Poverty dramatically increases the risk of common mental disorders, such as depression (
1,
2,
3). Probably as a result of historical experiences, persons from ethnic minority groups are overrepresented among the impoverished. Whereas only 20 percent of white Americans report incomes below 200 percent of the poverty level, at least 50 percent of Americans from racial or ethnic minority groups are poor according to this definition (
4). Few studies have examined the effectiveness of providing depression care to poor persons from ethnic minority groups. In this study we examined the effect of enhancing care for depression among poor, ethnically diverse patients.
Few data are available on the effectiveness of mental health treatment by race, culture, or ethnicity (
5). However, most practitioners agree that the delivery of mental health care should be consistent with the beliefs, values, and social conditions of those being served. In this study, we provided psychotherapy rather than medication because of patients' preferences for this type of care (
6). Depressed patients of all backgrounds prefer psychotherapy to medications (
7); African-American patients, in particular, prefer this form of therapy (
8,
9). We chose a form of psychotherapy that has proven efficacy (
10)—cognitive-behavioral therapy (
11,
12). Cognitive-behavioral therapy was shown to be effective for treating depressive symptoms in a Puerto Rican sample (
13) and has shown promise in naturalistic, nonrandomized studies of care for low-income and minority patients with major depression (
14,
15).
Persons from ethnic minority groups are less likely to seek outpatient mental health care than white patients and more likely to leave such care prematurely (
16). Fortunately, depressed persons who fail to seek mental health treatment can often be identified and treated in general medical settings (
17). Schulberg and colleagues (
18) found that short-term psychotherapy and antidepressant medications were effective in a sample of general medical patients, 45 percent of whom were nonwhite. However, only 33 percent of the patients who received pharmacotherapy and 42 percent of those who received psychotherapy completed treatment. Similarly, patients from ethnic minority groups who seek care in community mental health centers are more likely to end care prematurely (
19,
20). Premature withdrawal from treatment is less evident in ethnic-specific services (
21,
22,
23), which are the most effective in retaining Spanish-speaking patients in care (
23).
Clinical case management interventions have been used successfully to engage and maintain persons with serious mental illness in outpatient community care (
24). In this study, we developed a case management intervention to engage and maintain depressed general medical patients in care. Furthermore, because of ongoing stressors, impoverished patients may benefit less from mental health treatments than patients who are not poor (
25). Stressful life events have been found to be common among poor persons (
26,
27). Therefore, the clinical case management intervention we developed to engage patients in care also attempted to decrease ongoing stressors.
In this exploratory study of engaging and treating impoverished primary care patients from ethnic minority groups, we examined the impact of adding a clinical case management intervention designed to engage and maintain patients in care and to improve outcomes. We predicted that patients who received case management would be more likely to enter, stay in, and benefit from care than patients who received cognitive-behavioral therapy alone. Because we provided culturally tailored services for Spanish-speaking patients, we predicted that these patients' response to care would equal that of English-speaking patients.
Methods
All the study procedures were approved by the institutional review board of the University of California, San Francisco.
Treatment
Cognitive-behavioral therapy. A cognitive-behavioral treatment manual was adapted from an eight-session manual, the Depression Prevention Course (available from the first author), based on the book
Control Your Depression (
12). The manual included methods derived from the work of Beck and associates (
28), Burns (
29), Ellis and Harper (
30), Lewinsohn (
31), and Lakein (
32). Treatment was adapted for low-income patients by lowering the literacy level necessary for participation and focusing on pleasant activities that are largely free of charge. The English-language manual (
33) was developed specifically to treat low-income and minority primary care patients by using diverse cognitive and behavioral strategies. A similar—but culturally adapted—manual was developed in Spanish (
34).
The patients received manuals outlining 12 sessions in three modules (each covering four sessions). Sessions were held weekly. The modules covered changing depressogenic thinking, increasing pleasant activities, and improving interactions with others. To make the intervention viable within the ongoing system of referral from the medical clinics, new patients were "folded into" ongoing groups at the beginning of each module. Patients who completed eight of the 12 sessions were considered to have received an adequate treatment trial. The groups were led by a licensed clinical psychologist or a licensed clinical social worker with expertise in cognitive-behavioral therapy and in treating low-income and minority patients. Co-therapists for the groups were trainees completing intensive training in cognitive-behavioral therapy.
