Alzheimer's disease is a progressive form of dementia (
1). During the severe stage of the illness, patients lose the ability to communicate their needs and require significant assistance in activities of daily living. Physical consequences of the progression of dementia predispose persons with advanced Alzheimer's disease to infection and fever (
2), especially aspiration pneumonia (
3,
4) and urinary tract infections (
5,
6). There is no accepted standard treatment for the medical consequences of advanced dementia. The use of aggressive treatment, such as antibiotics and enteral tube feeding, appears to be prevalent (
7).
However, there is substantial evidence that an aggressive medical approach is of limited efficacy. End-stage dementia has been associated with a poor prognosis and a limited life expectancy, which are not improved by invasive procedures (
8). Aggressive treatment of infection does not improve survival rates among persons with severe dementia (
2) and has been associated with accelerated progression of the severity of dementia (
9). Antibiotics and other aggressive measures, although they probably do not improve survival, are associated with numerous deleterious outcomes, including renal failure and ototoxicity, allergic or drug reactions, rash, diarrhea, blood dyscrasias, antibiotic resistance, use of intravenous lines and mechanical restraints, prolonged time to death, and increased costs (
2,
7,
10,
11,
12).
It is well established that people who have Alzheimer's disease and related dementias receive analgesia less frequently than those who are cognitively intact, even when they have similar medical disease burdens (
7,
8,
13,
14,
15,
16). It has been suggested that the low use of pain medication for patients with dementia is attributable not to lower pain levels but to the deterioration of verbal and nonverbal communication, which means that pain goes unreported and unrecognized and thus undertreated (
17,
18,
19,
20). The frequency of pain reporting diminishes with the severity of dementia (
21), and noncommunicative patients with dementia are at risk of having their pain identified much less frequently than communicative patients (
22).
The futility and discomfort of aggressive treatments, combined with the underrecognition and undertreatment of pain among patients with severe dementia, support the use of palliative care for advanced dementia (
23). Among patients with severe dementia, comfort care has been associated with lower levels of discomfort (
12). Furthermore, limited use of antibiotics has not been associated with increased mortality (
2,
23), and aggressive treatment of infections has not been shown to alter underlying disease processes (
9).
Most of the literature on the care of patients with Alzheimer's disease has not focused on end-of-life experiences. Furthermore, little is known about how the severity of dementia is correlated with the use of aggressive or palliative care measures. The goals of this study were to establish the prevalence of aggressive and palliative treatment measures in a well-characterized population of patients with dementia who were sent for autopsy, the relationships of aggressive and palliative care to the severity of dementia, and whether patterns of palliative and aggressive treatment of patients with dementia have changed over time.
Methods
All the patients in the study were living in chronic care facilities at the time of their death. Antemortem data for 279 patients with dementia and 24 control patients who were brought for clinical autopsy between 1985 and 2000 were reviewed. Although the staff of an Alzheimer's disease research center were responsible for conducting autopsies and postmortem chart reviews, all the patients had been receiving standard clinical care until the time of their death. The chronic care facilities were clinical rather than research settings, and all patients were approached equally about the possibility of autopsy. About 10 percent of the patients or a member of their family consented to an autopsy. Informed consent was obtained for all autopsies, and the study was approved by all relevant institutional review boards.
For all autopsies, semistructured chart reviews were conducted by either a physician or a research nurse. Data on the use of systemic antibiotics, narcotic and nonnarcotic pain medications, and nasal oxygen during the last six months of life were used to assess the frequency of aggressive and palliative treatment. Aggressive treatment was defined as use of antibiotics, and palliative care was defined as the use of narcotic or nonnarcotic pain medication or nasal oxygen.
