Why Is It Easier to Get Mad Than It Is to Feel Sad? Pilot Study of Regulation-Focused Psychotherapy for Children
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Current Treatment Approaches
Regulation-Focused Psychotherapy for Children (RFP-C)
Methods
Participants
| Participant characteristic | Child 1 | Child 2 | Child 3 |
|---|---|---|---|
| Age (years) | 9 | 5 | 8 |
| Race-ethnicity | Black/non-white Hispanic | Black | White |
| Medication | No | No | No |
| Diagnosisa | ODD, dysthymia | ODD | ODD, enuresis |
| Estimated FSIQb | 83 | 95 | 91 |
| Prior therapy | Yes | No | Yes |
| School type | Public | Public | Public |
| Family income | 0–19,999 | 20,000–39,999 | 120,000–139,999 |
| Caregiver 1 education | College | Some college | Graduate degree |
| Caregiver 2 education | N/A | GED | GED |
Procedures
Measures
Data Analysis
Power analysis.
Cutoff scores for inclusion.
Reliable change index (RCI).
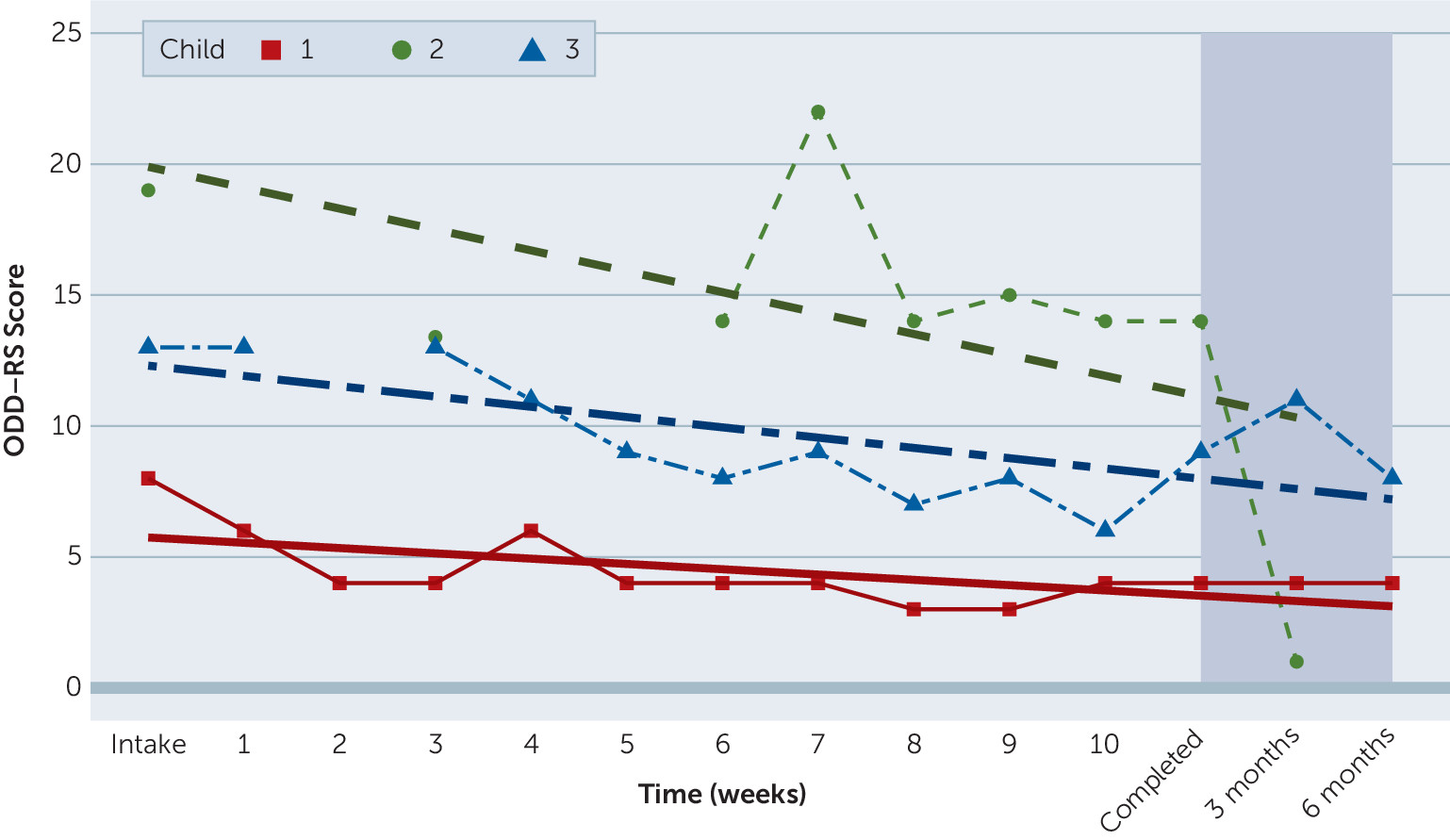
Results
Treatment Compliance
Outcomes
| Child | Intake | Completed | Difference | E Δb | Cohen’s dc | RCIc | Classification |