Culturally adapted care. The cultural adaptations for the Spanish-speaking patients included having bilingual and bicultural providers, providing all materials in Spanish, training staff to show respeto and simpatia to patients, and allowing for somewhat warmer, more personalized interactions than are typical for English-speaking patients.
Enhanced intervention. The case management intervention was a flexible intervention that took place over a six-month period. It was developed by a senior licensed clinical social worker specializing in case management interventions for people with serious mental illness and the bilingual and bicultural licensed clinical social worker who headed the case management intervention team. The case managers engaged in active telephone outreach as soon as patients were referred to them. The case managers were trained in cognitive-behavioral therapy and maintained this model within the case management. They assessed patients' self-reports of problems in housing, employment, recreation, and relationships with family and friends and, jointly with patients, set goals to work toward together in areas they assessed as problematic.
Recruitment
Participants were recruited for this study from the depression clinic at San Francisco General Hospital, which was established to accept referrals from outpatient general medical clinics located at or associated with San Francisco General Hospital. Staff from the depression clinic evaluated all patients who were referred from their primary care providers for psychiatric care, providing referral for those who needed mental health care other than care for depression. The medical clinics served primarily publicly insured and indigent patients. All patients referred to the depression clinic were contacted multiple times when necessary to encourage them to come in for evaluation. In addition, the depression clinic staff worked closely with referring physicians to encourage patients to enter care.
During the four and a half years of the study, primary care practitioners referred 1,163 patients to the depression clinic. Of the patients referred, 400 (34 percent) were found to be ineligible for the services of the depression clinic because of either current substance abuse or psychosis established through routine diagnostic workups based on the Structured Clinical Interview for DSM-III-R36 (SCID) (
35). In addition, 513 patients (44 percent) were lost to contact. Despite extensive telephone outreach and communication with the primary care providers, a number of patients who were referred to the depression clinic subsequently moved, lost telephone service, or were unreachable for a variety of other reasons. A total of 250 patients (22 percent) were eligible to participate in the depression clinic after completion of the required diagnostic interview.
The study participants had major depression and were neither psychotic nor currently (during the previous month) abusing alcohol or drugs. Two patients could not be reached for further participation, 34 declined, and ten were found to be inappropriate on clinical evaluation. A total of 199 patients, 80 percent of those appropriate for the depression clinic, participated in this intervention trial. Informed consent was obtained before random assignment.
The study participants were ethnically diverse. Of the 77 participants for whom Spanish was the first language, all but five (6 percent) (second-generation Mexican Americans) were foreign born; 25 (33 percent) were from El Salvador, 17 (22 percent) from Nicaragua, 13 (17 percent) from Mexico, seven (9 percent) from South America, five (6 percent) from Puerto Rico, four (5 percent) from Cuba, and one (2 percent) from Guatemala. Of the 122 participants for whom English was the first language, 46 (38 percent) were African American, 57 (47 percent) were white, and 18 (15 percent) were Asian or American Indian and either were born in the United States or had lived in the United States for at least 30 years.
Assessments
Baseline assessments were repeated four and six months after the initial group treatment session. All measures were available in Spanish. A Spanish-language version of the SCID was obtained from the psychiatric department of San Juan de Dios in Guadalajara, Mexico, where Mexican psychiatrists had forward-translated the measure for their own use. A Spanish-language version of the Beck Depression Inventory (BDI) was back-translated during previous research at the study site (
36). The Social Adjustment Scale (SAS) was back-translated into Spanish by bilingual members of the research team.