The severity of dementia during the last six months of life was assessed with a chart review that yielded a Clinical Dementia Rating (CDR) score (
24). Possible scores on the CDR range from 0 to 5, with higher scores representing more severe dementia. Ratings of dementia made during clinical interviews and chart-review-generated CDR scores are highly correlated (
25). To assess the relationship between the severity of dementia and the prevalence of either aggressive or palliative interventions, the patients with dementia were divided into three groups on the basis of their CDR scores: .5 to 1, mild dementia (52 patients); 2, moderate dementia (42 patients); and 3 to 5, severe dementia (185 patients).
To determine whether patterns of palliative and aggressive care among patients with dementia have changed over time, the patients in our sample were divided into three cohorts based on date of death. Nineteen of the patients died between 1985 and 1990, inclusive; 124 between 1991 and 1995; and 136 between 1996 and 2000.
Data were analyzed with SPSS 10. Chi square tests were used to compare categorical variables, and t tests were used to compare continuous variables. Differences were considered to be significant if the p value was less than .05.
Results
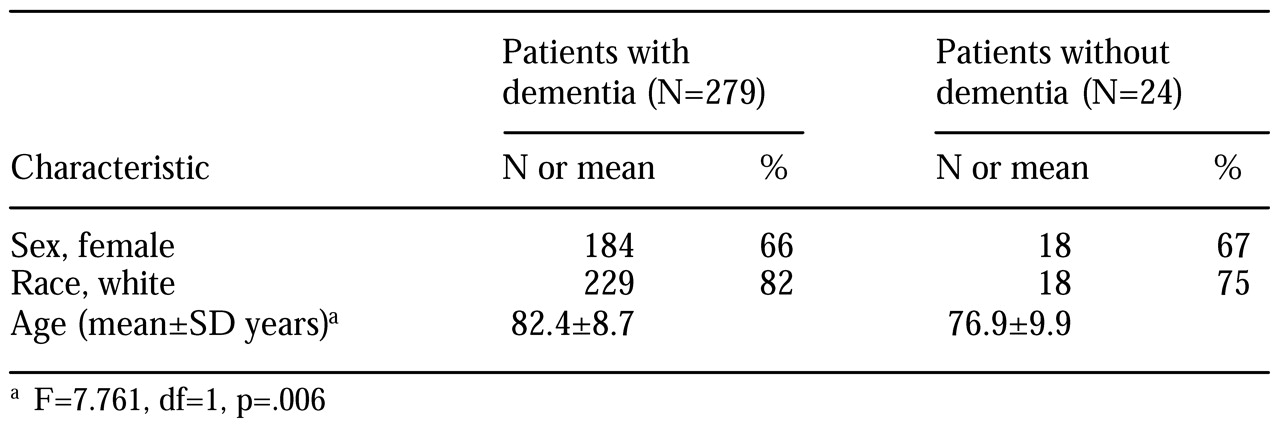
The study patients were residents of 30 different chronic care facilities before their death. A total of 218 patients (72 percent) lived in one facility. Basic demographic data on the study sample are presented in
Table 1. Multiple physicians were involved in patient care at the largest facility. No significant differences were noted between the patients who were autopsied and those who were not in patterns of care across sites or in race, sex, age, educational level, occupation, or medical burden.
Medical burden of the sample
The mean±SD number of medical diagnoses per patient was 10.5±1.4. No significant differences were observed in the number or types of diagnoses between patients with and without dementia or across severity or death cohorts. The five most common medical diagnoses were coronary artery disease (143 patients, or 47 percent), pneumonia (128 patients, or 42 percent), urinary tract infections (90 patients, or 30 percent), hypertension (99 patients, or 33 percent), and congestive heart failure (89 patients, or 29 percent).
