Historically, psychiatric facilities in the United States were largely a charitable activity (
1). But this pattern changed in the last half of the 20th century, as the entire U.S. health system moved toward for-profit provision of health care (
2,
3). The question of the relative role of for-profit and nonprofit providers in psychiatric inpatient care is quite controversial, driven as much by market concerns as by ideology or evidence of outcomes (
4,
5,
6,
7). Some authors have argued that market efficiency and competition favor expanding the role of the private for-profit sector (
8,
9,
10,
11,
12,
13,
14,
15,
16,
17). Equally convincing points, such as achieving lower costs and better quality, have been made in favor of the provision of nonprofit care (
14,
18,
19,
20,
21).
Although lower overall discretionary public spending is likely in the future, public policy makers should consider the research evidence on the performance differences between for-profit and nonprofit psychiatric health care providers before reducing subsidies or rates of reimbursement. Many private-sector benefits managers require performance ratings of the providers from whom they purchase health services (
22,
23). This article presents a systematic review of the evidence on the comparative performance of for-profit and nonprofit inpatient psychiatric health care providers. In addition, it examines how the performance of for-profit and nonprofit providers in the psychiatric inpatient sector compares with that of providers in other health care sectors and considers the proportion of health care performance studies that is dedicated to inpatient mental health care.
Methods
Two approaches were used to obtain an exhaustive list of studies comparing for-profit and nonprofit providers across the health care sector. First, a computerized bibliographic search of databases and published indexes and abstracts was undertaken. Searches of MEDLINE (Ovid and PubMed versions), Web of Science (Social Sciences Citation Index and Science Citation Index), ABI/INFORM, and Sociological Abstracts were conducted. The following indexing terms were used to retrieve English-language-only articles restricted to human subjects: for-profit, nonprofit, not-for-profit, ownership, health services, investor status, quality, cost, charity, access, psychiatric facilities, health providers, psychiatric hospitals, dialysis centers, health maintenance organizations (HMOs), hospitals, home health care, and nursing homes. The online literature search yielded 1,428 published articles, which were then closely screened and coded. Second, the bibliographies and reference lists of these articles were searched for additional articles.
Three inclusion criteria were used to screen the published articles. First, the analysis of the original empirical data comparing for-profit and not-for-profit health care providers had to include one or more of the following four performance variables of interest: access, quality, cost-efficiency, and amount of charity care. Second, the majority of data collection had to be completed after January 1, 1980. Third, the study had to be published in a peer-reviewed journal. The peer-review status of the journals was determined from the journal's listing in
Ulrich's Periodical Directory (
24).
All studies in the inventory were given equal weight for purposes of this analysis. Because the inventory was comprehensive, sample-based tests of statistical significance were not relevant. Such tests are useful principally when the intent is to draw inferences about the unknown characteristics of a population from a sample with specific, known characteristics. The intent in this study was, rather, to inventory the full universe of studies and characterize the population that met the inclusion criteria without selecting a representative sample.
Unlike a quantitative meta-analysis, the analysis reported here did not aggregate statistical results across studies, because few are commensurable. We attended principally to statements of findings about relative performance and relied on the peer-review process to ensure each study's validity. The authors' conclusions about the relative performance of for-profit and nonprofit providers were coded as findings favoring the superiority of for-profit providers, findings favoring the superiority of nonprofit providers, or as mixed and inconclusive findings that showed no clear superiority between the two types of providers.
In coding the authors' conclusions, we assumed that superior performance was represented by lower costs or better cost-efficiency rather than by higher costs or lower efficiency and by higher quality rather than lower quality. Greater access to health care was considered to be better than less access (
25). More charity care was assumed to be preferred to less and to represent higher performance. How these performance variables were defined and operationalized across the studies is discussed below.