Measures
The SCID was used to establish a diagnosis of current major depression. Current anxiety disorders were also assessed. The SCID was also used to exclude patients who met criteria for psychotic disorders or current substance abuse. The BDI (
37) was used to assess the severity of symptoms of depression. The modified SAS developed by Weissman and Paykel (
38) and revised by Elkin and colleagues for the National Institute of Mental Health Collaborative Treatment of Depression Study (
39) assessed adjustment in work, home, social, and leisure activities. In addition, this measure assesses ability to relate to family and friends. A chronic disease score was derived from computerized hospital records indicating type of medications prescribed to patients, using methods developed by Von Korff and colleagues (
40).
Analyses
Outcome analyses were conducted with two samples. First, the intent-to-treat sample of 199 patients was analyzed to compare changes in depressive symptoms. These analyses controlled for all differences in demographic and clinical characteristics of the Spanish- and English-speaking patients. Measures of depressive symptoms among English-speaking patients at four-month follow-up were missing for 16 (26 percent) of those who received cognitive-behavioral therapy alone and 12 (20 percent) of those who received cognitive-behavioral therapy plus case management; in both Spanish-speaking groups, measures were missing for 16 (21 percent) of the patients. At six-month follow-up, measures were missing for an additional 2 to 4 percent across all groups. To impute missing values, we used group mean substitution, which is likely to underestimate the standard errors and can lead to overestimation of treatment effects.
