I've heard that duty hour restrictions for residents have changed again with more stringent limits being placed. This is supposed to help protect patients by having less sleep-deprived residents. But this will result in patients being transferred from one clinician to another more often and we know errors are common during handoffs. How can we make these and other types of handoffs safer?
Transfers of patient care from one physician to another, a process known as “handoffs,” are ubiquitous in health care. Prior studies report 15 resident handoffs per patient during a 5-day hospitalization (
1), and more than 4,000 handoffs per day at a single academic medical hospital (
2). Handoffs are also common in outpatient settings when, for example, the patient changes clinicians or moves between levels of care (e.g., inpatient, partial hospitalization, and outpatient), or when the clinician refers for consultation or laboratory and other tests or arranges coverage for nights, weekends, or leave (e.g., vacation, maternity).
Two recent developments have focused increased attention on handoffs: the emergence of the hospitalist field, which introduced a transfer of patient responsibility between hospital-based and primary care physicians (
3) and the restriction of resident duty hours by the Accreditation Council on Graduate Medical Education (ACGME) in 2003 followed by additional restrictions scheduled for July 2011, which has led to increased transfers due to shift changes. Handoffs are often accompanied by problems with the communication and transfer of clinical information, which can lead to medical errors and harm to patients (
4). The potential for harm during these transitions has led the Institute of Medicine to recommend (
5) and the ACGME to now require enhanced “handoffs” training for residents and The Joint Commission to mandate a standardized approach to handoff communications (
6).
Much of the research to date has focused on transitions necessitated by transfer to a different setting of care (e.g., transfer from a general ward to an ICU or discharge from the hospital) or by the end of a shift. An outpatient care transition that has received recent attention is the change in personnel that occurs on July 1, when residents either advance to a higher level of training or graduate (
7).
Although year-end handoffs in outpatient clinics resemble other types of handoffs in many regards, there are important distinguishing features. First, the year-end transfer terminates a longer-term treatment relationship, which in turn can be experienced by patients as a significant loss, leading to increased symptoms (
8). This heightened acuity makes monitoring of higher-risk patients even more critical during the transition. Second, residents stationed in continuity clinics have often accumulated relatively large panels of patients. As a result, the year-end transfer requires unique organizational processes capable of simultaneously transitioning a high volume of patients. Without such procedures in place, there is a much higher probability for patients or important clinical information to “fall through the cracks” in this type of transfer compared with other types of transfers. Third, patients are transferred from trainees with substantial experience to those with much less (outpatient) experience and skill. This experience gradient can be significant and warrant slower caseload growth, enhanced supervision, and specialized didactics.
COMMON PROBLEMS WITH HANDOFFS
Studies have documented considerable variation in the quality of handoffs. Critical incident analyses and surveys of clinicians indicate that handoffs are rarely standardized, even within a given department or institution (
9). For example, many programs do not consistently require both a written and verbal sign-out at transfer (
10). Approximately one-third of the house staff at Massachusetts General Hospital rated the overall quality of handoffs as fair or poor, with many stating that handoffs rarely or never occurred in a quiet place (43%) and were often interrupted (36%) (
11).
Although there are many potential failures in the current physician handoff processes, the majority are related to communication failures. Such failures are characterized by omissions of important medical information and/or failure-prone communication processes, both of which can lead to clinician uncertainty and medical error. The failure-prone processes include unstructured written and verbal communication, no face-to-face sign-out, poorly communicated rationale for the clinical plan (
9–
11), inadequate training of clinicians in handoffs communication, occurrence of handoffs in settings that are neither quiet, private, nor free of interruptions (
12) and the lack of infrastructure to support handoffs such as protected time for handoffs or a structured electronic written template linked to an EMR (
5).
HANDOFFS AND PATIENT HARM
Data from a variety of studies suggest that problems with handoffs do lead to medical errors and harm. In cross-sectional surveys, residents consistently report high rates of harm to patients due to problems with handoffs (
10,
11). A retrospective chart review of patients recently discharged from a large teaching hospital found that nearly half experienced at least one medical error, including errors in medication continuity, test follow-up, and workup, the latter being associated with a sixfold increase in rehospitalization within 3 months (
13). A case-control study examining adverse events in hospitalized patients found that affected patients were far more likely to have been under the care of a covering physician during the event (odds ratio of 6.1) (
14). Likewise, closed malpractice claims analysis found an association between handoff errors and missed and delayed diagnoses in the emergency department and ambulatory setting (
4,
15).
Similar findings have been reported in prospective studies. For example, one prospective study of patients admitted to a large teaching hospital found that nearly 47% of patients had omission of a regularly used medication, and 38% of these omissions were judged to have the potential to cause clinical deterioration (
16). Research in psychiatric settings is limited, with a recently published case report describing how failures in the outpatient transfer process contributed to a patient suicide (
17).