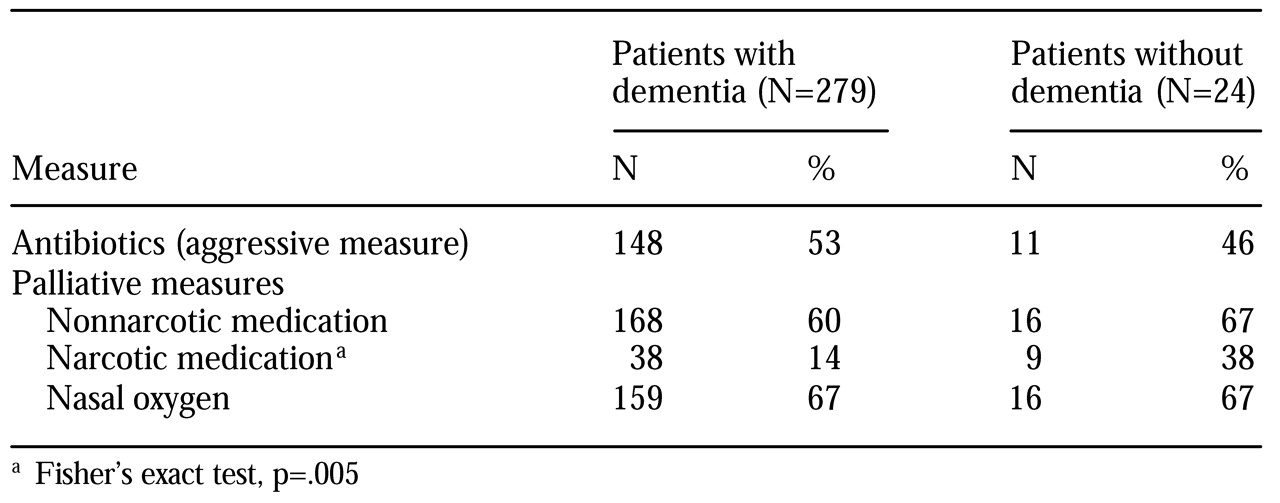
The prevalence of palliative and aggressive measures among the patients with dementia and the control patients is summarized in
Table 2. Use of antibiotics was common in both groups. The patients with dementia were significantly less likely to have received narcotic pain medication.
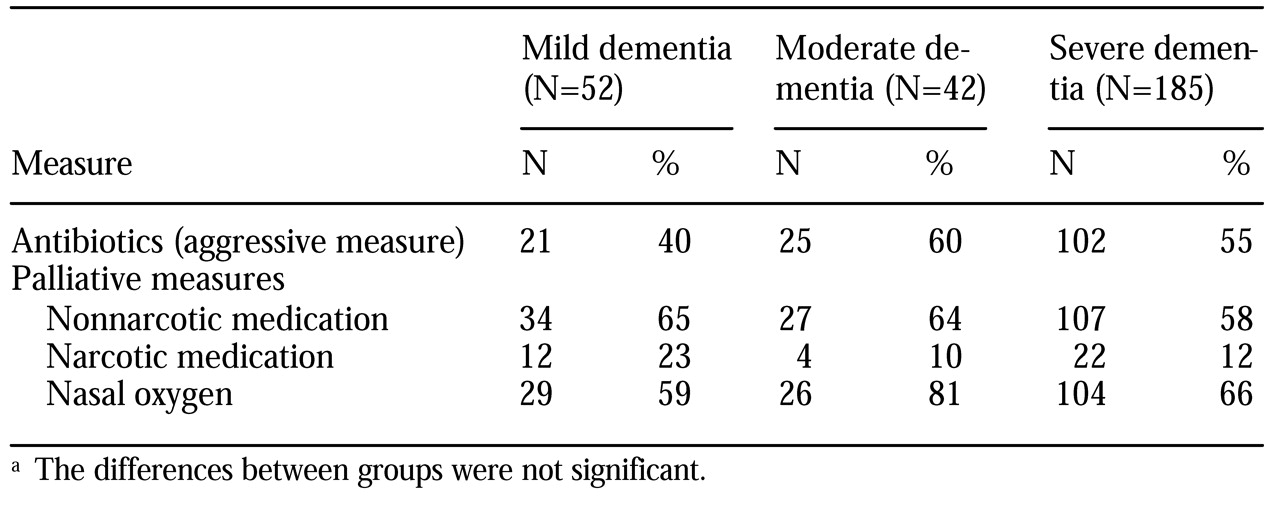
The prevalence of palliative and aggressive measures across severity groups of patients with dementia is summarized in
Table 3. No significant differences were found in the use of any measure. Use of antibiotics was common among patients with dementia, whereas use of narcotic pain medication was relatively infrequent.