Outcomes were examined through repeated-measures analysis of variance (for BDI scores) or analysis of covariance (for SAS scores), with treatment assignment, language, and the interaction of treatment assignment and language as between-subject factors, comparing mean scores at baseline (for both BDI scores and SAS scores), four months after the initial session (for BDI scores), and six months after the initial session (for both BDI and SAS scores).
Second, the 132 patients who completed treatment by attending at least eight sessions of cognitive-behavioral therapy were analyzed separately; no data were missing from this sample.
Results
Participants
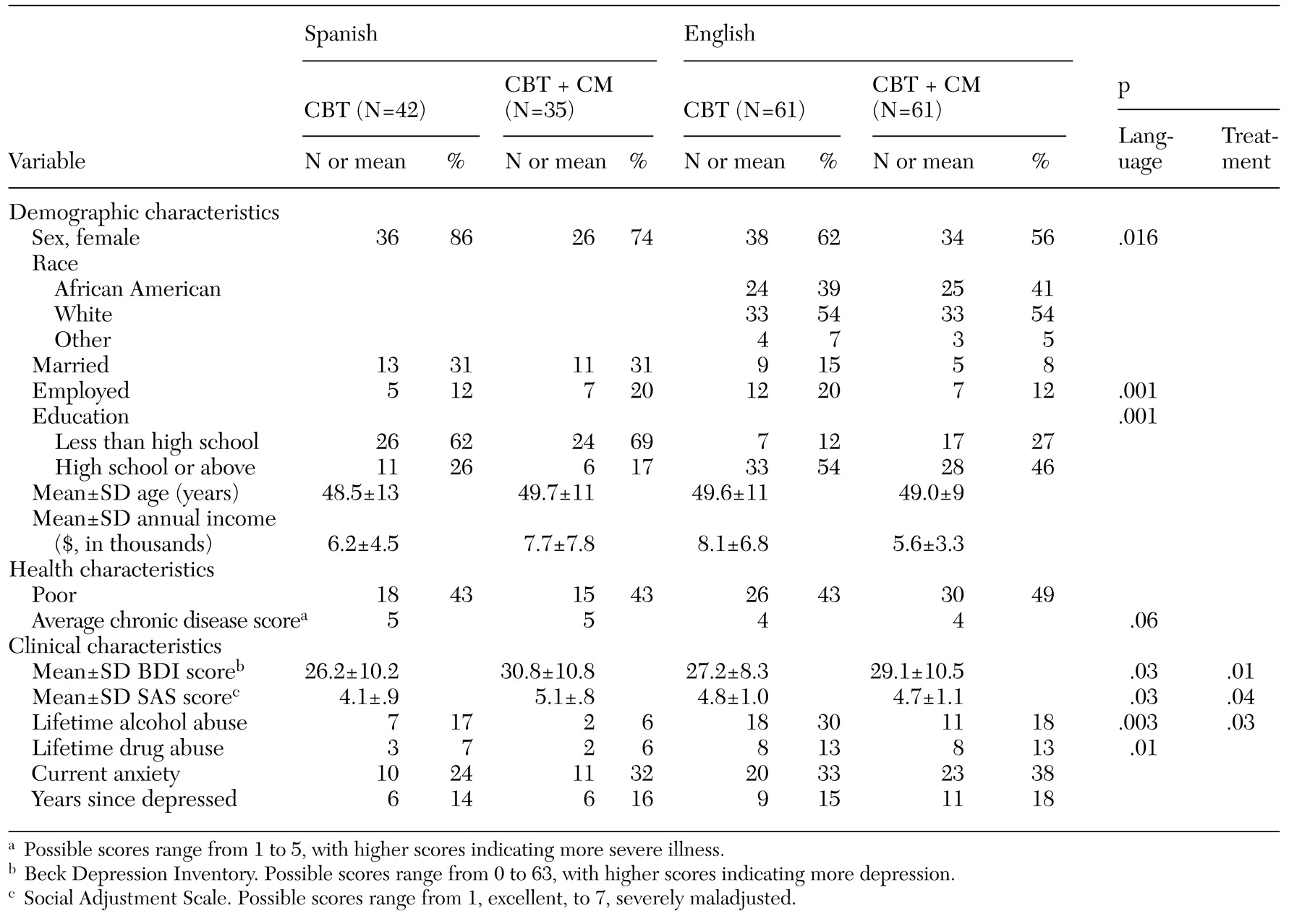
The demographic and clinical characteristics of the 199 study participants are summarized in
Table 1, categorized by whether the patients' first language was English or Spanish and by the type of treatment they received. The overall sample was multiethnic, middle-aged, predominantly female, and impoverished. The differences between the Spanish- and English-speaking groups were consistent with national statistics.
The study participants reported initially high levels of depression and poor functioning. High rates of comorbidity were also apparent. Most of these participants had a first episode of depression nearly 15 years before they participated in this study. Clinical characteristics varied by treatment assignment. The patients who received supplemental case management had higher baseline depression scores and poorer functioning as measured by the SAS. The patients who received cognitive-behavioral therapy alone were more likely to have a history of alcohol abuse. We controlled for these factors in further analyses. In addition, we conducted sensitivity analyses that excluded all patients who had a history of alcohol abuse. The findings did not change when patients who had a history of alcohol abuse were excluded from the analyses.
Clinical case management
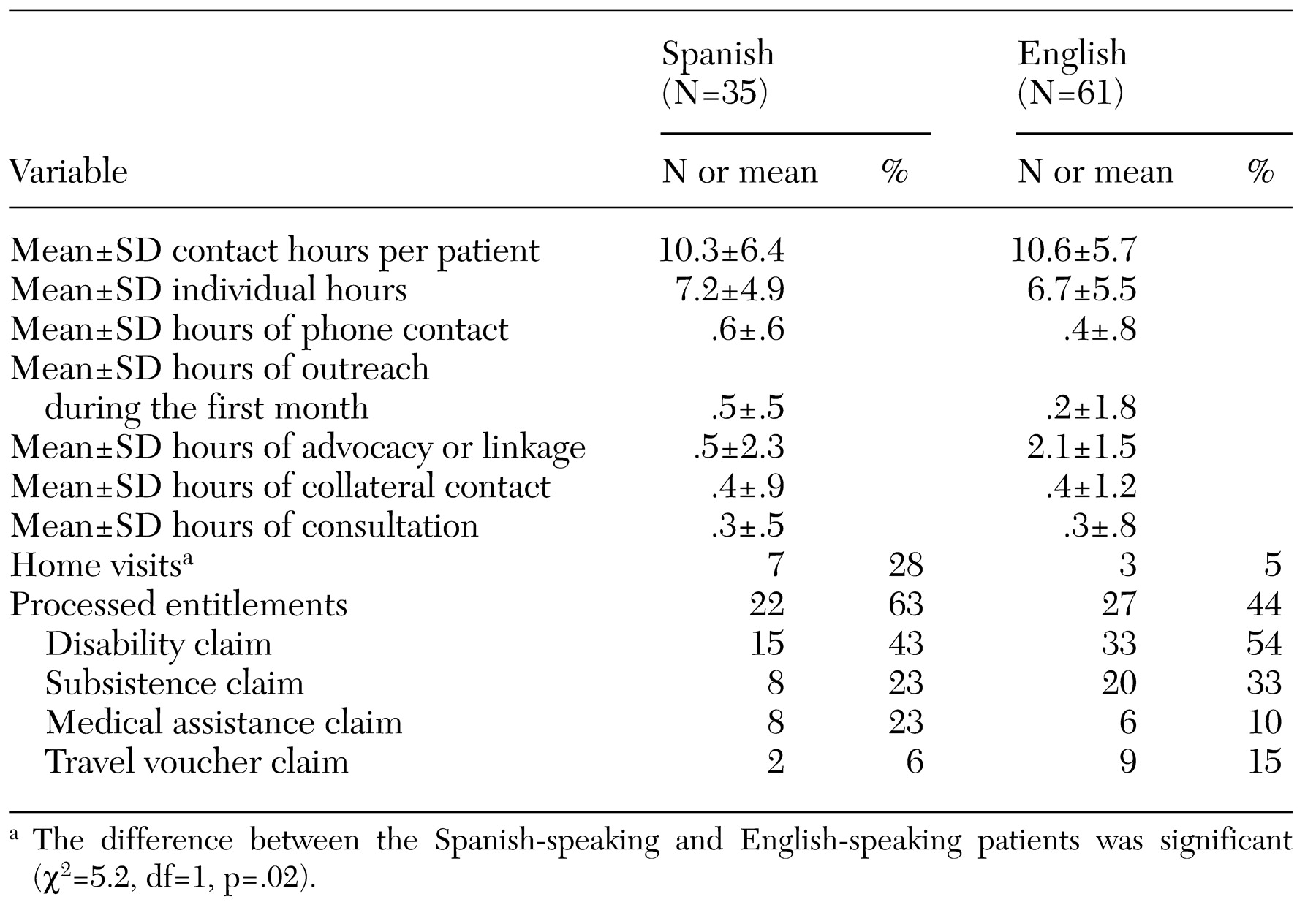