|---|---|---|---|---|---|---|---|
| 1 | 8 | 4 | –4 | –.5 | .79 | –1.97 | Recovered |
| 2 | 19 | 14 | –5 | .5 | .98 | –2.46 | Improved |
| 3 | 13 | 9 | –4 | –.5 | .79 | –1.97 | Improved |
| Mean | 13.33 | 9 | –4.33 | –.17 | .85 |
| Child | Scale | Intake | Completed | Difference | Cohen’s d | RCI |
|---|---|---|---|---|---|---|
| 1 | Emotion Regulation | 19 | 21 | 2 | .42 | 2.00 |
| 1 | Lability and Negativity | 31 | 31 | 0 | .00 | 0 |
| 2 | Emotion Regulation | 21 | 24 | 3 | .64 | 3.00 |
| 2 | Lability and Negativity | 33 | 30 | –3 | .64 | –7.32 |
| 3 | Emotion Regulation | 26 | 31 | 5 | 1.06 | 5.00 |
| 3 | Lability and Negativity | 34 | 26 | –8 | 1.70 | –19.51 |
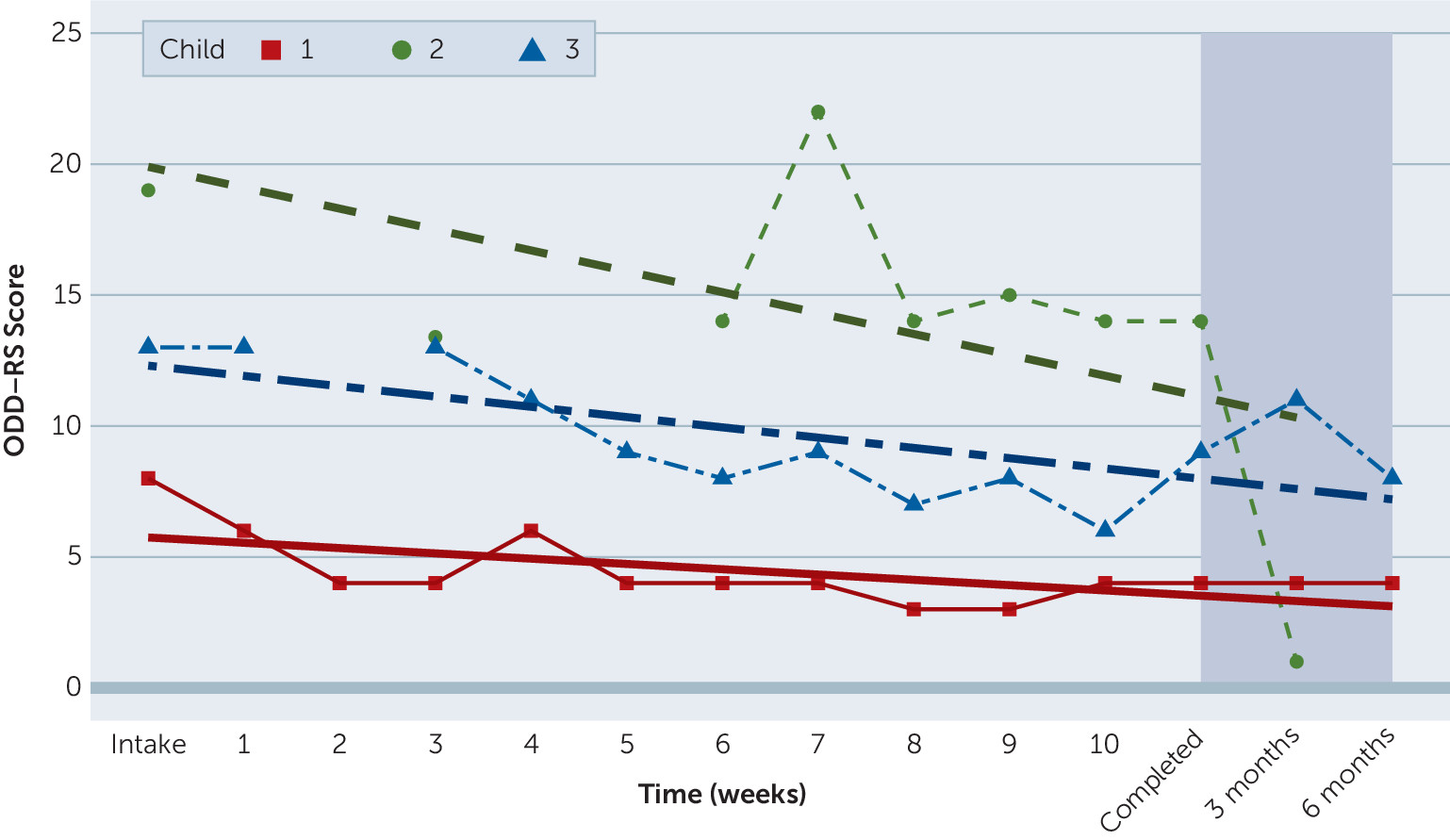
| Time point | N | Mean | SD | Range |
|---|---|---|---|---|
| Intake | 3 | 13.33 | 5.51 | 8–19 |
| End of treatment | 3 | 9.00 | 5.00 | 4–14 |
| 3-month follow-up | 3 | 5.33 | 5.13 | 1–11 |
| 6-month follow-up | 2 | 6.00 | 2.83 | 4–8 |
Parents’ Experiences of RFP-C
Discussion
Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 24.56 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBMedia
Figures