Results
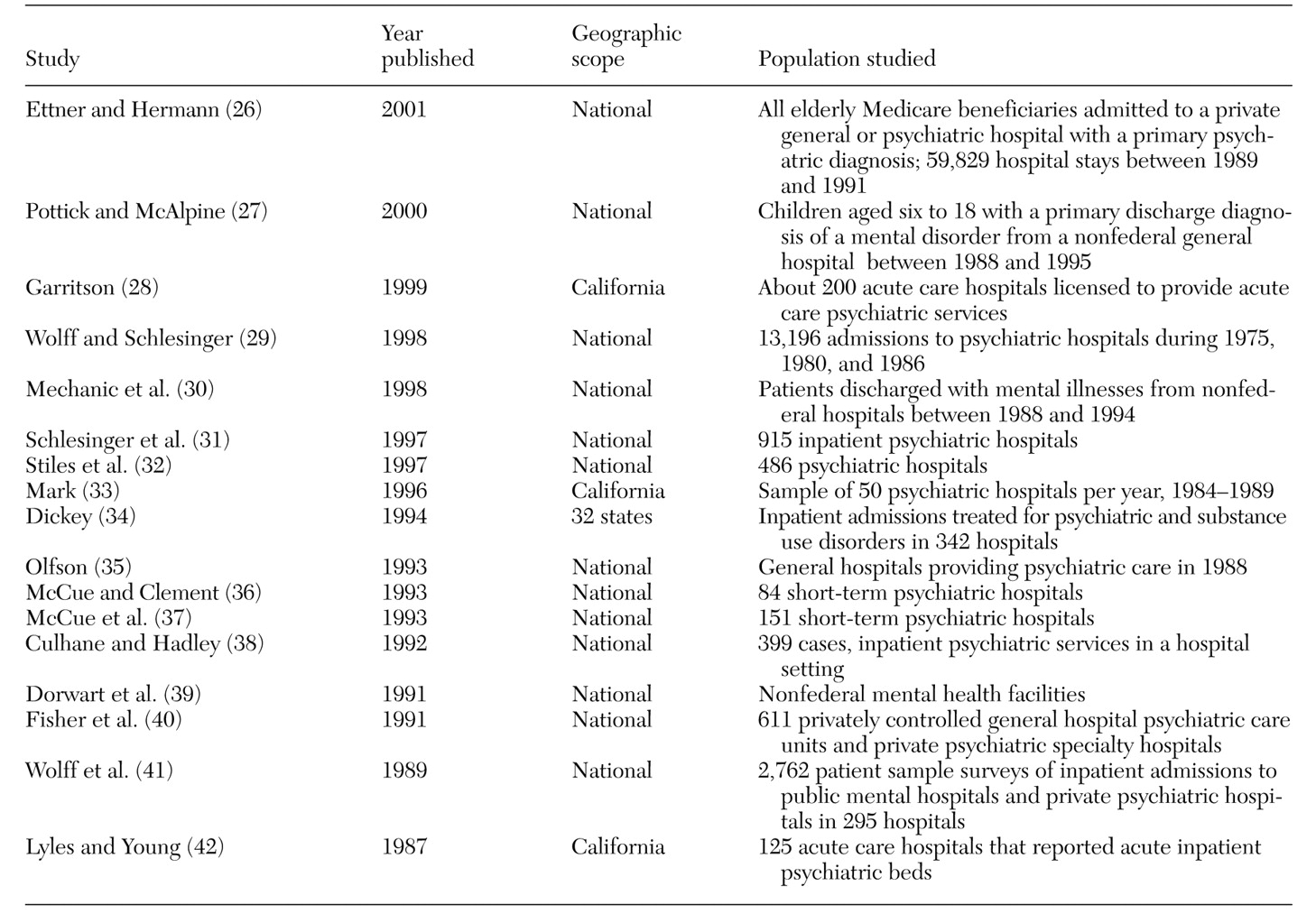
A total of 149 peer-reviewed journal articles qualified for inclusion in our final population of studies assessing the relative performance of for-profit and nonprofit providers across all health care provider types. Seventeen of the 149 articles assessed the performance of psychiatric care providers, and they are specifically cited in this article; a complete list of the 149 articles is available from the first author.
The 149 articles reported a total of 179 performance assessments over the past 22 years. Thirty examined access, 56 considered cost, 69 looked at quality, and 24 studied the amount of charity care provided. Eleven percent of these studies (17 studies) compared the relative performance of inpatient psychiatric care providers, offering a total of 23 comparative performance assessments (
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42) (see
Table 1). Twelve compared for-profit and nonprofit psychiatric inpatient care providers on access, five examined cost, four looked at quality differences, and two compared the amount of charity care provided.
