emotion-behavior model is based on Weiner's (
12) attribution theory, which has been tested in several studies (
13,
14,
15,
16,
17,
18,
19,
20,
21,
22).
As implied in these two examples, a perception of dangerousness is a crucial attitude that affects the components of the stigma model. According to this model, the assumption that an individual has personal responsibility for being violent leads to fear—for example, most people respond to violent threats with apprehension (
23). Several studies have shown a specific relationship between perceiving persons who have mental illness as dangerous and fearing such persons (
7,
9,
24,
25). Fear, in turn, yields avoidant behaviors or social distance.
For example, one study showed that a fearful reaction to two attempts to assassinate politicians, attributed to persons who had schizophrenia, led to greater social distance between the public and individuals with mental illness (
24). This historical finding has been supported by research showing that perceptions of dangerousness lead to social distance from persons with mental illness (
9,
10). Employers do not hire persons who have mental illness, because they want to keep such persons at a distance. Landlords do not permit people with psychiatric disabilities to move onto their properties.
Attitudes about mental illness in general, and dangerousness in particular, are influenced by an individual's familiarity with serious mental illness. Familiarity has been defined as knowledge of and experience with mental illness (
6). It ranges from seeing a television portrayal of mental illness, to having a friend or coworker who has a mental illness, to having a family member who has a mental illness, to having a mental illness oneself. Previous research has shown that a lack of familiarity is associated with prejudicial attitudes about mental illness (
6,
7,
8). We expected members of the general public who were more familiar with mental illness to be less likely to agree that persons who have psychiatric disabilities are dangerous, and we expected this lower perception of dangerousness in turn to be associated with less fear and less social distance.
Within the broader model of familiarity and social distance, we also examined the direct impact of familiarity on fear and social distance. In other words, does familiarity with mental illness directly diminish one's fear of persons who have mental illness as well as social distance from such persons?
Methods
Participants in this study were drawn from the student body of a local community college. We have done previous research with community college students (
5,
26), because they tend to be more demographically representative of the population as a whole than college sophomores from four-year universities. The participants provided demographic information and completed three written measures related to the constructs of familiarity, dangerousness, fear, and social distance.
Familiarity
Previous studies have measured familiarity categorically by asking participants, "Do you know someone with a mental illness?" (
8). However, categorical measures have limited statistical power, so we used the Level of Contact Report (
6), which we had developed previously. The Level of Contact Report lists 12 situations of varying degrees of intimacy that involve persons who have mental illness. These situations were adapted from other scales used in stigma research (
8,
27) and ranged from the least intimacy ("I have never observed a person that I was aware had a serious mental illness") to medium intimacy ("I have worked with a person who had a severe mental illness at my place of employment") to high intimacy ("I have a mental illness").
When the Level of Contact Report was developed, the 12 situations were ranked in terms of intimacy of contact. The mean of rank-order correlations summarizing interrater reliability was .83. The rank order, shown in
Table 1, was validated in a subsequent sample of 100 research participants (
6). The reliability and validity of the measure have been supported by two studies (
5,
6).
The 208 participants in this study were asked to check all of the situations on the 12-item list that they had experienced in their lifetime. The index of familiarity was the rank score of the most intimate situation the participant checked. For example, a participant who checked three situations— "A friend of the family has a serious mental illness" (rank order score, 9), "I have watched a documentary on television about mental illness" (rank order score, 4), and "My job includes providing services to persons with mental illness" (rank order score, 7)—would have a score of 9 because a friend of the family having a serious mental illness is the most intimate of the checked situations.
Perception of dangerousness and fear
A 21-item Attribution Questionnaire (
28), modeled on the work of Reisenzein (
16), was administered to participants. Three questionnaire items each test seven constructs that are relevant to stigma and mental illness: two attitudes—personal responsibility and dangerousness; three emotional reactions—anger, concern, and fear; and two behavioral responses—help and avoidance. An example of an item is, "How frightened of a person with mental illness would you feel?" Participants respond to the items by using a 9-point Likert scale, where 9 indicates "very much." Possible scores thus range from 21 to 189, with higher scores indicating higher levels of perception of dangerousness and fear. The reliability and factor structure for this test were supported by an earlier study (
28). Factor scores corresponding with perceived danger and fear were used.