The clinical case managers kept detailed records of the services they provided over the six-month period. The results are presented by language group in
Table 2. The case managers averaged approximately ten hours of caring for each patient, mostly in individual sessions. Entitlements were processed for approximately half of the participants. Few differences were found in the use of services between the Spanish- and English-speaking patients, although home visits occurred more often for Spanish-speaking than for English-speaking patients.
Attrition
We predicted that supplementing group cognitive-behavioral therapy with case management would engage patients in care and prevent premature termination of care. Patients were less likely to drop out of cognitive-behavioral therapy before they had received an adequate dose of eight sessions if they had also received supplemental case management. Among the 77 Spanish-speaking patients, 23 (30 percent) dropped out of therapy: 17 (40 percent) of those who received cognitive-behavioral therapy alone and six (17 percent) of those who received supplemental case management (χ2=5.0, df=1, p=.03). Among the 122 English-speaking patients, 44 (36 percent) dropped out of therapy: 27 (44 percent) of those who received cognitive-behavioral therapy alone and 17 (28 percent) of those who received supplemental case management (χ2= 3.8, df=1, p=.05). Patients who received case management also attended more cognitive-behavioral therapy sessions than patients who received cognitive-behavioral therapy alone (10.5±4.6 compared with 8.4±4.7, t=3.21, df=196, p=.002).
No significant differences were found between Spanish- and English-speaking patients in the likelihood of dropping out. We examined the number of sessions attended by demographic and clinical characteristics of the patients. Only age was a significant predictor of dropout; younger patients were more likely to drop out of treatment than were older patients.