In the articles that were inventoried, the term "inpatient psychiatric care" was found to refer to a range of providers, including mental health care hospitals, freestanding psychiatric inpatient facilities, psychiatric specialty hospitals, mental health care facilities, and general hospital units specializing in acute inpatient psychiatric care. The studies that assessed inpatient mental health care providers examined performance in a variety of geographical locations. Thirteen studies were national. One study included data from 32 primarily eastern states. Three were single-state studies with California as the focus. A few studies considered special populations, for example, children, adolescents, or elderly patients.
Performance was defined and measured in several ways. Cost or efficiency referred to expenses per patient, cost per patient day, cost per case, net patient revenues, mark-up, or profitability. Measures of high-quality performance included lower adverse event rates, lower mortality rates, lower disenrollment rates, the presence of programs offering a full continuum of health care, more patient education, or a higher Health Plan Employer Data and Information Set (HEDIS) score from the National Committee for Quality Assurance. In the subset of studies that focused on psychiatric inpatient care, higher quality was reported as a lower noncompliance notification rate, a broader array of services, fewer inappropriately short stays, and lower rehospitalization rates.
Access to health care for both mental health care providers and all other provider types was typically defined as whether the provider took on a fair share of Medicaid and Medicare patients and other expensive-to-treat patients and whether the provider offered costly treatments, such as unprofitable emergency room care. Most studies considered charity care to be any treatment of bad-debt patients or provision of unpaid services or uncompensated care.
The amount of research comparing the performance of for-profit and nonprofit psychiatric inpatient health care providers increased across the past two decades. Data collection was at a peak in the late 1980s, when eight research projects whose findings were later published in peer-reviewed journals were concluded. As for actual publication dates, however, 15 articles were published on this topic since 1990, and only two were published in the 1980s. The mean time interval between data collection and publication was 5.88 years for articles comparing for-profit and nonprofit psychiatric inpatient care providers, slightly greater than the mean time of 4.74 years for all other types of providers.
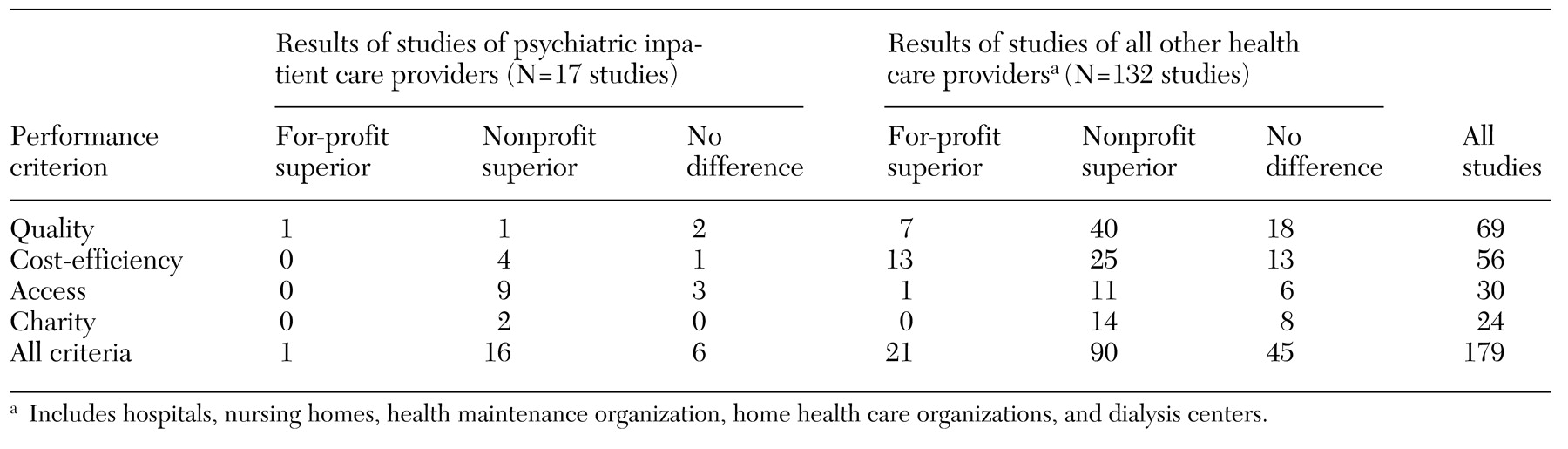
The major—and unexpected—finding of this synthesis of studies was the performance superiority of the nonprofit psychiatric inpatient care providers compared with the for-profit providers (
Table 2). Sixteen of the 17 studies (96 percent) found that the performance of the nonprofit psychiatric inpatient care providers was better than or equal to that of their for-profit counterparts across all four performance criteria. The nonprofit care providers were found to have performed best in 70 percent of the comparisons. Twenty-six percent of the comparisons indicated no difference between the for-profit and nonprofit providers.