Social distance
Social distance from persons who have mental illness was assessed with the Social Distance Scale (
8,
27). This scale contains seven items that participants rate on a scale of 0 to 3, where 3 indicates "definitely unwilling." Possible scores thus range from 0 to 21, with higher scores representing a greater desire to distance oneself from persons who have mental illness. An example of an item is, "How would you feel about renting a room in your home to a person with serious mental illness?" The Social Distance Scale has excellent reliability and validity and is often used in stigma research as a proxy for behavioral indexes of discrimination against persons who have mental illness (
6,
8).
Results
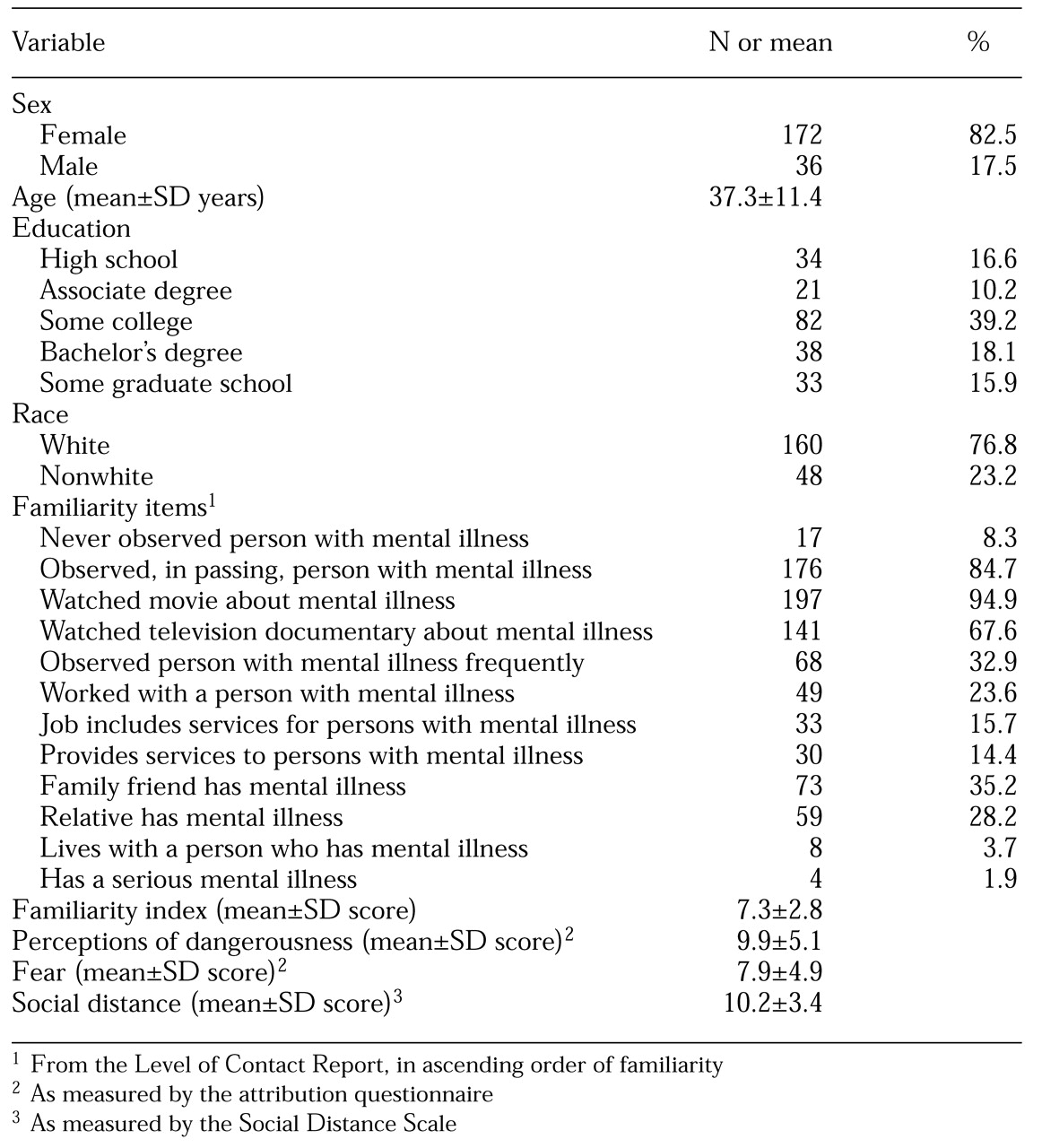
A total of 216 students were informed of the study during their psychology or social science classes and were asked to participate. Of these, 208 agreed to participate and completed all the measures; the other eight students either refused to participate or returned incomplete measures. Demographic data for the participants are shown in
Table 1. A total of 172 participants, or 83 percent, were female, and 160 participants, or 77 percent, were white.