Effect on depression
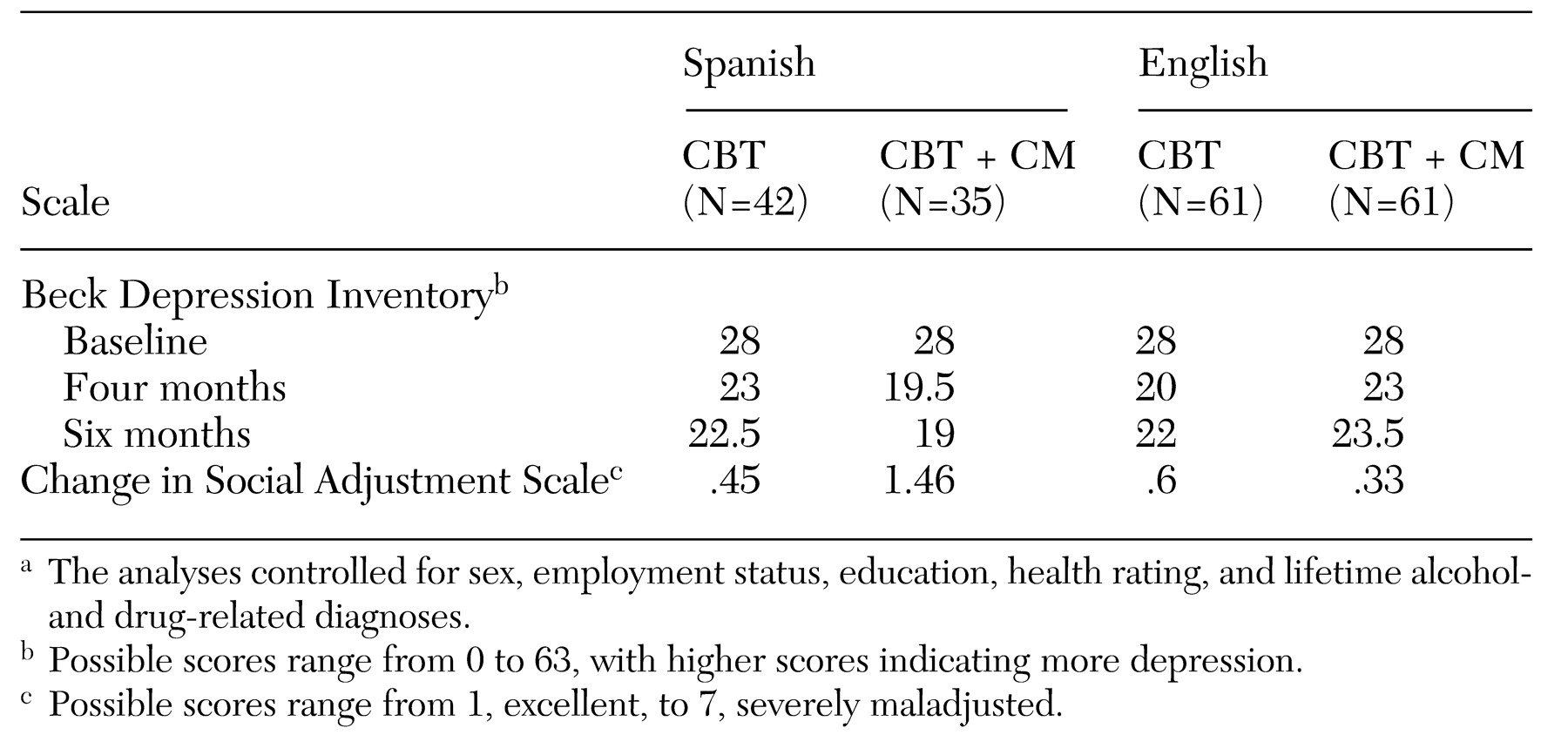
We predicted that patients who received cognitive-behavioral therapy supplemented with case management would have fewer depressive symptoms at six-month follow-up than those who received cognitive-behavioral therapy alone. The results of the repeated-measures analysis of variance that included all participants supported this hypothesis. A significant interaction of treatment assignment by language (p=.04) was found. The results are presented in
Table 3.