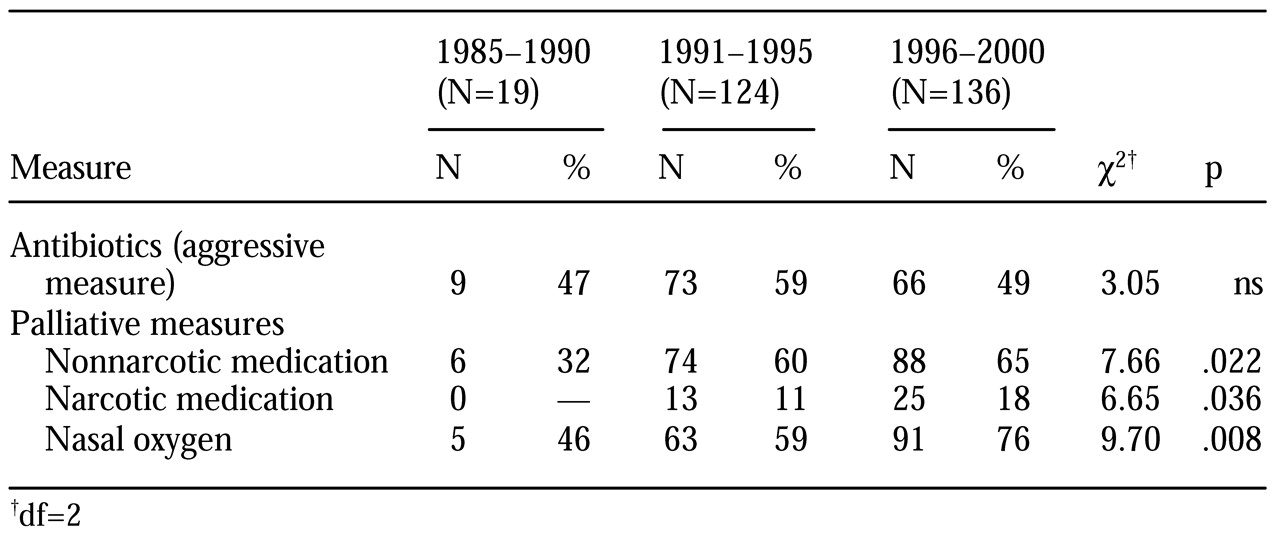
The prevalence of palliative and aggressive measures in the three death cohorts is summarized in
Table 4. Use of nonnarcotic and narcotic pain medications as well as nasal oxygen was significantly more prevalent in the 1996-2000 cohort. Use of antibiotics did not vary significantly over time.
Discussion
We found a high prevalence of systemic antibiotic use (53 percent) and a relatively low rate of use of narcotic pain medications (14 percent) among patients with dementia who were living in chronic care facilities during the last six months of their lives. These findings confirm, in a large and well-characterized patient population, the aggressive nature of treatment of persons with dementia that has been reported in other studies (
7). In particular, patients with severe dementia were as likely as patients without dementia to have received antibiotics. Although antibiotic treatment of intercurrent infections among patients with mild or moderate dementia may reduce mortality, such treatment may not improve survival among those who have more severe cognitive impairment (
2).