Also shown in
Table 1 are the mean scores and standard deviations for the measures used in the path analysis, along with the frequencies with which the participants checked each of the items on the Level of Contact Report. These frequencies reveal some interesting trends. For example, fewer than 10 percent of the participants reported that they had no experience with mental illness.
This high rate of exposure to persons with mental illness was partly a result of exposure through contemporary media sources. More than 90 percent of the participants had been exposed to images of mental illness in films, and another two-thirds reported seeing more objective presentations of mental illness in documentaries. About a quarter of the participants reported working alongside someone who had a mental illness. A third of the participants had a friend of the family with a mental illness, and a quarter had a relative with a mental illness. Fewer than 5 percent of the participants lived with a person who had mental illness, and only about 2 percent identified themselves as having a serious mental illness.
Path analysis
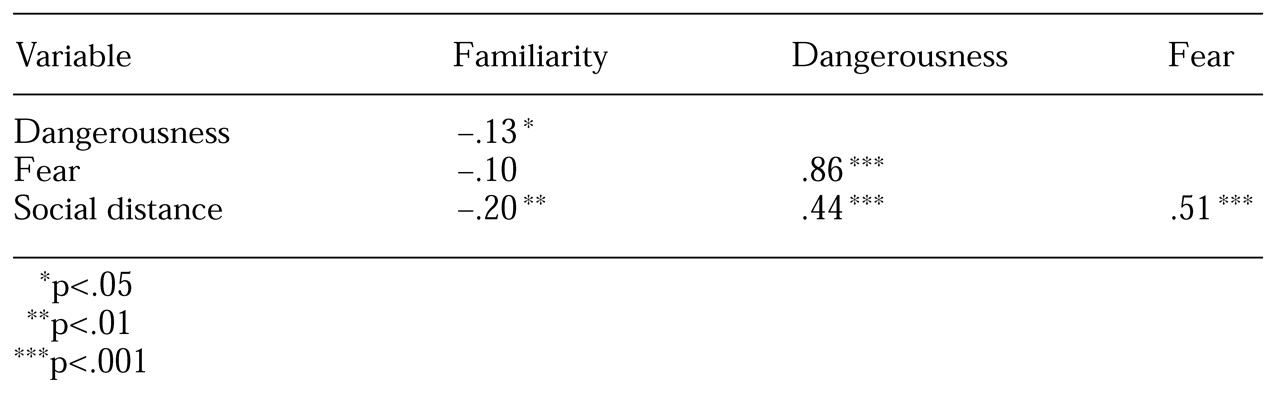
We used path analysis with manifest-variable structural modeling techniques to test our proposed model, because such an analysis examines both the size and the direction of associations among variables. The model was an overidentified recursive model with manifest variables. Intercorrelations among the dependent variables (familiarity, dangerousness, fear, and social distance) are summarized in
Table 2. This intercorrelational matrix was used as the foundation for the remainder of the analyses, which were conducted with use of the SAS system's CALIS procedure. The analyses used the maximum-likelihood method of parameter estimation; all analyses were performed on the variance-covariance matrix (
29).
In terms of goodness of fit, the chi square statistic was used to test the null hypothesis that the reproduced covariance matrix would have the specified model structure—that is, that the model would fit the data. We included two additional goodness-of-fit indexes: the normed fit index (
30) and the comparative fit index (
31). The normed fit index ranges from 0 to 1, where 0 represents the goodness of fit associated with the null model—a model in which all variables are uncorrelated—and 1 represents the goodness of fit associated with a saturated model—a model with 0 degrees of freedom that perfectly reproduces the original covariance matrix. The comparative fit index is a variation on the normed fit index that has been shown to be less biased than the normed fit index in small samples (
31). For each index, a value above .9 suggests an acceptable fit between the model and the data.