The Spanish- and English-speaking patients responded equally well to cognitive-behavioral therapy alone. However, among Spanish-speaking patients, those who received supplemental case management reported fewer depressive symptoms at four and six months than those who received cognitive-behavioral therapy alone. By contrast, among English-speaking patients, those who received supplemental case management reported more depressive symptoms at four months than those who received cognitive-behavioral therapy alone. However, this difference was not significant at six-month follow-up. The results were similar when the analysis included only patients who completed treatment (attended at least eight weeks of therapy).
Effect on functional status
The results of the intent-to-treat analyses showed no significant main effect of treatment assignment nor an interaction between assignment and first language. Results of the analysis of covariance again showed a significant interaction of treatment assignment by language (p=.03). The results are presented in
Table 3. The Spanish-speaking participants were more likely to improve in functioning if they received supplemental case management as opposed to cognitive-behavioral therapy alone. By contrast, the English-speaking participants improved similarly across the two treatment conditions.
Exploratory analyses
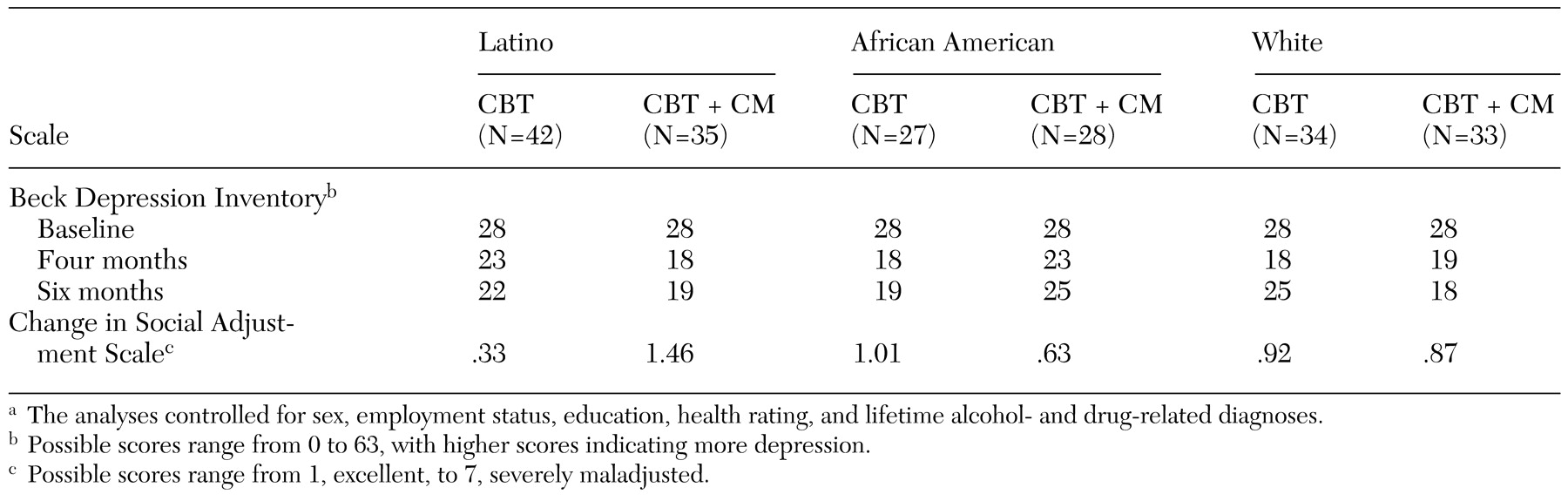
To better understand these findings, a series of exploratory analyses were undertaken that examined racial or ethnic differences in response to the intervention. These analyses compared the 77 Latinos, 53 African Americans, and 67 participants who were classified as white or other. The 13 Asians, American Indians, and Pacific Islanders did not differ from the white patients in baseline characteristics and so were included with this sample in the analyses. However, excluding these individuals from the analyses did not change any of the results.