For all other health care provider types—hospitals, nursing homes, HMOs, home health care organizations, and dialysis centers—the results were much the same, although less pronounced, than for the psychiatric inpatient care providers. Most of the 132 studies failed to demonstrate that for-profit providers maintained a level of performance equal to or better than the nonprofit providers (
Table 2).
Discussion
The number of for-profit psychiatric inpatient providers appears to have declined substantially in recent years (
43), and the lower-than-expected level of performance of these providers found in this synthesis of studies may provide an explanation. Although about half of inpatient mental health care providers in 1997 were for-profit entities, that proportion declined to about one-third by 1999 (
3,
44,
45). Besides providers that were affected by performance issues, some for-profit enterprises may have simply concluded that the financial payoff was too low to warrant further investment. Some for-profit providers were also subject to criminal investigation because of fraud charges in the 1990s, and the bad publicity did not help the bottom line (
46). Patient lawsuits, oversupply, and capitation fee structures similarly reduced profit margins (
43).
Economists typically expect the cost performance of for-profit providers to be superior to that of nonprofit providers, and the hope is that for-profit providers can maintain quality while also being cost-effective (
47). On the other hand, one early study was a forewarning that this expectation was unrealistic; it reported that for-profit outpatient clinics were "highly motivated by commercial concerns" and billed more per patient than nonprofit clinics (
48). However, the path to quality improvement in psychiatric inpatient care, while known, is expensive. Some examples illustrate this point. Case management has been found to improve outcomes (
49), as has follow-up care after an initial inpatient mental health episode (
50). Both may add to costs and reduce profit margins. Higher-quality psychiatric inpatient care includes reducing the use of restraints, but often the trade-off is that staffing must be increased or video monitoring equipment installed to ensure safety (
51). Several studies in this inventory suggested that reducing costs may also reduce quality, something unanticipated and left undiscussed by formal economic models.
Management experts have hypothesized that nonprofit organizations in general may be better at "the motivation and productivity of knowledge workers" than private for-profit businesses (
52). Psychiatric inpatient care may be an important example of this type of knowledge-based enterprise. Private nonprofit organizations have long been known to produce public goods of great value to society. They save taxpayers scarce resources by caring for poor patients who might otherwise be cared for only at public inpatient facilities (
53). Authorities in the business field have considered nonprofit managers to be especially creative and innovative (
54). A 2000
Wall Street Journal article (
55) presented the opinion that "people who run charities and other nonprofits have a long history of managing under uncertain conditions, satisfying multiple stakeholders, building passionate work forces and developing non-financial measurements of goals—the kind of issues that are becoming hot topics in corporate management." Our research supports these views.
Our study had several limitations that should be noted. Perhaps the most serious limitation is our acceptance of the authors' judgment of relative performance in each of the studies we reviewed. Some authors may have exaggerated or overgeneralized their empirical findings. Of course, unless such a bias is slanted toward one type of provider, this kind of error would not dramatically alter our results. If the recent political climate creates any bias, it would tend to support a presumption against the superiority of nonprofit provision of care. In addition, conclusions from the available research cannot be taken as indicative of national trends. Several of the studies drew on state-level rather than provider-level data; others were case studies. Finally, the results reflect only published studies from the last 22 years and do not support extrapolation to the future.
Conclusions
This article summarized the results of studies that compared the performance of for-profit and nonprofit psychiatric inpatient care providers in the United States on the basis of data collected since 1980. On the whole, the data did not reveal any special performance advantage in the for-profit provision of inpatient psychiatric care. The proportion of studies that reported superior performance of nonprofit providers was greater for psychiatric inpatient mental health providers than for all other health care providers. The review found little evidence that for-profit inpatient health care in general has achieved superiority on any of the four basic performance variables considered. The overwhelming majority of the studies undermine a performance rationale for public policy decisions to expand for-profit inpatient health care.
Acknowledgments
The authors thank Jennifer Bennett, B.A., and Malorie Gist, J.D., for help in searching the databases, managing the archives of articles, and preparing the manuscript. This research was supported by the Center for Society and Population Health, School of Public Health, University Texas-Houston Health Science Center.