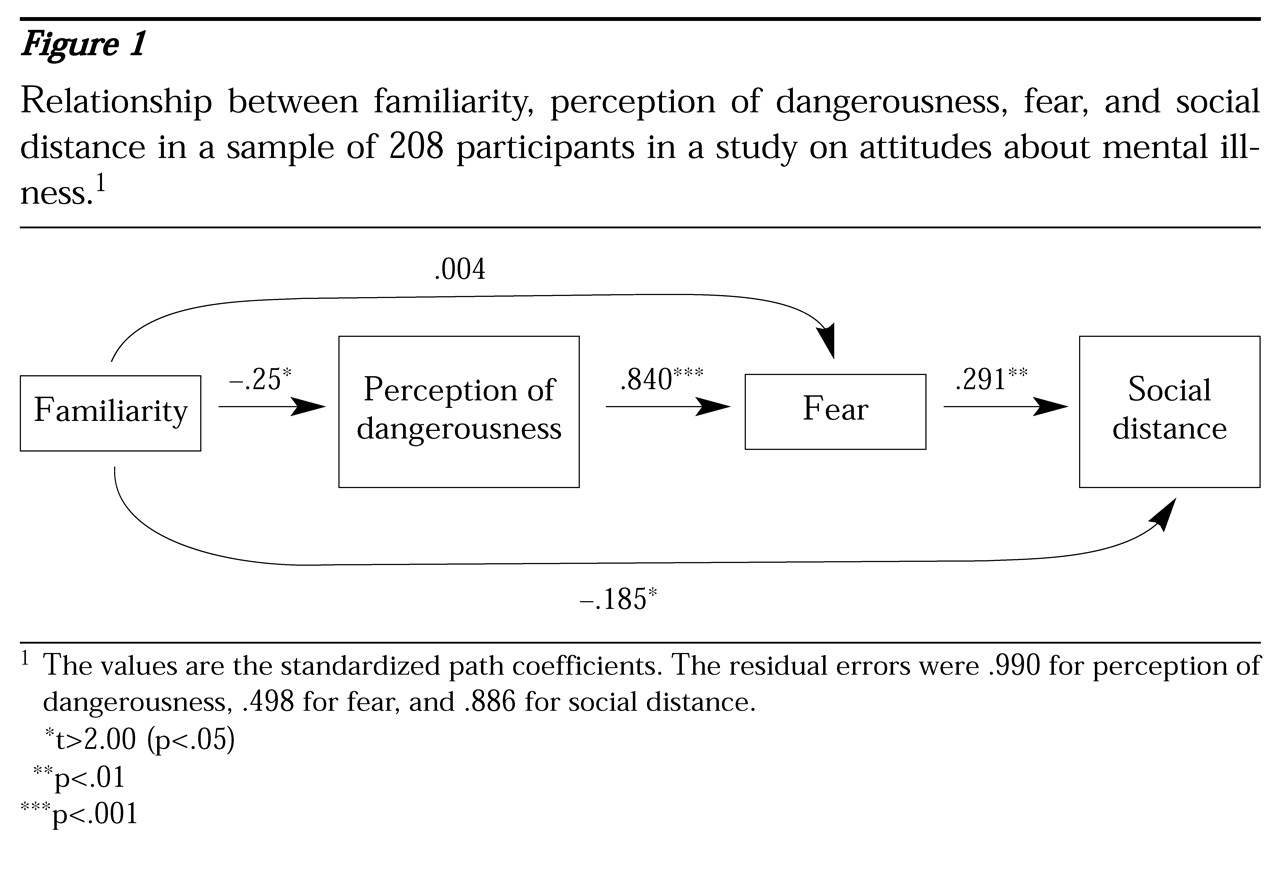
Figure 1 shows the relationship between familiarity, perceived dangerousness, fear, and social distance. Estimations produced a significant chi square value that did not support a fit between the model and the data (χ
2=17.67, df=1, p<.001). Technically, when the proper assumptions are met, the chi square statistic may be used to test the null hypothesis that the model fits the data. However, in practice the statistic is very sensitive to sample size and departures from multivariate normality and will often result in the rejection of a well-fitting model. One alternative way to examine the size of the chi square statistic for the theoretical model is to compare it with the chi square value for the null model. A chi square difference test showed that this model fit the data (p<.001) much better than the null model did (χ
2=368.81, df=6). Moreover, the normed fit index and the comparative fit index were .953 and .951, respectively, supporting the fit between the model and the data.