Repeated-measures analysis of variance was again used to assess the impact of ethnicity, treatment, and the interaction of ethnicity and treatment on depressive symptoms. A near-significant interaction was found (p=.06). The results are presented in
Table 4. At both follow-up points, the supplemental case management, as opposed to cognitive-behavioral therapy alone, was associated with fewer symptoms of depression among the Latino patients, somewhat fewer symptoms among the white patients, but more symptoms among the African-American patients. A similar interaction of ethnicity and treatment was found in predicting the impact of the interventions on functioning (p=.06). As can be seen in the table, supplemental case management was associated with better functioning for Latino patients compared with cognitive-behavioral therapy alone. Supplemental case management was not associated with improved functioning among white patients or African-American patients. In fact, the African-American patients who received cognitive-behavioral therapy alone showed greater improvement.
Discussion and conclusions
This exploratory study examined the impact of enhancing standard care for depression in the treatment of impoverished, ethnically diverse primary care patients. We examined whether adding clinical case management to group cognitive-behavioral therapy would help engage patients in care and improve outcomes. The enhanced care was associated with a lower likelihood of early termination of cognitive-behavioral therapy. The patients who received case management were significantly more likely to complete eight weeks of cognitive-behavioral therapy than the patients who received cognitive-behavioral therapy alone. The enhanced intervention was also effective in reducing depressive symptoms and improving functioning among Spanish-speaking patients but not among English-speaking patients. Exploratory analyses suggested that the patients who were classified as white or "other" responded somewhat positively to the enhanced intervention but that African-American participants did more poorly.
Caution should be exercised in interpreting these initial findings on the impact of interventions for depression among impoverished patients from ethnic or racial minority groups. First, the finding that the effect of supplemental case management could be dependent on culture was not predicted. Also, the case management activities differed between groups; Latinos received more home visits. Second, the case management intervention influenced patients' participation in the study and thus introduced bias into the comparative samples. Furthermore, dropout from treatment and failure to complete all measures could have affected these findings. Third, the samples were relatively small, and many of the results were of only borderline statistical significance. However, the results are remarkably consistent across study indexes of change.
Finally, this study examined treatments for depression among low-income and minority patients who were referred by their primary care physicians. Among those who were referred, 34 percent were not eligible to participate because they were either psychotic or currently abusing alcohol or drugs. Furthermore, we were unable to contact 44 percent of the patients who were initially referred. The results cannot be generalized to medical patients with comorbid psychiatric disorders or to those who cannot be contacted through traditional telephone outreach.
Despite these shortcomings, this study provided new information relevant to providing quality care for low-income and minority patients. This is the first study of interventions for depression among impoverished patients who were not seeking care. Overall, in this high-risk sample, 66 percent completed treatment. This finding compares favorably with the rate of 68 percent found in the National Institute of Mental Health collaborative treatment of depression study (
39). Furthermore, among patients whose care was enhanced with clinical case management, the completion rate was 76 percent. Therefore, this study has established that poor and minority populations are willing to participate in both mental health interventions and studies of such interventions.
Although the study participants improved overall as a result of the interventions, their depression scores remained relatively high both at the completion of therapy and two months later. This finding could have been due to the generally higher scores on depression scales among patients with medical illness (
41). On the other hand, these patients may not have responded as fully to care as would be desirable. Many of these impoverished patients reported that their first episode of depression had been nearly 15 years earlier. Given that these patients had generally not previously obtained psychiatric care, the chronic course of their untreated depression could have meant that only a partial response to this care was possible. Clearly, interventions among impoverished persons earlier in their lives could be more beneficial. Furthermore, despite initial preferences for psychotherapy, antidepressant care provided to these patients in culturally sensitive ways may be necessary to further enhance treatment effects.
Acknowledgments
This study was supported by grant R-29-MH-47855 from the National Institute of Mental Health. The authors thank Robert Surber, L.C.S.W., Bill Hargreaves, Ph.D., Ricardo Muñoz, Ph.D., Jacqueline Persons, Ph.D., Chuck Garrigus, L.C.S.W., Jill Caire, Ph.D., and Emmet Velten, Ph.D.