BEST PRACTICES FOR HANDOFFS
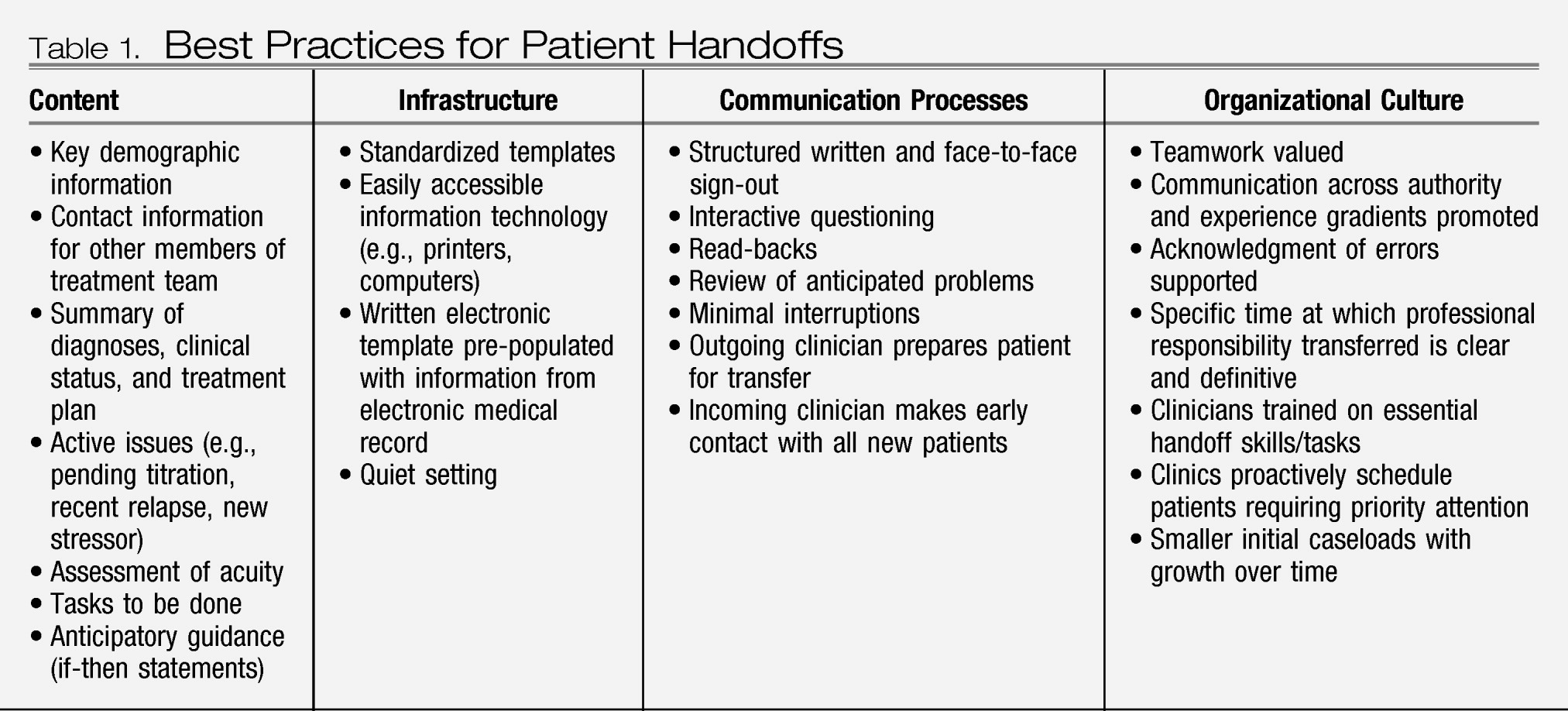
Given this degree of risk, considerable attention has been focused on interventions to improve patient safety and reduce errors during these transfers (
18,
19), many of which have been adapted from industries such as nuclear power and space aviation in which transition errors have high consequences (
20). These interventions can be organized into four categories: content, infrastructure, communication processes, and organizational culture.
Table 1 summarizes the recommended practices from the existing literature in each of these categories.
The purpose of any handoff is to establish a shared mental model about a patient in order to avoid unwarranted changes in goals, decisions, priorities, or plans. For all settings, a safe handoff includes the following features:
1.
structured written and face-to-face sign-out in an environment free of interruptions with an opportunity for clarifying questions;
2.
a reliable process by which patients with acute and/or complex illness and, therefore, at higher risk, are flagged and given priority attention; and
3.
definitive transfer of professional responsibility at a specific time.
These handoff practices have been developed primarily for inpatient settings; however, these practices are equally relevant in the outpatient setting, although they require adaptation. For example, the most appropriate strategy will depend on whether the outpatient handoff is temporary or permanent. For temporary transitions (e.g., vacation coverage), verbal sign-out may be limited to “acute” patients while a structured written document (ideally linked to an EMR) provides a snapshot of each patient. Permanent transfer require different approaches. While it is important to prepare all patients for a transfer, when an outpatient transfer involves termination of a longer-standing relationship, both the outgoing and incoming clinician should specifically address the meaning of this “loss” with the patient. In addition, the new outpatient clinician inheriting a large panel of patients, many of whom will not be seen for weeks or even months, might call or send a letter to patients to provide key contact information and begin the process of establishing a therapeutic relationship.
For trainees and, as appropriate, other clinicians, it is important to provide training that focuses on handoff-related competencies. For example, training for incoming (less experienced) residents may cover topics such as how to contextualize clinical information, prioritize tasks in the initial visits, address the loss directly with the patient, and inquire what did and did not work in the past. Outgoing (more experienced) residents may benefit from training on how to communicate effectively with new residents across an experience gradient and how to educate and prepare their patients for the transfer, including addressing the relationship loss and anticipating challenges.