All but one of the t values for the path coefficients in
Figure 1 were significant (p<.05). As expected, familiarity inversely predicted the perception of dangerousness: the more familiar a study participant was with mental illness, the less dangerous that individual believed persons with mental illness to be. Familiarity was also inversely associated with social distance: participants who were familiar with mental illness were not likely to be socially distant from these individuals. No significant relationship was found between familiarity and fear. As predicted, a strong relationship was found between expectations of dangerousness and fear. In addition, fear was found to positively predict social distance: participants who feared persons with mental illness were more likely to avoid such persons.
Discussion and conclusions
The purpose of this study was to examine the relationship between familiarity, social distance, and stigmatizing attitudes about mental illness. The results seem to support the causal path we proposed. That is, members of the general public who are relatively familiar with serious mental illness are less likely to believe that persons who have psychiatric disabilities are dangerous. Relatively weaker perceptions of dangerousness corresponded with less fear of persons with mental illness, which in turn was associated with less social distance.
These findings seem to support the role of familiarity in the stigma surrounding mental illness. Members of the general public who have greater knowledge about or experience with mental illness are less likely to stigmatize, at least in terms of stereotypes of dangerousness. Moreover, these individuals are less likely to discriminate against persons who have serious mental illness by avoiding them. The effects of familiarity were somewhat pervasive in our model: participants who reported more familiarity demonstrated less social distance.
This finding may be a measurement artifact, because in some ways familiarity and social distance are different sides of the same coin. The Social Distance Scale has been described as a proxy for discriminatory behavior (
8,
27,
32). Individuals report only whether they think they would withhold opportunities from people who belong to a minority group—in this case, persons who have mental illness. Additional research is needed to clarify the relationship between familiarity and social distance by using actual behavioral indexes of avoidance and discrimination.
Frequency analyses of familiarity items from the Level of Contact Report provided some useful information that challenges stigma. One naive notion of serious mental illness is that these disorders are rarely encountered because few persons are seriously mentally ill, and most of these people are confined to remote wards (
33). Contrary to this notion, fewer than 10 percent of the participants in our study reported having no experience with mental illness, whereas more than 90 percent reported learning about mental illness from movies. Unfortunately, much of the information from the film industry promotes stigma. Media analyses have shown that on the whole, people who have mental illness are represented in movies as being dangerous (
34).
Our study also showed that members of the general public have fairly intimate contact with people who have mental illness. More than a quarter of the participants reported working with someone who had a mental illness, and about a third reported that a friend of the family identified him- or herself as being mentally ill. It is likely that these numbers are artificially low, because people who have mental illness learn that keeping their history from coworkers and friends can protect them from public disapproval (
33). Hence members of the general public are likely to have far more coworkers and associates who have mental illness than they are aware of. The important message here is that mental illness is not a rare disorder that locks most of its sufferers away in hospitals: interactions with persons who have mental illness are common.
One concern about this study is whether the sample was representative of the general public. The participants were diverse in race, sex, age, and educational background, partly because they were recruited from certificate and vocational programs at a community college. In addition, the sample was sufficiently large to enable all analyses to be completed with good statistical power (
29). However, the study did not include the kind of probability sampling and stratification strategies that are needed to ensure good external validity. Nationwide survey research of this nature is typically more labor intensive and costly than the approaches used in our study (
35). Our results support our fundamental assumptions and therefore suggest that a broader survey of a representative sample is justified.
Our findings have implications for strategies to address stigma. Approaches to social change that increase the public's familiarity with serious mental illness will decrease stigma. Social psychologists have examined several variables that are relevant to ethnic prejudice and that could be adapted for research on contact with and stigma surrounding persons who have mental illness. One important variable that affects contact is opportunity: members of the majority must have opportunities to interact with members of minority groups if stigma is to be reduced (
36). Thus persons who have serious mental illnesses must have formal opportunities to contact and interact with the general public. Other factors that augment the effects of interpersonal contact include treatment and perception of the participants as equals by members of the public (
37,
38), cooperative interaction (
41,
42), institutional support for contact (
41,
42), frequent contact with individuals who mildly disconfirm the stereotype of mental illness (
43,
44), a high level of intimacy (
45,
46,
47), and real opportunities to interact with members of minority groups (
36). Each of these factors suggests specific hypotheses on how contact between members of the general public and persons who have serious mental illness can be facilitated.