Possible reasons for the high prevalence of antibiotic treatment include a lack of advance directives (
8), inadequate training of physicians in discussing end-of-life decisions (
26), and physicians' uncertainty about the course of dementia. Luchins and colleagues (
27) have developed an algorithm that has excellent predictive validity for identifying patients with dementia who have a six-month prognosis. Their criteria include National Hospice Organization criteria and Functional Assessment Staging.
Although patients with dementia are treated aggressively in conventional hospital settings, hospice programs for this patient population are underutilized at the national level (
28), despite the fact that 90 percent of family and professional caregivers view hospices as appropriate for patients with end-stage dementia (
29). Hospice programs were originally developed for patients with cancer, and only a minority of hospice facilities have served persons with dementia. Over the past few years, these services have become more widely available for patients with dementia (
30). However, Medicare reimbursement for hospice services for dementia is below that for hospice services for other conditions (
31).
Patients who had dementia received significantly less narcotic medication than those who did not have dementia, both in the sample as a whole and when we controlled for the presence of potentially painful conditions. This finding confirms numerous reports that persons with cognitive impairment receive analgesia less frequently than those who are cognitively intact (
7,
8,
13,
14). Scales have been developed for assessing pain and discomfort among patients with Alzheimer's disease (
32,
33) in order to enhance the recognition and treatment of pain in this population.
Among patients with dementia, no significant differences were found in the use of pain medication across severity groups. The analgesic needs of patients with dementia have been described as stage independent (
13), indicating that equivalent use of analgesia across severity cohorts is a reasonable approach. It has been suggested that patients who have dementia experience pain very differently from those who are cognitively intact. In studies of patients with dementia and poor cognition, patients with Alzheimer's disease were found to have a stronger tolerance for pain than patients who did not have dementia (
34,
35). Because cognitive difficulties exist along a broad continuum from mild cognitive impairment to severe dementia, the relationship between the experience and the presentation of pain by patients with dementia may be complex.
The administration of nonnarcotic and narcotic pain medications and nasal oxygen has increased over the past 15 years. This trend may be attributable to numerous reports that have called attention to the undertreatment of pain among persons with cognitive impairment (
36) and the need for palliative care for patients with dementia (
12). Although the use of narcotic pain medication among patients with dementia has increased significantly, the use of analgesics is still significantly below that observed among patients who do not have dementia. A broader inquiry into the full range of decisions surrounding end-of-life care—such as the use of intravenous fluids, parenteral feeding, and advance directives—is needed.
The use of antibiotics did not change significantly over the three time cohorts we examined. Thus, although information about pain management may have affected clinical practice during that time, it seems that data on the judicious use of antibiotics has not had a similar impact. Research during the past five years has similarly shown a high prevalence of antibiotic use (
7) and of burdensome procedures in general (
8) among patients with dementia.
Greater use of hospices by patients with dementia may constitute good patient care and good public policy. Facilities may consider education programs for family and staff that focus on the hospice options available to patients. Staff may also be encouraged to actively revisit advance-directive discussions with patients and their families throughout the course of illness. A more favorable Medicare reimbursement policy for hospice services may also be warranted.
The use of selected variables as proxies for palliative and aggressive care does not capture all aspects of the larger domains of clinical decision making. Because participation in this study required that the patient or caregiver provide consent to autopsy, selection bias may have limited the generalizability of the results to the general population.
Conclusions
Administration of antibiotics to patients with dementia who were living in chronic care facilities during the last six months of their lives was prevalent, despite the limited utility and discomfort associated with these measures. That patients with severe dementia received similar treatment to those with milder impairment and elderly patients without dementia, given the poor prognosis of end-stage dementia, may be contrary to good clinical practice. Although pain management may be improving, the practice of using antibiotics does not appear to have changed. An ongoing discussion of the medical and ethical implications of end-of-life care of persons with dementia is needed.
Acknowledgments
This study was supported by grant AG-02219 from the National Institute on Aging. The authors acknowledge the assistance of Sean Morrison, M.D., and Pervaiz Q. Qureshi, M.D.